Health Impact of Psychosocial Hazards at Work: an Overview
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Occupational Burnout of Health Care Professionals in Hospitals
Research Article iMedPub Journals Journal of Healthcare Communications 2018 www.imedpub.com ISSN 2472-1654 Vol.3 No.3:38 DOI: 10.4172/2472-1654.100148 Occupational Burnout of Health Care Tachtsoglou K1, Lera M2, Iliadis Ch3, Frantzana A4 and Professionals in Hospitals Kourkouta L4* 1General Hospital of Thessaloniki G Genimatas, Abstract Greece Introduction: The phenomenon of occupational burnout has been the field 2General Hospital of Thessaloniki Ippokratio, of substantial research. Initially, the research has been focused on health Greece professionals, for they were considered to be the most prone employees to 3Private Diagnostic Health Center of occupational burnout. Thessaloniki, Greece 4Nursing Department, Alexander Technological Purpose: The purpose of this research paper is to investigate the health care Educational Institute of Thessaloniki, Greece professionals’ feelings and attitudes both during working and after their work. Additionally, their relationships with patients will be investigated. Material and methods: This research paper has the form of a quantitative research using questionnaires with numerically rated items. The questionnaire is one of the most popular techniques for the quantitative research. The sample of *Corresponding author: this research paper includes both nurses and doctors chosen from the workforce Kourkouta Lambrini of various hospital departments of a General Hospital in Thessaloniki. Specifically, 180 nurses and 120 doctors were surveyed. [email protected] Results: Initially, starting with the presentation of the results of our research, demographic characteristics were juxtaposed in order to clarify the sample. Professor of Nursing Department, Alexander Firstly, it is observed that a big percentage of the sample consists of women Technological Educational Institute of (66.7%), while the remaining 33.3% of men. -

Psychosocial Hazards and Occupational Stress
Psychosocial Hazards and Occupational Stress OHS Body of Knowledge Psychosocial Hazards and Occupational Stress April, 2012 Copyright notice and licence terms First published in 2012 by the Safety Institute of Australia Ltd, Tullamarine, Victoria, Australia. Bibliography. ISBN 978-0-9808743-1-0 This work is copyright and has been published by the Safety Institute of Australia Ltd ( SIA) under the auspices of HaSPA (Health and Safety Professionals Alliance). Except as may be expressly provided by law and subject to the conditions prescribed in the Copyright Act 1968 (Commonwealth of Australia), or as expressly permitted below, no part of the work may in any form or by any means (electronic, mechanical, microcopying, digital scanning, photocopying, recording or otherwise) be reproduced, stored in a retrieval system or transmitted without prior written permission of the SIA. You are free to reproduce the material for reasonable personal, or in-house, non-commercial use for the purposes of workplace health and safety as long as you attribute the work using the citation guidelines below and do not charge fees directly or indirectly for use of the material. You must not change any part of the work or remove any part of this copyright notice, licence terms and disclaimer below. A further licence will be required and may be granted by the SIA for use of the materials if you wish to: • reproduce multiple copies of the work or any part of it • charge others directly or indirectly for access to the materials • include all or part of the materials in advertising of a product or services, or in a product for sale • modify the materials in any form, or • publish the materials. -
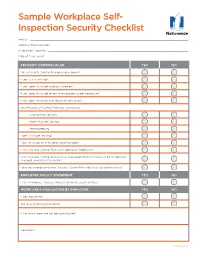
Sample Workplace Self- Inspection Security Checklist
Sample Workplace Self- Inspection Security Checklist Facility: ������������������������������������������������������������������������������������������������������������������������� Address/Work Location: �������������������������������������������������������������������������������������������������������� Assessment Done By: ����������������������������������������������������������������������������������������������������������� Date of Assessment: ������������������������������������������������������������������������������������������������������������ SECURITY CONTROL PLAN YES NO Has a Security Control Plan been developed? If yes, is it in writing? If yes, does it include a policy statement? If yes, does it include review of employee incident exposure? If yes, does it include evaluation of work areas? Identification of Control Methods considered: Engineering Controls Work Practice Controls Recordkeeping Does it include training? Does it include an evacuation and floor plan? Is the Security Control Plan accessible to all employees? Is the Security Control Plan reviews and updated when a task has been added or changed, and at least annually? Have you coordinated your Security Control Plan with local law enforcement? EMPLOYER POLICY STATEMENT YES NO Is the Workplace Violence Policy statement clearly written? WORK AREA EVALUATION BY EMPLOYER YES NO If yes, how often? Are all areas being evaluated? If no, which areas are not being evaluated? Comments: Continued >> Loss Control Services Workplace Security Checklist CONTROL MEASURES -

Mediating Role of Psychosocial Hazard: an Integrated Modelling Approach
International Journal of Environmental Research and Public Health Article Impact of Safety Culture on Safety Performance; Mediating Role of Psychosocial Hazard: An Integrated Modelling Approach Gehad Mohammed Ahmed Naji 1,*, Ahmad Shahrul Nizam Isha 1, Mysara Eissa Mohyaldinn 2, Stavroula Leka 3 , Muhammad Shoaib Saleem 1, Syed Mohamed Nasir Bin Syed Abd Rahman 4 and Mohammed Alzoraiki 5 1 Department of Management & Humanities, Universiti Teknologi PETRONAS, Seri Iskandar 32610, Perak, Malaysia; [email protected] (A.S.N.I.); [email protected] (M.S.S.) 2 Department of Petroleum Engineering, Universiti Teknologi PETRONAS, Seri Iskandar 32610, Perak, Malaysia; [email protected] 3 Cork University Business School, University College Cork, T12 K8AF Cork, Ireland; [email protected] 4 Petronas Group Technology Solutions, Bandar Baru Bangi 43000, Selangor, Malaysia; [email protected] 5 Department of Technology Management and Business, Universiti Tun Hussein Onn Malaysia, Parit Raja 86400, Johor, Malaysia; [email protected] * Correspondence: [email protected] Abstract: We conceptualize that safety culture (SC) has a positive impact on employee’s safety performance by reducing their psychosocial hazards. A higher level of safety culture environment reduces psychosocial hazards by improving employee’s performance toward safety concerns. The Citation: Naji, G.M.A.; Isha, A.S.N.; purpose of this study was to evaluate how psychosocial hazard mediates the relationship between Mohyaldinn, M.E.; Leka, S.; Saleem, safety culture and safety performance. Data were collected from 380 production employees in M.S.; Rahman, S.M.N.B.S.A.; three states of Malaysia from the upstream oil and gas sector. -
Personal Protective Equipment (PPE) Guide
Personal Protective Equipment (PPE) Guide Volume 1: General PPE February 2003 F417-207-000 This guide is designed to be used by supervisors, lead workers, managers, employers, and anyone responsible for the safety and health of employees. Employees are also encouraged to use information in this guide to analyze their own jobs, be aware of work place hazards, and take active responsibility for their own safety. Photos and graphic illustrations contained within this document were provided courtesy of the Occupational Safety and Health Administration (OSHA), Oregon OSHA, United States Coast Guard, EnviroWin Safety, Microsoft Clip Gallery (Online), and the Washington State Department of Labor and Industries. TABLE OF CONTENTS (If viewing this pdf document on the computer, you can place the cursor over the section headings below until a hand appears and then click. You can also use the Adobe Acrobat Navigation Pane to jump directly to the sections.) How To Use This Guide.......................................................................................... 4 A. Introduction.........................................................................................6 B. What you are required to do ..............................................................8 1. Do a Hazard Assessment for PPE and document it ........................................... 8 2. Select and provide appropriate PPE to your employees................................... 10 3. Provide training to your employees and document it ........................................ 11 -
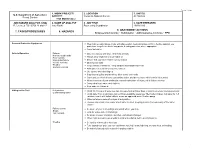
7. Tasks/Procedures 8. Hazards 9. Abatement
FS-6700-7 (11/99) 1. WORK PROJECT/ 2. LOCATION 3. UNIT(S) U.S. Department of Agriculture ACTIVITY Coconino National Forest All Districts Forest Service Trail Maintenance JOB HAZARD ANALYSIS (JHA) 4. NAME OF ANALYST 5. JOB TITLE 6. DATE PREPARED References-FSH 6709.11 and 12 Amy Racki Partnership Coordinator 10/28/2013 9. ABATEMENT ACTIONS 7. TASKS/PROCEDURES 8. HAZARDS Engineering Controls * Substitution * Administrative Controls * PPE Personal Protective Equipment Wear helmet, work gloves, boots with slip-resistant heels and soles with firm, flexible support, eye protection, long sleeve shirts, long pants, hearing protection where appropriate Carry first aid kit Vehicle Operation Fatigue Drive defensively and slow. Watch for animals Narrow, rough roads Always wear seatbelts and turn lights on Poor visibility Mechanical failure Ensure that you have reliable communication Vehicle Accients Obey speed limits Weather Keep vehicles maintained. Keep windows and windshield clean Animals on Road Anticipate careless actions by other drivers Use spotter when backing up Stay clear of gullies and trenches, drive slowly over rocks. Carry and use chock blocks, use parking brake, and do not leave vehicle while it is running Inform someone of your destination and estimated time of return, call in if plans change Carry extra food, water, and clothing Stop and rest if fatigued Hiking on the Trail Dehydration Drink 12-15 quarts of water per day, increase fluid on hotter days or during extremely strenuous activity Contaminated water Drink -
Controlling Hazardous Energy: De-Energization and Lockout Iii Trapped-Key Interlock Systems
Controlling Hazardous Energy De-Energization and Lockout About WorkSafeBC At WorkSafeBC, we’re dedicated to promoting safe and healthy workplaces across B.C. We partner with workers and employers to save lives and prevent injury, disease, and disability. When work-related injuries or diseases occur, we provide compensation and support injured workers in their recovery, rehabilitation, and safe return to work. We also provide no-fault insurance and work diligently to sustain our workers’ compensation system for today and future generations. We’re honoured to serve the workers and employers in our province. Prevention Information Line We provide information and assistance with health and safety issues in the workplace. Call the information line 24 hours a day, 7 days a week to report unsafe working conditions, a serious incident, or a major chemical release. Your call can be made anonymously. We can provide assistance in almost any language. If you have questions about workplace health and safety or the Occupational Health and Safety Regulation, call during our office hours (8:05 a.m. to 4:30 p.m.) to speak to a WorkSafeBC officer. If you’re in the Lower Mainland, call 604.276.3100. Elsewhere in Canada, call toll-free at 1.888.621.7233 (621.SAFE). Health and safety resources You can find our health and safety resources on worksafebc.com, and many of them can be ordered from the WorkSafeBC Store at worksafebcstore.com. In addition to books, you’ll find other types of resources at the WorkSafeBC Store, including DVDs, posters, and brochures. If you have any questions about placing an order online, please contact a customer service representative at 604.232.9704 or toll-free at 1.866.319.9704. -

Philippine Independence Day Issue
P Philippine Independence Day Issue Editor’s Notes: ………………………… “Happy Independence Day, Philippines!” ……………………. Eddie Zamora Featured Items: 1. Philippine Independence Day, A Brief History ……………………………………………………………………….. The Editor 2. I Am Proud To Be A Filipino ……………………………………………………………………….. by Nelson Lagos Ornopia, Sr. 3. Presidents Of The Philippines ……………………………………………………………..………………………………. Group Effort 4. The Philippine Flag and Its Symbols ……………………………………………………………………………………. The Internet 5. The Philippine National Anthem …………………………………………………………………………………………………………….. SULADS Corner: …………………………..………………… “Sulads Is Like A Rose” ………………… by Crisophel Abayan. NEMM Patch of Weeds: …………………………………………………………………………….……………………………..………….. Jesse Colegado LIFE of a Missionary: ………………… “President of SDA Church Visits ‘Land Eternal’”………..………. Romulo M. Halasan CLOSING: Announcements |From The Mail Bag| Prayer Requests | Acknowledgements Meet The Editors |Closing Thoughts | Miscellaneous Happy Independence Day, Philippines! very June 12 the Philippines celebrates its Independence Day. Having lived in America some 30 E years now I am familiar with how people celebrate Independence here—they have parades, barbecues and in the evening fireworks. When we left the Philippines years ago fireworks were banned in the country. I don’t know how it is today. It would be wonderful if Filipinos celebrated Independence Day similar to or better than the usual parades, picnics, barbecues and some fireworks. When I was a kid growing up, Independence Day was observed on July 4th, the day when the United States granted the country independence from American rule. The American flag was finally lowered from government building flagpoles and the Philippine flag was hoisted in its stead. From that day until one day in 1962 the country celebrated Independence Day on the same day the United States celebrated its own Independence Day. But on May 12, 1962 then President Diosdado Macapagal issued Presidential Proclamation No. -

Occupational Burnout School of Medicine for International Students, I-Shou University, No
ISSN: 2455-5479 DOI: https://dx.doi.org/10.17352/acmph MEDICAL GROUP Received: 30 March, 2020 Mini Review Accepted: 10 April, 2020 Published: 11 April, 2020 *Corresponding author: Tzu-Ching Sung, MS, PhD, Occupational burnout School of Medicine for International Students, I-Shou University, No. 8, Yida Rd., Jiaosu Village, Yanchao Tzu-Ching Sung* District, Kaohsiung City 82445, Taiwan, Tel: 886-7- 615-1100 ext.7971; E-mail: School of Medicine for International Students, College of Medicine, I-Shou University, Kaohsiung, Taiwan https://www.peertechz.com During the 1960s, the term “burnout” originated as an response to incapability to cope with workplace demands), explanation of the effect on an individual who struggled with depersonalization (attitudes and behaviors marked by apathy, substance use disorder [1]. Burnout was fi rst identifi ed as a coldness, distance, indifference, cynicism and detachment potential cause of attrition in various fi elds by Freudenberger from the job), and decreased personal accomplishment at work in 1974 [2]. Since 1974, many scientifi c studies on this mental (a sense of ineffectiveness and poorer performance or feelings circumstance have been published. Freudenberger defi ned of not reaching achievement at work, and intense desires to burnout as an individual who were exhausted by extreme change jobs) [6-8]. The most extensively used instrument demands on energy, capitals, or strength that would lead them to measure burnout syndrome is Maslach Burnout Inventory to become ineffective in achieving the intents and purposes (MBI) that has been categorized into three types of Maslach [3]. Numerous published studies on this mental condition cited Burnout Inventory-Educators Survey (MBI-ES), Maslach Freudenberger as the fi rst to describe burnout [4]. -

Burnout Syndrome in Europe: Towards a Harmonized Approach in Occupational Health Practice and Research
Industrial Health 2019, 57, 745–752 Research Strategy Burnout syndrome in Europe: towards a harmonized approach in occupational health practice and research Irina GUSEVA CANU1*, Olivia MESOT1, Christina GYÖRKÖS1, Zakia MEDIOUNI1, Ingrid Sivesind MEHLUM2 and Merete Drevvatne BUGGE2 1Center for primary care and public health (Unisanté), University of Lausanne, Switzerland 2National Institute of Occupational Health (STAMI), Norway Received August 25, 2018 and accepted January 29, 2019 Published online in J-STAGE February 27, 2019 Abstract: Health practitioners and decision makers in the medical and insurance systems need knowledge on the work-relatedness of burnout. To gather the most reliable information regarding burnout diagnosis and recognition in Europe, we used an 8-item standard questionnaire sent by e-mail to occupational health specialists identified via the Network on the Coordination and Har- monization of European Occupational Cohorts (OMEGA-NET) within the European Cooperation in Science and Technology (COST) Action. Participation rate was 100%, and the questionnaire was completed for 37 countries. In 14 (38%) countries burnout syndrome can be acknowledged as an occupational disease. However, only one country included burnout on the list of occupational diseases. The results showed a high variability in burnout diagnosis, in assessment of its work- relatedness, and in conditions allowing compensation of patients. These results reflect a lack of graded evidence on burnout and its determinants. The ongoing research on burnout conducted in the frame of the OMEGA-NET COST Action should be helpful through facilitating standardization of both existing and new data on burnout, a priority outcome requiring harmonization. Key words: Burnout, Diagnosis, Epidemiology, Harmonization, Occupation, Work-relatedness defined by means of the dimensions of exhaustion, cynicism Introduction and lack of efficacy from the “Maslach Burnout Inventory- General Survey” (MBI-GS)4). -

1/11/2006 Health in an Unequal World Michael Marmot This Is a Lightly
1/11/2006 Health in an Unequal World Michael Marmot This is a lightly edited version of the (October) 2006 Harveian Oration at the Royal College of Physicians. It will be published in Clinical Medicine and the Lancet. In poor countries, tragically, people die unnecessarily. In rich countries, too, the higher death rate of those in less fortunate social positions is unnecessary. Can there be a link between these two phenomena: inequalities in health among countries and inequalities within? Surely, it might be argued, the depredations of grinding poverty – lack of food, shelter, clean water, and basic medical care or public health – that ravage the lives of the poor in developing countries are different in kind from the way that social disadvantage leads to poor health in modern Britain, for example. The diseases of the slums of Nairobi are, to be sure, different in kind from the diseases that affect the disadvantaged in east London or Harlem, and have different proximate causes. There is, however, a link. The unnecessary disease and suffering of the disadvantaged, whether in poor countries or rich, is a result of the way we organise our affairs in society. I shall argue, in this oration, that failing to meet the fundamental human need of autonomy, empowerment, or human freedom is a potent cause of ill-health. In making this case, I shall bring together two rather disparate streams of work. The first is a report of my own research endeavour. I have sought explanations for the social gradient in health, as observed in the Whitehall studies, pointing to the fundamental importance of the circumstances in which people live and work. -

Obesity and Overweight in Relation to Mortality in Men with and Without Type 2 Diabetes/Impaired Glucose Tolerance the Original Whitehall Study
Cardiovascular and Metabolic Risk BRIEF REPORT Obesity and Overweight in Relation to Mortality in Men With and Without Type 2 Diabetes/Impaired Glucose Tolerance The original Whitehall Study 1 2 G. DAVID BATTY, PHD MICHAEL G. MARMOT, FRCP IGT (n ϭ 1,030) and in those with type 2 2 2 MIKA KIVIMAKI, PHD MARTIN J. SHIPLEY, MSC diabetes (n ϭ 195) was very similar. That 3 GEORGE DAVEY SMITH, MD is, there was no suggestion that the all- cause weight-mortality relation differed between the IGT (hazard ratio [HR] per n studies of apparently healthy individ- ernment employees aged 40–69 years increase in weight category 1.12 [95% CI uals, overweight and obesity, typically when examined between 1967 and 1970, 1.00–1.25]) and diabetes group (1.19 I assessed using BMI, have been consis- representing a 74% response (22). Height [0.94–1.49], P ϭ 0.64 for difference in tently associated with an increased risk of and weight were measured using stan- gradient between groups). Similar results all-cause mortality, cardiovascular dis- dard protocols, and BMI was computed were apparent when CVD was the out- ease (CVD), and select cancers (1–4). (weight [kg]/height2 [m2]) and catego- come of interest (P ϭ 0.98). Therefore, we However, extrapolating these results to rized according to current guidelines combined the IGT and type 2 diabetes individuals with type 2 diabetes is com- (23): normal weight (18.5 to Ͻ25.0), groups, an approach we have taken else- plex and perhaps inappropriate. Studies over weight (25.0–29.99), and obesity where (26).