Document Version Pre-Print
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Canary Islands) by Per Sunding Botanical Garden, University of Oslo, Norway
Notes on the Flora of La Graciosa (Canary Islands) By Per Sunding Botanical Garden, University of Oslo, Norway RESUMEN Notas sobre la flora de La Graciosa (Islas Canarias): Enume- ración de 80 especies de fanerógamas, anotadas y colectadas du- rante una breve visita en dicha isla. Se considera citas florísticas poco conocidas y se presenta algunos datos sobre la vegetación en general. During field work in the eastern part of the Canary Is- lands archipelago in February-March 1969 the author made an one-day excursion to the island of Graciosa, north of Lanzarote. The flora of this 27km2 of mainly desert seems to be ~nlyscarcely known. There may well be material de- posited in various herbclria from the island, but what have bcen brought to common knowledge through publications have, so far, been only a few short plant lists or brief des- criptions of the vegetation. The first list of species from Graciosa was given by Berthelot (1836), who, however, included many doubtful cases and questionmarks. Further contributions to the flora of the island were given by Christ (1888), Bolle (1892, 1893), Pitard & Proust (1908), and Bannerman (1922). In the flora of Pitard & Proust were listed 35 species from Graciosa. The vegetation of the island is - where the landscape .S not completely devoid of plants - marked by open plant conimunities of the classes Ammophiletea and Salicornietea fruticosae (cp. Esteve Chueca 1968, and Sunding, in press). Some of the more common plant communities are the Cy- perus kalli - Euphorbia paralias comrnunity on unstable sand (the sand dune forming Traganum moquini community) and the Salsola vermiculata community on more stabilizcd sand or rocky ground. -

Pr Abdelkrim CHERITI Curriculum Vitae 1
Pr Abdelkrim CHERITI Curriculum Vitae ISSN 2170‐1768 Phytochemistry & Organic Synthesis Laboratory Family name: CHERITI First name: Abdelkrim Date & place of birth: November 25, 1963 at El – Bayadh (Algeria) Nationality: Algerian Marital status: Married (04 Childrens) Work address: Phytochemistry & Organic synthesis Laboratory, University of Bechar, 08000, Bechar, Algeria, www.posl.webs.com Phone / Fax (Works): +213 49 81 52 44 E-Mail: Karimcheriti @ yahoo.com. Actualy : Professor & Director of the Phytochemistry & Organic Synthesis Laboratory (POSL) University of Bechar, 08000, Bechar, Algeria http://www.scopus.com/authid/detail.url?authorId=27867567300 http://www.researchgate.net/profile/Cheriti_Abdelkrim Academic Qualifications • 1992: Doctorate Thesis ( PhD) in Organic Chemistry – Natural Products - , Aix- Marseille III University - ENSSPICAM, CNRS URA 1410- France « Hemisynthesis of saponins deivatives from Cholesterol and Oleanolic abd Ursolic Acids » Under supervision of Prof. A. Babadjamian ( ENSSPICAM, France). • 1987: D.E.A (Aprofunded Studies Diploma) in applied and fundamental Organic Chemistry – Fine Organic Synthesis - Aix-Marseille III University , France « Studies of SRN1 Substitution and radical reactions in heterocyclic compounds » Under supervision of Dr. M. P. Crozet (CNRS UA 109, France) • 1986: D.E.S (High Studies Diploma) in Organic Chemistry, Sidi Bél Abbès University, Algeria « IR spectral proprieties of some carbonyl compounds » Under supervision of Prof. S. Taleb ( Sidi Bel Abbes, Algeria). • 1982: Baccalaureat -

The Canary Islands
The Canary Islands Naturetrek Tour Report 6 - 13 March 2009 Indian Red Admiral – Vanessa indica vulcania Canary Islands Cranesbill – Geranium canariense Fuerteventura Sea Daisy – Nauplius sericeus Aeonium urbicum - Tenerife Euphorbia handiensis - Fuerteventura Report compiled by Tony Clarke with images by kind courtesy of Ken Bailey Naturetrek Cheriton Mill Cheriton Alresford Hampshire SO24 0NG England T: +44 (0)1962 733051 F: +44 (0)1962 736426 E: [email protected] W: www.naturetrek.co.uk Tour Report The Canary Islands Tour Leader: Tony Clarke (tour leader and naturalist) Tour Participants: Phil Haywood Hazel Haywood Peter Barrett Charles Wade Ken Bailey Day 1 Friday 6th March The arrival time of the group meant that we had enough time to do some birding in the afternoon and so we drove up from the airport, through Vilaflor to the Zona Recreativa de Las Lajas. This is probably the most well known location on Tenerife as it is where most people see their first Blue Chaffinches and we were not to be disappointed. Also at this location we saw the only Great Spotted Woodpecker of the tour plus a few Canaries, a Tenerife Kinglet and a few African Blue Tits. After departing from Las Lajas we continued climbing and entered the Las Cañadas National Park which is a spectacular drive through volcanic scenery. On the drive we encountered quite a few endemic plants including Pinus canariensis and Spartocytisus supranubius that were common and easily recognized and Echium wildpretii, Pterocephalus lasiospermus, Descurainia bourgaeana and Argyranthemum teneriffae which were rather unimpressive as they were not yet flowering but we were compensated by the fabulous views across the ancient caldera. -

EXILE, CAMPS, and CAMELS Recovery and Adaptation of Subsistence Practices and Ethnobiological Knowledge Among Sahrawi Refugees
EXILE, CAMPS, AND CAMELS Recovery and adaptation of subsistence practices and ethnobiological knowledge among Sahrawi refugees GABRIELE VOLPATO Exile, Camps, and Camels: Recovery and Adaptation of Subsistence Practices and Ethnobiological Knowledge among Sahrawi Refugees Gabriele Volpato Thesis committee Promotor Prof. Dr P. Howard Professor of Gender Studies in Agriculture, Wageningen University Honorary Professor in Biocultural Diversity and Ethnobiology, School of Anthropology and Conservation, University of Kent, UK Other members Prof. Dr J.W.M. van Dijk, Wageningen University Dr B.J. Jansen, Wageningen University Dr R. Puri, University of Kent, Canterbury, UK Prof. Dr C. Horst, The Peace Research Institute, Oslo, Norway This research was conducted under the auspices of the CERES Graduate School Exile, Camps, and Camels: Recovery and Adaptation of Subsistence Practices and Ethnobiological Knowledge among Sahrawi Refugees Gabriele Volpato Thesis submitted in fulfilment of the requirements for the degree of doctor at Wageningen University by the authority of the Rector Magnificus Prof. Dr M.J. Kropff, in the presence of the Thesis Committee appointed by the Academic Board to be defended in public on Monday 20 October 2014 at 11 a.m. in the Aula. Gabriele Volpato Exile, Camps, and Camels: Recovery and Adaptation of Subsistence Practices and Ethnobiological Knowledge among Sahrawi Refugees, 274 pages. PhD thesis, Wageningen University, Wageningen, NL (2014) With references, with summaries in Dutch and English ISBN 978-94-6257-081-8 To my mother Abstract Volpato, G. (2014). Exile, Camps, and Camels: Recovery and Adaptation of Subsistence Practices and Ethnobiological Knowledge among Sahrawi Refugees. PhD Thesis, Wageningen University, The Netherlands. With summaries in English and Dutch, 274 pp. -
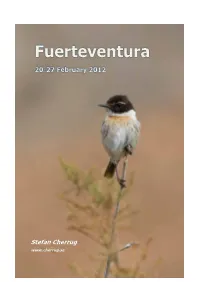
Stefan Cherrug
Stefan Cherrug www.cherrug.se Introduction I made a weeklong trip mainly for birding with my two children Alexander 20 and Nina 16. It was my third trip to the archipelago since Gran Canaria 1999, Tenerife 2011, and the fifth trip to Macaronesia after Madeira 2005 (two trips) and Kap Verde 2010. We stayed at the good hotel Geranios Suites and Spa in Caleta de Fuste just S of the airport near the sea on the middle of the east coast on Fuerteventura. It was a rather good point with reasonable easy access to most localities on the island. We travelled with Apollo and also rented a car through that agency. A little new for us was that we had to wait for bus transportation to the rental company Orlando nearby. The main targets for the trip were to see Hourbara Bustard, Canary Islands Stonechat and the endemic subspecies of the island – dacotiae of Common Kestrel, insularum of Stone-curlew, polatzeki of Lesser Short-toed Lark, degener of African Blue Tit, and harterti of Common Linnet. I had no intention to get gracilirostris of Barn Owl or canariensis of Long-eared Owl, and did not make any efforts due to lack of localities. I have in former trips seen ssp. baroli of Little Shearwater, insularum of Common Buzzard, berthelotii of Berthelot's Pipit, orbitalis of Spectacled Warbler, koenigi of Southern Grey Shrike and amantum of Trumpeter Finch, so these endemics would be the last for me to see. Great emphases were also put on photographing, me for birds and nature, my daughter and son for more touristic objects. -

A New Aulacidea Species (Hymenoptera, Cynipidae
Graellsia, 60(2): 175-184 (2004) ANEWAULACIDEA SPECIES (HYMENOPTERA, CYNIPIDAE) FROM CABO DE GATA NATURE PARK (SPAIN) INDUCING GALLS ON LAUNAEA ARBORESCENS, INCLUDING DESCRIPTION OF ITS TERMINAL INSTAR LARVA J. L. Nieves-Aldrey* ABSTRACT A new species of Aulacidea Ashmead, A. martae n. sp. (Hymenoptera, Cynipidae) is described from Cabo de Gata Nature Park (South-Eastern Spain). The new species indu- ces galls on stems of Launaea arborescens (Asteraceae) and represents the first cynipid species recorded from this plant, growing in desertic areas of south Spain. The terminal- instar larva and the gall are also described. A. martae is closely related to A. laurae Nieves-Aldrey, a species inducing galls in achenes of Podospermum laciniatum (Asteraceae). Characters separating adults, larvae and galls of both species are given and life-cycle data of the new species are provided. Key words: Aylacini, Aulacidea, herb gall-wasps, new species, Launaea, galls, Cabo de Gata, Spain. RESUMEN Una nueva especie de Aulacidea (Hymenoptera, Cynipidae) del parque natural de Cabo de Gata (España) que induce agallas en Launaea arborescens, incluyendo la descripción de su último estadio larval Se describe una nueva especie de Aulacidea Ashmead: A. martae sp. n. (Hymenop- tera, del Parque Natural de Cabo de Gata (Sureste de España). La nueva especie induce agallas en tallos de Launaea arborescens (Asteraceae) y es la primera especie de cinípi- do citada en esa planta, que crece en áreas desérticas del sureste español. Se describe también la larva madura y la agalla. A. martae es cercana a A. laurae Nieves-Aldrey, una especie que forma agallas en los aquenios de Podospermum laciniatum (Asteraceae). -

Saxicola Dacotiae
Saxicola dacotiae -- (Meade-Waldo, 1889) ANIMALIA -- CHORDATA -- AVES -- PASSERIFORMES -- MUSCICAPIDAE Common names: Fuerteventura Stonechat; Canary Chat; Canary Islands Bush Chat; Canary Islands Chat; Canary Islands Stonechat European Red List Assessment European Red List Status NT -- Near Threatened, (IUCN version 3.1) Assessment Information Year published: 2015 Date assessed: 2015-03-31 Assessor(s): BirdLife International Reviewer(s): Symes, A. Compiler(s): Ashpole, J., Burfield, I., Ieronymidou, C., Pople, R., Wheatley, H. & Wright, L. Assessment Rationale European regional assessment: Near Threatened (NT) EU27 regional assessment: Near Threatened (NT) This species, endemic to Europe and the EU27, has a moderately small population which approaches the threshold for classification as Vulnerable. It also has a very small range, which is in decline owing to ongoing habitat loss and degradation; however, its population is not severely fragmented, nor is it restricted to ten locations or fewer. For these reasons it is listed as Near Threatened in both Europe and the EU27. Occurrence Countries/Territories of Occurrence Native: Spain; Canary Is. (to ES) Population The European population is estimated at 13,400-15,500 mature individuals. The entire population is found in the EU27. For details of national estimates, see Supplementary PDF. Trend Although the estimated population exceeds the estimate provided by Bibby and Hill (1987), this is not necessarily indicative of an increase as differences in methodology mean that such estimates are difficult to compare, and the earlier study may not have properly considered detection probability (Seoane et al. 2010). Development for tourism remains a threat but its rate has probably decreased in recent years; however, overgrazing by livestock appears to be increasing and is thought to be impacting the species through habitat degradation (A. -

Ÿþa N N E X E
FACULTE DES SCIENCES DE LA NATURE ET DE LA VIE DEPARTEMENT DE BIOLOGIE THÈSE Présentée par Mme DAHANE Née ROUISSAT Lineda En vue de l’obtention du DOCTORAT EN SCIENCES BIOLOGIQUES Spécialité : Biochimie végétale appliquée. Thème : Etude des effets nématicides et molluscicides des extraits de quelques plantes sahariennes. Soutenue le : 21 Décembre 2017 Devant le jury composé de : Mr HADJADJ- AOUL Seghir, Prof. Université Oran1 ABB Président Mr BELKHODJA Moulay, Prof. UniversitéOran1, ABB Examinateur Mme BENNACEUR Malika, Prof. Université Oran1, ABB Examinatrice Mr MEKHALDI Abdelkader Prof. Université de Mostaganem, Examinateur Mr. Marouf Abderrazak. Prof. Centre. Univ. Naama Directeur de thèse Mr. Cheriti Abdelkrim Prof. Université de Béchar. Co-directeur de thèse 2016-2017 RESUME Dans le présent travail, les parties aériennes de vingt et une plantes sahariennes (21) des différentes familles botaniques (Asteraceae ; Amaranthaceae ; Rhamnaceae ; Brassicaceae ; Plumbaginaceae ; Capparidaceae ; Caryophyllaceae ; Fabaceae ; Apocynaceae ; Solanaceae ; Verbenaceae et Euphorbiacaeae) ont été utilisées pour évaluer leurs extraits aqueux (par macération ou à reflux) et les extraits organiques (acétoniques et méthanoliques avec ces fractions : hexanique, éthérique, dichlorométanolique, chloroformique, butanoliques…) pour l’activité nématicide (vis-à-vis nématodes phytoparasites à kyste : Globodera sp. et Heterodera sp. et molluscicide (vis-à-vis aux mollusques d’eau douce transporteurs des parasites : Lymnaea acumunata et Bulinus truncatus ). Les résultats sont exprimées en LC50 (taux de mortalité est égale à 50% de la population testée) par l’analyse des probits. Après l’extraction et le criblage phytochimique des extraits, l’évaluation a été réalisée sous des conditions expérimentales convenables aux cycles de vie de chaque spécimen zoologique (Température 24°C avec l’humidité et l’aération). -

On the Consumption of Launaea Arborescens Flowers by the Lizard Gallotia Atlantica in Lanzarote, Canary Islands
Viera ea 16: 233-236 ISSN 021 0-945X Junio 1986 On the consumption of Launaea arborescens flowers by the lizard Gallotia atlantica in Lanzarote, Canary Islands. M. MOLlNA- BORJA' y E. BARQUIN2 l. Departamento de Fisiología Animal. Facu ltad de Biología. Universidad de La Laguna. Tenerife. Canary Islands. Spain. 2. Departamento de Fisiología Vegetal. Facultad de Farmacia. Universidad de La Laguna. Tenerife. Canary Islands. Spain. (A ceptado el 17 de En ero de 1986) . MOLlNA-BORlA, M. & E. BARQUIN, 1986. On the consumption of Launaea arborescens nowers by the lizard Gal/otia atlantiea in Lan zarote, Canary Islands. Viera ea 16: 233-236. ABSTRACT : In this paper a part of the plant diet of Gallotia atlantica - reported as mainly insectivorous- is recorded for the second time . Some considerations are included on t he critical trophic position of the genus Gall otia and t he lack of Canarian, endemi c , strictly herbivorous land vertebrates. Key WOrdS : Gallotia, diet , herbivorous, behaviour, troph:Lc plastici ty, Canary Islands. RESL~ : En este artículo se concreta por segunda vez una parte de la dieta vegetal de Gallotia atlantica, considerada como fundamentalmente insectívora. Se hacen algunas consideraciones sobre la posición trófica crucial del género Gal lotia y la ausencia en Canarias de vertebrados terrestres endémicos, estrictamente herbívoros. Palabras clave: Gallotia, dieta, herbívoro , comportamiento, plasticidad trófica, Islas Canarias. INTRODUCTION The diet of several lacertid lizards has been shown to be varied , some species being mainly insectivorous: Lacerta vivipara (AVERY , 1966 ; I TAMIES & KOSKELA , 1971) , Podareis taurica (KABISCH , 1971) , 1:. muralis and 1:.. sicula (AVERY , 1978) , other species being omnivorous: Lacert a dugesii (SADEK , 1981). -

Evidence from an Ethnobotany Survey in Morocco Julien Blanco, Stéphanie Carrière
Sharing local ecological knowledge as a human adaptation strategy to arid environments: Evidence from an ethnobotany survey in Morocco Julien Blanco, Stéphanie Carrière To cite this version: Julien Blanco, Stéphanie Carrière. Sharing local ecological knowledge as a human adaptation strategy to arid environments: Evidence from an ethnobotany survey in Morocco. Journal of Arid Environ- ments, Elsevier, 2016, Journal of Arid Environments, 127, pp.30 - 43. 10.1016/j.jaridenv.2015.10.021. hal-01388049 HAL Id: hal-01388049 https://hal.archives-ouvertes.fr/hal-01388049 Submitted on 4 Nov 2016 HAL is a multi-disciplinary open access L’archive ouverte pluridisciplinaire HAL, est archive for the deposit and dissemination of sci- destinée au dépôt et à la diffusion de documents entific research documents, whether they are pub- scientifiques de niveau recherche, publiés ou non, lished or not. The documents may come from émanant des établissements d’enseignement et de teaching and research institutions in France or recherche français ou étrangers, des laboratoires abroad, or from public or private research centers. publics ou privés. Title: Sharing local ecological knowledge as a human adaptation strategy to arid environments: evidence from an ethnobotany survey in Morocco. Authors: Julien BLANCO a,1, Stéphanie M. CARRIERE a a IRD, UMR-220 GRED, 911, Av. Agropolis, BP 64501, 34394 Montpellier Cedex 5, France, [email protected], [email protected] 1 Corresponding author: Phone: (33) 4 67 63 69 82; Fax: (33) 4 67 63 87 78 Abstract In order to cope with uncertainty, human populations living in drylands have developed social-risk management strategies (SRMS) and own extended ecological knowledge (LEK), which contributes to their resilience and adaptive capacity. -

Population Size and Habitat Relationships of Black-Bellied Sandgrouse Pterocles Orientalis in the Canary Islands, Spain
Bird Conservation International (2010) 20:161–175. ª BirdLife International, 2009 doi:10.1017/S0959270909990207 Population size and habitat relationships of Black-bellied Sandgrouse Pterocles orientalis in the Canary Islands, Spain JAVIER SEOANE, LUIS M. CARRASCAL, DAVID PALOMINO and C. LUIS ALONSO Summary We estimated the breeding population size and assess the habitat relationships of Black-bellied Sandgrouse in the Eastern Canary Islands (Fuerteventura, Lanzarote and La Graciosa, Spain) by means of a survey based on 1,787 0.5-km line transects and distance sampling done in 2005 and 2006. The population comprised 2,906 individuals (90% CI: 2,363–3,562), which is much higher than the numbers estimated in previous reports based on partial surveys, and constitutes 20%of the total Spanish population. Sandgrouse in the Canaries are currently restricted to Fuerteven- tura, where 70% of the population gathers in four areas that encompass just 16.7 % of the island and are largely within Special Protection Areas classified under the EU Birds Directive (except the area of Tefia-Ampuyenta, first in absolute number of individuals). The environmental character- istics that maximize the probability of occurrence of the sandgrouse in Fuerteventura (probability 5 0.196) are: treeless non-cultivated areas of sandy soils without bare bedrock, with a rock cover less than 44%, located in non-coastal areas with an average terrain slope less than 27.5%, at more than 400 m from the nearest urban area, with less than 795 m of dirt roads per 20 ha, with at least 0.9% of shrub cover and a NDVI index higher than 53. -

Agroforestry Systems in Europe
Agroforestry in Europe Current Status and Future Prospects Advances in Agroforestry Volume 6 Series Editor: P.K.R. Nair School of Forest Resources and Conservation, University of Florida, Gainesville, Florida, U.S.A. Aims and Scope Agroforestry, the purposeful growing of trees and crops in interacting combinations, began to attain prominence in the late 1970s, when the international scientific community embraced its potentials in the tropics and recognized it as a practice in search of science. During the 1990s, the relevance of agroforestry for solving problems related to deterioration of family farms, increased soil erosion, surface and ground water pollution, and decreased biodiversity was recognized in the industrialized nations too. Thus, agroforestry is now receiving increasing attention as a sustainable land-management option the world over because of its ecological, economic, and social attributes. Consequently, the knowledge-base of agroforestry is being expanded at a rapid rate as illustrated by the increasing number and quality of scientific publications of various forms on different aspects of agroforestry. Making full and efficient use of this upsurge in scientific agroforestry is both a challenge and an opportunity to the agroforestry scientific community. In order to help prepare themselves better for facing the challenge and seizing the opportunity, agoroforestry scientists need access to synthesized information on multi-dimensional aspects of scientific agroforesty. The aim of this new book-series, Advances in Agroforestry, is to offer state-of-the art synthesis of research results and evaluations relating to different aspects of agroforestry. Its scope is broad enough to encompass any and all aspects of agroforestry research and development.