125 Worth Street New York, NY 10013
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Rheumatology
NYU Langone Medical Center 550 First Avenue, New York, NY 10016 nyulmc.org RHEUMATOLOGY 2014 YEAR IN REVIEW CONTENTS 1 Letter from the Chairs 2 Facts & Figures 1 Message from the Director 4 New & Noteworthy 2 Facts & Figures 6 Section 4 New & Noteworthy 42 Research 10 Clinical Care and Research 44 Education 11 Lupus and Neonatal Lupus 13 Behçet’s Syndrome 48 Publications 14 Rheumatology and Osteoporosis 5164 LoPsoriaticcations Arthritis 18 Rheumatoid Arthritis and Osteoarthritis 55 Leadership 20 Education & Training 56 NYU Langone Medical Center Facts & Figures 24 Professional Activities 57 NYU Langone Medical Center Leadership Design: Ideas On Purpose, www.ideasonpurpose.com 27 Leadership, Locations Produced by: Office of Communications and Marketing, NYU Langone Medical Center NYU LANGONE MEDICAL CENTER / RHEUMATOLOGY / 2014 PAGE 1 MESSAGE FROM THE DIRECTOR Dear Colleagues and Friends, The tripartite mission of our division is clear: Deliver comprehensive state-of-the-art clinical care, translate and integrate medicine and science, and increase the knowledge base of our trainees. I’m proud to report that in 2014, with the dedication of all faculty members, we have made significant strides in all three areas, as evidenced in the following pages. Under the guidance of our previous division director, Steven B. Abramson, MD, now chair of the Department of Medicine, the Judith and Stewart Colton Center for Autoimmunity was established. The center aims to advance discoveries about the microbiome and its relationship to autoimmune disease, and to leverage this new knowledge to develop strategies for prevention and JILL P. BUYON, MD treatment. Our vision of a comprehensive, multidisciplinary Psoriatic Arthritis Center dedicated to the bench-to-bedside integration of dermatology and Director, Division of Rheumatology, rheumatology has now been realized, and a strong laboratory research base will Department of Medicine stand behind this center to further our understanding of psoriatic arthritis and NYU Langone Medical Center develop novel therapies. -
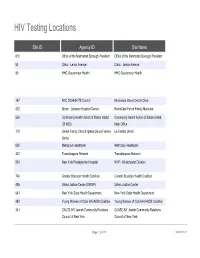
HIV Testing Locations
HIV Testing Locations Site ID Agency ID Site Name 810 Office of the Manhattan Borough President Office of the Manhattan Borough President 53 Clinic - Lenox Avenue Clinic - Lenox Avenue 90 HHC Gouverneur Health HHC Gouverneur Health 167 NYC DOHMH TB Control Morrisania Chest Center Clinic 822 Bronx - Lebanon Hospital Center BronxCare Fulton Family Medicine 524 Community Health Action of Staten Island Community Health Action of Staten Island- (CHASI) Main Office 119 United Family Church-Iglesia De La Familia La Familia Unida Unida 605 Metroplus Healthplan Metroplus Healthplan 442 Transdiaspora Network Transdiaspora Network 542 New York Presbyterian Hospital NYP - Westchester Division 746 Greater Brooklyn Health Coalition Greater Brooklyn Health Coalition 495 Urban Justice Center (SWOP) Urban Justice Center 641 New York State Health Department New York State Health Department 452 Young Women of Color HIV/AIDS Coalition Young Women of Color HIV/AIDS Coalition 341 CAUSE-NY Jewish Community Relations CAUSE-NY Jewish Community Relations Council of New York Council of New York Page 1 of 533 09/30/2021 HIV Testing Locations Hours Monday Hours Tuesday 11:00 AM - 7:00 PM 9:00 AM - 5:00 PM 8:00 AM - 8:00 PM 8:00 AM - 8:00 PM CLOSED CLOSED 9:00 AM - 5:00 PM 9:00 AM - 5:00 PM Page 2 of 533 09/30/2021 HIV Testing Locations Hours Wednesday Hours Thursday 9:00 AM - 5:00 PM 9:00 AM - 5:00 PM 8:30 AM - 5:00 PM 8:00 AM - 8:00 PM 8:30 AM - 5:00 PM 8:30 AM - 5:00 PM 9:00 AM - 5:00 PM 9:00 AM - 5:00 PM Page 3 of 533 09/30/2021 HIV Testing Locations Hours Friday -

August 9, 2021 RELIEF RESOURCES and SUPPORTIVE
September 24, 2021 RELIEF RESOURCES AND SUPPORTIVE INFORMATION1 • Health & Wellness • Housing • Workplace Support • Human Rights • Education • Bilingual and Culturally Competent Material • Beware of Scams • Volunteering • Utilities • Legal Assistance • City and State Services • Burial • Transportation • New York Forward/Reopening Guidance • Events HEALTH & WELLNESS • Financial Assistance and Coaching o COVID-19 Recovery Center : The City Comptroller has launched an online, multilingual, comprehensive guide to help New Yorkers navigate the many federal, state and city relief programs that you may qualify for. Whether you’re a tenant, homeowner, parent, small business owner, or excluded worker, this online guide offers information about a range of services and financial support. o New York City will be extending free tax assistance to help families claim their new federal child tax credit. As an investment in the long-term recovery from the pandemic, the federal American Rescue Plan made changes to the Child Tax Credit so families get half of the fully refundable credit—worth up to $3,600 per child—as monthly payments in 2021 and the other half as a part of their refund in 1 Compiled from multiple public sources 2022. Most families will automatically receive the advance payments, but 250,000+ New York City families with more than 400,000 children need to sign up with the IRS to receive the Credit. The Advance Child Tax Credits payments began on July 15, 2021 and most New Yorkers will receive their payments automatically. However, New Yorkers who have not submitted information to the IRS need to either file their taxes or enter their information with the IRS’ Child Tax Credit Non-Filer Sign-Up Tool For more information about the Advance Child Tax Credit including access to Multilingual flyer and poster—and NYC Free Tax Prep, visit nyc.gov/TaxPrep or call 311. -

HAVAA Invitation
RD AWA XILIAN AN EMENT L AU D VOLUNTEER ACHIEV ITA SP HO D AR AW T EN EM V IE H C A R E E T N U The United Hospital Fund is dedicated to creating the health care system all of us want for ourselves, our families, and our neighbors. Please consider honoring one of today’s extraordinary volunteers or auxilians, and supporting the work of the Fund, by becoming a Patron or Sponsor. This unique awards program brings public attention to the invaluable contributions of our honorees, and the other 50,000 committed volunteers in our city, who make such an important difference to patients and their families and extend the ability of New York’s hospitals to provide the best care possible. Patrons and Sponsors will be recognized in the event’s Program and all gifts will be gratefully acknowledged. Please use the enclosed reply card to indicate your level of support. Please join us for tea at the Waldorf as the United Hospital Fund honors the 2009 recipients of the # HOSPITAL AUXILIAN and VOLUNTEER ACHIEVE#MENT AWARD Friday, March 6, 2009 1:00 p.m. to 3:00 p.m The Grand Ballroom of The Waldorf-Astoria Park Avenue at 50th Street, New York City Special Guest Sade Baderinwa Co-anchor,WABC-TV Eyewitness News at 5:00 RSVP by February 10, 2009 on the enclosed card Generously underwritten by TD Bank United Hospital Fund The United Hospital Fund is a health services research and J. Barclay Collins II philanthropic organization whose Chairman mission is to shape positive change James R. -

Clinical Advisory Group (CAG) List of Participants Maternity CAG
w RK Department Medicaid ATE of Health Redesign Team Value Based Payment (VBP) Clinical Advisory Groups (CAGs) Archived List of Participants October 2016 Introduction This list represents membership for the Maternity Care, Behavioral Health, HIV/AIDS, Pulmonary, Chronic Heart Disease, Diabetes, Managed Long Term Care (MLTC), Intellectual / Developmental Disabilities (I/DD) Clinical Advisory Groups (CAGs) and the Children’s Health Subcommittee/ CAG for the measurement year (MY) 2017 quality measure annual review cycle. The current CAG membership list can be found on the VBP Resource Library. Clinical Advisory Group (CAG) List of Participants Maternity CAG Name Title Chairman of Department of Obstetrics and Gynecology Howard Minkoff, MD Maimonides Medical Center The Chella and Moise Safra Chair, Dept. of Obstetrics & Gynecology and Sharmila K Makhija MD, MBA Women’s Health, Montefiore Medical Center Maryanne F. Laffin, RN, FNP, NYSALM (NYS Association of Licensed Midwives) CNM, FACNM Faculty Advisor to the Doctorate Program at SUNY Downstate Professor and Chair of Obstetrics and Gynecology; Division Chief of Maternal Robert Silverman, MD and Fetal Medicine; Upstate University Hospital Ephraim Back, MD MPH Director, Mid-Hudson Family Practice Residency, Institute for Family Health Director of Policy & Advocacy, American Academy of Pediatrics District II (New Elie Ward, MSW York State) Executive Director, American Congress of Obstetricians and Gynecologists Donna Montalto, MPP (ACOG) , NYS Professor of Clinical Pediatrics, Albert Einstein -
The Consulting Practice a Capstone Course Moving Students from the Classroom to Industry and Back How It Works
The Consulting Practice A capstone course moving students from the classroom to industry and back how it works The Consulting Practice provides students with the opportunity to solve a strategic, policy, marketing, or operational problem for a client organization and gain experience analogous to the project-based dynamic of professional consultants. Client organizations are drawn from the spectrum of the healthcare sector, including world-renowned hospitals, pharmaceutical companies, health plans, social service nonprofits, public health organizations, and more. In this course, students serve as the consulting team on a significant project to tackle a real-world issue identified by the client—from financial modeling to assessing program readiness to designing public awareness campaigns. Consulting groups work directly with client executives under the guidance and expertise of senior faculty members with extensive business experience, who act as account managers and partners. Teams, consisting of four to six students, are expected to conduct the research, client interviews, and assessments necessary for delivering fact-based analyses and action recommendations to the client. Recent Consulting Practice Projects • Develop a manual for use by non-governmental organizations (NGOs) and international foundations to create successful and sustainable surgical programs in developing countries; • Assess the readiness of a large provider of long-term care to meet the challenges of changing New York State Medicaid requirements; • Reduce avoidable readmissions -

2016 Community Health Needs Assessment
2016 COMMUNITY HEALTH NEEDS ASSESSMENT EXECUTIVE SUMMARY Community Health Needs Assessment, 2016 Update Purpose of the Community Health Needs Assessment This 2016 Community Health Needs Assessment (CHNA) updates the CHNA completed in 2013 to meet the requirements of Section 9007 of the 2010 federal law, The Affordable Care Act (“ACA”). The ACA requires that any tax-exempt, IRS- designated 501(c) (3) hospital complete or update a publicly-available, comprehensive CHNA every three years in order to document the extent to which it understands the unique characteristics and needs of the local communities it serves, and responds to these needs by delivering meaningful and effective community benefit through clinical services and other programming. Required Components A CHNA report has five required components: 1) Definition of community served 2) A prioritized description of the significant health needs of the community 3) Transparency in the process and methods used to conduct the CHNA, including how it took into account input from the community served and prioritized community health needs 4) A description of the resources potentially available to address the identified significant prioritized community health needs 5) An evaluation of the impact of actions taken to address the significant health needs identified in the previous CHNA report (June 2013). A CHNA report is considered complete when it is adopted by a governing body of the facility and made widely available to the public. Community Served NYC Health + Hospitals serve all New Yorkers in every neighborhood in New York City regardless of their ability to pay. Addressing disparity throughout New York City, NYC Health + Hospitals is the safety-net for the uninsured and underserved in New York City. -

National Hispanic Medical Association VIRTUAL 24Th Annual Conference March 17-20, 2021 AGENDA (02.25.21) – Note All Times Are ET
National Hispanic Medical Association VIRTUAL 24th Annual Conference March 17-20, 2021 AGENDA (02.25.21) – Note All Times are ET Wednesday, March 17, 2021 7:00pm-7:45pm Opening Reception – CME - sponsored by CDC, Johnson & Johnson, Pfizer Inc Introduction of NHMA #Vaccinate4All Campaign Elena Rios, MD, MSPH, FACP President & CEO NHMA and NHHF Speakers: The Honorable Raul Ruiz U.S. Representative for California Defining Health Disparities Nicole Kulisek, MD - Senior Medical Director, Pfizer Inc Donna Judd, Ph.D - Senior Director, Pfizer Inc J&J Speaker - TBN Welcome: Nereida Correa, MD, Chairwoman, NHMA Board of Directors Mark Diaz, MD, Chairman, National Hispanic Health Foundation Board of Directors Pilar Guerrero, MD, Maria M. Garcia, MD, MPH – CoChairs, NHMA Conference Committee Pamela Montano, MD, MPH, Chairperson, NHMA Council of Young Physicians Keila Muniz, MD, Chairwoman, NHMA Council of Residents Donald Rodriguez, President, Latino Medical Student Association Lee A. Savio Beers, MD, FAAP, President of the American Academy of Pediatrics 7:45 pm-9:00 pm Networking Reception Thursday, March 18, 2021 11:30am-1:00pm OPENING PLENARY – CME Welcome & NHMA 2021 Priorities Elena Rios, MD, MSPH, FACP President & CEO National Hispanic Medical Association, Washington, DC Description: This presentation will provide a review of lessons learned from NHMA membership on COVID-19 response and program accomplishments over the past 2 years. Federal Leadership for COVID-19 and Hispanic Health Moderator: Elena Rios, MD, MSPH, FACP Marcella Nunez Smith, MD, MHS Lead of COVID-19 Health Equity Task Force White House RADM Felicia Collins, MD, MPH, FAAP - invited Acting Assistant Secretary of Health U.S. -

2016 New York State Family Planning Provider Meeting
New York State Center of Excellence for Family Planning & Reproductive Health Services Presents 2016 New York State Family Planning Provider Meeting A project of 2016 NEW YORK STATE FAMILY PLANNING PROVIDER MEETING Greetings New York State Family Planning Providers! The New York State Center of Excellence for Family Planning and Reproductive Health Services (NYS COE) and the CAI (Cicatelli Associates, Inc.) team welcomes you to Albany and the Fourth Annual New York State Family Planning Provider Meeting. This year’s meeting will explore the day-to-day challenges that low-income individuals face, and the role that family planning provider agencies – through their clinic systems – play in both contributing to obstacles as well as removing barriers to access. Limited hours of operation, not taking walk-in or same-day appointments, and long wait and cycle times all translate to logistical barriers that some clients are not able to overcome. On the flip side, strong and streamlined clinic systems can assure a positive patient experience and increase the WELCOME likelihood that a client receives needed family planning services and returns for follow-up care. This Provider Meeting will serve as a forum where family planning providers can share and consider systems-level strategies for serving and retaining low-income women, men, and adolescent clients. As the NYS COE continues to support New York State Department of Health’s family planning providers to serve individuals most in need of family planning services, its entire team is excited to see what strategies this innovative network will make use of. We also look forward to continuing to develop innovative capacity-building opportunities to support this critical work. -

The World Trade Center Environmental Health
The World Trade Center Environmental Health Center at Bellevue Hospital of the New York City Health and Hospitals Corporation (HHC) is a program to treat people with WTC-related illness. The Center, which works in partnership with community organizations and people affected by 9/11, has added two other sites: Gouverneur Healthcare Services in Lower Manhattan and Elmhurst Hospital in Queens. Bellevue Hospital Center 462 First Avenue New York, New York 10016 Gouverneur Healthcare Services 227 Madison Street New York, New York 10002 Elmhurst Hospital Center 79-01 Broadway Elmhurst, New York 11373 For information about WTC health services, or to make an appointment for treatment, call toll free 1-877-WTC-0107 (1-877-982-0107). The WTC Environmental Health Center at Bellevue, and now at Gouverneur Health Services and Elmhurst Hospital, offers treatment to people who have health problems as a result of 9/11. You can get treatment even if you can’t pay or have no insurance. You can come for treatment if, on or after 9/11, you: • Were a resident who lived in Lower Manhattan • Were a student in a school in the area • Worked in or around area offices, stores, schools, or apartment buildings • Helped in the clean-up of buildings in the affected area How would I know if my health problems are related to 9/11? It is hard to know if your health problems are due to 9/11. Some problems might include: • Shortness of breath • Stomach problems • Skin problems • Depression, anxiety, nervousness If you think you have a health problem related to 9/11, call toll free 1-877-WTC-0107. -

An Organization That Is Delegated for Credentialing
Organizations Delegated for Credentialing Delegate Name • AdvantageCare Physicians • New York - Presbyterian Queens • Albany Medical Center • New York Eye and Ear Infirmary of Mount Sinai • Allied Pediatrics • Northwell Health • American Specialty Health (ASH) • NYC Health + Hospitals - Bellevue Hospital Center • Atlas IPA/Essen Medical Associates • NYC Health + Hospitals - Coney Island Hospital Center • Balance ACO/Corinthian IPA • NYC Health + Hospitals - Elmhurst Hospital Center • Bassett Healthcare Network • NYC Health + Hospitals - Gouverneur Health Services • Beacon Health Options • NYC Health + Hospitals - Harlem Hospital Center • BronxCare Health Systems • NYC Health + Hospitals - Kings County Hospital Center (Bronx Lebanon Hospital Center) • NYC Health + Hospitals - Lincoln Medical and Mental • Brookdale Hospital Medical Center Health Center • Brooklyn Hospital Center • NYC Health + Hospitals - Metropolitan Hospital Center • Care Management Organization (CMO Montefiore) • NYC Health + Hospitals - North Bronx Healthcare • Cayuga Medical Center Network • Charles B. Wang Community Health Center • NYC Health + Hospitals - Queens Hospital Center • Coalition of Asian-American IPA (CAIPA) • NYC Health + Hospitals -Woodhull Medical and Mental • Columbia Affiliated Physicians (CAP) Health Center • ColumbiaDoctors • NYU Langone Health • Community Health Care Network • OptumHealth - Managed Transplant Program • Cornell Medical Center IPA • Palladian Health • Crystal Run Healthcare • PHCS/Multiplan • DentaQuest • ProHEALTH Physicians • eviCore -

Using a Data-Driven Organizational Improvement Model to Engage an Interdisciplinary Team in Transforming a Public Women’S Health Clinic Kenneth J
Patient Experience Journal Volume 1 | Issue 2 Article 14 2014 Using a data-driven organizational improvement model to engage an interdisciplinary team in transforming a public women’s health clinic Kenneth J. Feldman Gouverneur Health, NYC Health & Hospitals Corporation, [email protected] Molly Lopez Gouverneur Health, NYC Health & Hospitals Corporation, [email protected] Morris Gagliardi Gouverneur Health, NYC Health & Hospitals Corporation, [email protected] Follow this and additional works at: https://pxjournal.org/journal Part of the Health and Medical Administration Commons, Health Policy Commons, Health Services Administration Commons, and the Health Services Research Commons Recommended Citation Feldman, Kenneth J.; Lopez, Molly; and Gagliardi, Morris (2014) "Using a data-driven organizational improvement model to engage an interdisciplinary team in transforming a public women’s health clinic," Patient Experience Journal: Vol. 1 : Iss. 2 , Article 14. Available at: https://pxjournal.org/journal/vol1/iss2/14 This Article is brought to you for free and open access by Patient Experience Journal. It has been accepted for inclusion in Patient Experience Journal by an authorized editor of Patient Experience Journal. Using a data-driven organizational improvement model to engage an interdisciplinary team in transforming a public women’s health clinic Cover Page Footnote The uthora s acknowledge the important contributions of Lynnette Mercado, Ariel Schure, Victor Hernandez, Joanna Omi, Barbara Arline, MS, MHA, MT, Feng F. Chen, RN, Raven Carter, MBA, FACHE, Patricia Chau, MD, Maura Larkin, CNM, MSN, Jose Javier Perez, MPA, Lillian Ramos, RN, and Lleny Vargas to this work. This article is available in Patient Experience Journal: https://pxjournal.org/journal/vol1/iss2/14 Patient Experience Journal Volume 1, Issue 2 – Fall 2014, pp.