Facilitators and Barriers in the Humanization of Childbirth Practice in Japan
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

The Effect of Premarital Pregnancy on Second Childbearing in Japan
DEMOGRAPHIC RESEARCH VOLUME 39, ARTICLE 48, PAGES 1305,1330 PUBLISHED 19 DECEMBER 2018 https://www.demographic-research.org/Volumes/Vol39/48/ DOI: 10.4054/DemRes.2018.39.48 Research Article Order matters: The effect of premarital pregnancy on second childbearing in Japan Fumiya Uchikoshi Ryohei Mogi © 2018 Fumiya Uchikoshi & Ryohei Mogi. This open-access work is published under the terms of the Creative Commons Attribution 3.0 Germany (CC BY 3.0 DE), which permits use, reproduction, and distribution in any medium, provided the original author(s) and source are given credit. See https://creativecommons.org/licenses/by/3.0/de/legalcode. Contents 1 Introduction 1306 2 Background 1307 2.1 Recent increase in premarital pregnancy in Japan 1307 2.2 Negative association between premarital pregnancy and second 1309 childbearing 2.3 Positive association between premarital pregnancy and second 1310 childbearing 2.4 Null association between premarital pregnancy and second 1311 childbearing 2.5 Selective mechanisms of premarital pregnancy 1311 3 Data and methods 1312 3.1 Data 1312 3.2 Methods 1315 4 Results 1316 4.1 Results of propensity score matching 1316 4.2 Descriptive analysis 1318 4.3 Results of discrete time logistic model 1320 5 Conclusion 1322 6 Acknowledgments 1324 References 1326 Demographic Research: Volume 39, Article 48 Research Article Order matters: The effect of premarital pregnancy on second childbearing in Japan Fumiya Uchikoshi1 Ryohei Mogi2 Abstract BACKGROUND Although nonmarital childbearing is uncommon in Japan, in contrast to the trends observed in other countries, the number of premarital pregnancies has increased. While prior studies have examined the determinants of premarital pregnancy, little is known about its consequence on individuals’ subsequent childbearing. -

Polycystic Ovarian Syndrome June 07-08, 2018 | London, UK
Day 1 & Abstracts Tracks Scientific 4 th World Congress on Polycystic Ovarian Syndrome June 07-08, 2018 | London, UK Page 17 PCOS 2018 Sessions PCOS and Pregnancy | Prevention and Management of PCOS | Effects of PCOS on Women’s Health | Long-Term Effects of PCOS | Day 1 PCOS and Obesity June 07, 2018 Session Chair Session Co-Chair George B. Kudolo M A Hasanat UT Health San Antonio, USA Bangabandhu Sheikh Mujib Medical University (BSMMU), Bangladesh Session Introduction Title: Effect of exposure to second-hand smoke from husbands on sex hormones, metabolic profiles, clinical phenotypes and pregnancy outcomes in women with polycystic ovary syndrome undergoing ovulation induction Ronald Wang, The Chinese University of Hong Kong, Hong Kong Title: Relationship between variants of menstrual disturbance and insulin resistance in patients with polycystic ovary syndrome in Bangladesh Naresh Parajuli, Bangabandhu Sheikh Mujib Medical University (BSMMU), Bangladesh Title: Management for women with PCOS prior to desiring pregnancy Nobuhiko Suganuma, Kyoto University Graduate School of Medicine, Japan Title: Prepregnancy phenotype and physiological characteristics in PCOS Tendai M. Chiware, University of Vermont Larner College of Medicine, USA Title: Insulin resistance and metabolic syndrome among different phenotypes of women with polycystic ovary syndrome Hurjahan Banu, Bangabandhu Sheikh Mujib Medical University (BSMMU), Bangladesh Title: The critical role of p66shc oxidative stress pathway in hyperandrogen-induced ovarian fibrosis Yong Wang, Nanjing -

Effectiveness of a Breastfeeding Program for Mothers Returning to Work in Japan: a Quasi-Experimental Study Kaori Nakada
Nakada International Breastfeeding Journal (2021) 16:6 https://doi.org/10.1186/s13006-020-00351-3 RESEARCH Open Access Effectiveness of a breastfeeding program for mothers returning to work in Japan: a quasi-experimental study Kaori Nakada Abstract Background: Maternal employment has been described as a barrier to breastfeeding in many countries. In Japan, many mothers quit breastfeeding after returning to work because they do not know how to continue breastfeeding. The primary objective of this study was to investigate the effectiveness of a breastfeeding support program for mothers. The secondary objective was to explore the effectiveness of a pamphlet for mothers returning to work. Methods: This was a quasi-experimental design study with a program group (n = 48), pamphlet group (n = 46) and comparison group (n = 47) that took place from February 2017 to August 2018. Participants in the program and pamphlet groups were women who planned to return to work within 4–12 months after giving birth, while the comparison group included women who had been back at work for at least 3 months. The program involved a 90- min breastfeeding class, a pamphlet, a newsletter, and email consultation. The pamphlet group was sent only the pamphlet, while the comparison group received no intervention. The outcome was breastfeeding continuation rate at 3 months after returning to work. Results: The breastfeeding continuation rate 3 months after returning to work was significantly higher in the program group than in the comparison group (79.2% vs. 51.1%, p = 0.004). After adjusting for background factors, the program intervention had an effect on breastfeeding rates (adjusted odds ratio = 4.68, 95% confidence interval: 1.57, 13.96; p = 0.006). -

Childbearing in Japanese Society: Traditional Beliefs and Contemporary Practices
Childbearing in Japanese Society: Traditional Beliefs and Contemporary Practices by Gunnella Thorgeirsdottir A thesis submitted in partial fulfilment of the requirements for the degree of Doctor of Philosophy The University of Sheffield Faculty of Social Sciences School of East Asian Studies August 2014 ii iii iv Abstract In recent years there has been an oft-held assumption as to the decline of traditions as well as folk belief amidst the technological modern age. The current thesis seeks to bring to light the various rituals, traditions and beliefs surrounding pregnancy in Japanese society, arguing that, although changed, they are still very much alive and a large part of the pregnancy experience. Current perception and ideas were gathered through a series of in depth interviews with 31 Japanese females of varying ages and socio-cultural backgrounds. These current perceptions were then compared to and contrasted with historical data of a folkloristic nature, seeking to highlight developments and seek out continuities. This was done within the theoretical framework of the liminal nature of that which is betwixt and between as set forth by Victor Turner, as well as theories set forth by Mary Douglas and her ideas of the polluting element of the liminal. It quickly became obvious that the beliefs were still strong having though developed from a person-to- person communication and into a set of knowledge aquired by the mother largely from books, magazines and or offline. v vi Acknowledgements This thesis would never have been written had it not been for the endless assistance, patience and good will of a good number of people. -

The Current State of Professional Midwives in Japan and Their Traditional Virtues
WOMEN’S HEALTH ISSN 2380-3940 http://dx.doi.org/10.17140/WHOJ-2-114 Open Journal Opinion The Current State of Professional Midwives *Corresponding author in Japan and their Traditional Virtues Masafumi Koshiyama, MD, PhD Professor Department of Women’s Health Graduate School of Human Nursing Masafumi Koshiyama, MD, PhD*; Yumiko Watanabe, CNM; Natsuko Motooka, CNM; The University of Shiga Prefecture Haruko Horiuchi, CNM 2500 Hassakacho, Hikone Shiga 522-8533, Japan Tel. +81-749-28-8664 Department of Women’s Health, Graduate School of Human Nursing, The University of Fax: +81-749-28-9532 Shiga Prefecture, 2500 Hassakacho, Hikone, Shiga 522-8533, Japan E-mail: [email protected] Volume 2 : Issue 1 ABSTRACT Article Ref. #: 1000WHOJ2114 Traditionally, Japanese women endure labor pain. They are then pleased by the sense of ac- Article History complishment after a successful vaginal childbirth, a concept based on the Japanese Buddhism. Received: June 2nd, 2016 Therefore, Japanese midwives place importance on the process and devote care for pregnant Accepted: June 15th, 2016 women throughout the experience. Professional midwives in Japan strive to monitor the child- Published: June 16th, 2016 birth process with devotion and identify any abnormality with modern scientific knowledge in the small midwifery rooms of hospitals and clinics, in cooperation with obstetricians. Recently a new midwifery category has evolved called “advanced midwife” that do not work under a Citation physician’s direct supervision, but rather practice independently and in harmony with the doc- Koshiyama M, Watanabe Y, Moto- tors. oka N, Horiuchi H. The current state of professional midwives in Japan and their traditional virtues. -
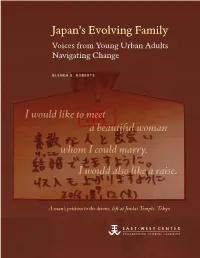
Japan's Evolving Family
Japan’s Evolving Family: Voices from Young Urban Adults Navigating Change Navigating Adults Urban Young from Voices Family: Evolving Japan’s Japan’s Evolving Family Voices from Young Urban Adults Navigating Change GLENDA S. ROBERTS I would like to meet a beautiful woman whom I could marry. I would also like a raise. A man’s petition to the divine, left at Jindai Temple, Tokyo Roberts East-West Center East-West Japan’s Evolving Family: Voices from Young Urban Adults Navigating Change GLENDA S. ROBERTS The East-West Center promotes better relations and understanding among the people and nations of the United States, Asia, and the Pacific through cooperative study, research, and dialogue. Established by the US Congress in 1960, the Center serves as a resource for information and analysis on critical issues of common concern, bringing people together to exchange views, build expertise, and develop policy options. The Center’s 21-acre Honolulu campus, adjacent to the University of Hawai‘i at Mānoa, is located midway between Asia and the US mainland and features research, residential, and international conference facilities. The Center’s Washington, DC, office focuses on preparing the United States for an era of growing Asia Pacific prominence. EastWestCenter.org Print copies are available from Amazon.com. Single copies of most titles can be downloaded from the East-West Center website, at EastWestCenter.org. For information, please contact: Publications Office East-West Center 1601 East-West Road Honolulu, Hawai‘i 96848-1601 Tel: 808.944.7145 Fax: 808.944.7376 [email protected] EastWestCenter.org/Publications ISBN 978-0-86638-274-8 (print) and 978-0-86638-275-5 (electronic) © 2016 East-West Center Japan’s Evolving Family: Voices from Young Urban Adults Navigating Change Glenda S. -

Perception of Childbirth Experiences of Japanese Women in Bali, Indonesia: a Qualitative Study
Perception of childbirth experiences of Japanese women in Bali, Indonesia: A qualitative study Kazuko Tanaka ( [email protected] ) Yamaguchi Kenritsu Daigaku Kango Eiyo Gakubu https://orcid.org/0000-0002-8292-4930 Ni Made Dian Kurniasari Universitas Udayana Kampus Surdiman Desak Nyoman Widyanthini Universitas Udayana Kampus Surdiman Ni Luh Putu Suariyani Universitas Udayana Kampus Surdiman Rina Listyowati Universitas Udayana Kampus Surdiman Akimi Urayama Yamaguchi Kenritsu Daigaku I Made Ady Wirawan Universitas Udayana Kampus Surdiman Koichi Yoshimura Yamaguchi Kenritsu Daigaku Research article Keywords: childbirth experiences, Japanese, pregnant women, Bali Indonesia, midwifery, qualitative study, woman-centred care Posted Date: December 8th, 2020 DOI: https://doi.org/10.21203/rs.3.rs-30084/v3 License: This work is licensed under a Creative Commons Attribution 4.0 International License. Read Full License Version of Record: A version of this preprint was published on December 7th, 2020. See the published version at https://doi.org/10.1186/s12884-020-03466-x. Page 1/17 Abstract Background: Maternal healthcare services in Indonesia have seen dramatic improvements over the past 25 years and yet there is still room for improvement. The perception, by the women, of the perinatal care provided, is a vital input to further improving these services. This study examines how the perinatal care provided is experienced by Japanese women in Bali, using an interview survey. Methods: We conducted semi-structured interviews, from August to October 2017, with 14 Japanese women living in Badung Regency and Denpasar City in Bali Province, Indonesia to report their perception of the perinatal care they experienced during their pregnancies. -

Daughter of Time: the Postmodern Midwife1 Robbie Davis-Floyd
Daughter of Time: The Postmodern Midwife1 Robbie Davis-Floyd For past millennia, midwives have served women in childbirth. In premodern times, midwives were usually the only birth attendants. With the Industrial Revolution and the arrival of modernism, male physicians either replaced midwives or superceded them in the modernist medical hierarchy, leaving them with plenty of women to attend but with relatively little autonomy. As the new millennium dawns on a growing worldwide biomedical hegemony over birth, midwives, the daughters of time and tradition, find themselves negotiating their identities, searching for appropriate roles, and seeking new rationales for their continued existence. “Modernity” is a narrow canal through which the vast majority of contemporary cultures have passed or are passing. It arrived in various parts of the world at different times; first in the industrializing countries of the North, and more slowly in the colonized and exploited countries of the South. So anthropologists consider “modernism” not to be a particular point in time but rather a univariate (single- pointed, single-minded, unvarying) orientation toward “progress,” defined in terms of Westernized forms of education, technologization, infrastructural development (highway, rail, water, and air systems etc.), factory production, economic growth, and the development of the global marketplace. This univariate orientation identifies a single point in a given area toward which development should be progressing: in economics, that single point is capitalism; in health care, it is Western biomedicine. Thus in modernizing societies traditional systems of healing, including midwifery, have become increasingly regarded by members of the growing middle and upper classes as “premodern vestiges” of a more backward time that must necessarily vanish as modernization/biomedicalization progresses. -

Development and Evaluation of a Self Care Program on Breastfeeding in Japan: a Quasi-Experimental Study Masayo Awano1*, Keiko Shimada2
Awano and Shimada International Breastfeeding Journal 2010, 5:9 http://www.internationalbreastfeedingjournal.com/content/5/1/9 RESEARCH Open Access Development and evaluation of a self care program on breastfeeding in Japan: A quasi-experimental study Masayo Awano1*, Keiko Shimada2 Abstract Background: Although the importance of breastfeeding is well known in Japan, in recent years less than 50% of mothers were fully breastfeeding at one month after birth. The purpose of this study was to develop a self-care program for breastfeeding aimed at increasing mothers’ breastfeeding confidence and to evaluate its effectiveness. Methods: A quasi-experimental pretest-posttest design was conducted in Japan. The intervention, a breastfeeding self-care program, was created to improve mothers’ self-efficacy for breastfeeding. This Breastfeeding Self-Care Program included: information on the advantages and basics of breastfeeding, a breastfeeding checklist to evaluate breastfeeding by mothers and midwives, and a pamphlet and audiovisual materials on breastfeeding. Mothers received this program during their postpartum hospital stay. A convenience sample of 117 primiparous women was recruited at two clinical sites from October 2007 to March 2008. The intervention group (n = 55), who gave birth in three odd-numbered months, received standard care and the Breastfeeding Self-Care Program while the control group (n = 62) gave birth in three even numbered months and received standard breastfeeding care. To evaluate the effectiveness of the Breastfeeding Self-Care Program, breastfeeding self-efficacy and breastfeeding rate were measured early postpartum, before the intervention, and after the intervention at one month postpar- tum. The study used the Japanese version of The Breastfeeding Self-Efficacy Scale Short Form (BSES-SF) to measure self-efficacy. -

Japan's Employment 'Catch-22': the Impact of Working Conditions for Women in Japan on Japan's Demographic Popula
The University of San Francisco USF Scholarship: a digital repository @ Gleeson Library | Geschke Center Master's Theses Theses, Dissertations, Capstones and Projects Winter 12-15-2017 Japan's Employment 'Catch-22': The mpI act of Working Conditions for Women in Japan on Japan's Demographic Population Crisis Mary Perkins [email protected] Follow this and additional works at: https://repository.usfca.edu/thes Part of the Asian American Studies Commons, Asian Studies Commons, Economic Policy Commons, Education Policy Commons, Infrastructure Commons, Japanese Studies Commons, Other Feminist, Gender, and Sexuality Studies Commons, Other International and Area Studies Commons, Other Public Affairs, Public Policy and Public Administration Commons, and the Women's Studies Commons Recommended Citation Perkins, Mary, "Japan's Employment 'Catch-22': The mpI act of Working Conditions for Women in Japan on Japan's Demographic Population Crisis" (2017). Master's Theses. 260. https://repository.usfca.edu/thes/260 This Thesis is brought to you for free and open access by the Theses, Dissertations, Capstones and Projects at USF Scholarship: a digital repository @ Gleeson Library | Geschke Center. It has been accepted for inclusion in Master's Theses by an authorized administrator of USF Scholarship: a digital repository @ Gleeson Library | Geschke Center. For more information, please contact [email protected]. TABLE OF CONTENTS 1. Acronyms, Terms, & Definitions ………………………………………………………. 2 2. Figures ………………………………………………………………………………….. 3 3. Abstract & Keywords ...……………………………………………………………….... 4 4. Introduction …………………………………………………………………………….. 5 Thesis Causative Trends Background 5. Literature Review ……………………………………………………………..……….. 10 Japan’s Aging Population Japanese Workplace Policies and Culture Japanese Feminism and Sexism Gaps in Literature 6. Methodology ………………………………………………………………..…………. 22 7. Findings ………………………………………………………………………………... 30 7.1 ‘Graying’ of Japan’s Population 7.2 Women Barriers 7.3 Lack of Births, aging society 8. -
Japan Federation of Bar Associations Report of JFBA Regarding the Third
JFBA/17/13 March 11, 2013 Japan Federation of Bar Associations Japan Federation of Bar Associations Report of JFBA Regarding the Third Periodic Report by the Government of Japan under Articles 16 and 17 of the International Covenant on Economic, Social and Cultural Rights January 18, 2013 JAPAN FEDERATION OF BAR ASSOCIATIONS 1-3, KASUMIGASEKI 1-CHOME, CHIYODA-KU, TOKYO 100-0013 JAPAN TEL: +81 3 3580 9741 FAX: +81 3 3580 9840 Email: [email protected] URL: www.nichibenren.or.jp 1 Contents Foreword ........................................................................................................................................... 5 Discussion by Article of the Covenant .............................................................................................. 6 Article 1 - Right of Self-Determination ............................................................................... 6 A. The Ainu ...................................................................................................................... 6 B. Okinawan Issues .......................................................................................................... 7 Article 2 - Treaty Entrenchment and Non-Discrimination ................................................ 9 A. Legal Characteristics of the Covenant and its Functions ............................................... 9 B. The Principle of Prohibition on the Retrogressive Measures ........................................ 10 C. Teaching and Training Programs on Human Rights ................................................... -

Childbirth Across Cultures Science Across Cultures: the History of Non-Western Science
CHILDBIRTH ACROSS CULTURES SCIENCE ACROSS CULTURES: THE HISTORY OF NON-WESTERN SCIENCE VOLUME 5 CHILDBIRTH ACROSS CULTURES Editor HELAINE SELIN, Hampshire College, Amherst, MA, USA For further volumes: http://www.springer.com/series/6504 CHILDBIRTH ACROSS CULTURES Ideas and Practices of Pregnancy, Childbirth and the Postpartum Editor HELAINE SELIN Hampshire College, Amherst, MA, USA Co-Editor PAMELA K. STONE Hampshire College, Amherst, MA, USA 123 Editor Co-Editor Helaine Selin Pamela Kendall Stone School of Natural Science School of Natural Science Hampshire College Hampshire College Amherst MA 01002 Amherst MA 01002 USA USA [email protected] [email protected] ISSN 1568-2145 ISBN 978-90-481-2598-2 e-ISBN 978-90-481-2599-9 DOI 10.1007/978-90-481-2599-9 Springer Dordrecht Heidelberg London New York Library of Congress Control Number: 2009926833 © Springer Science+Business Media B.V. 2009 No part of this work may be reproduced, stored in a retrieval system, or transmitted in any form or by any means, electronic, mechanical, photocopying, microfilming, recording or otherwise, without written permission from the Publisher, with the exception of any material supplied specifically for the purpose of being entered and executed on a computer system, for exclusive use by the purchaser of the work. Printed on acid-free paper Springer is part of Springer Science+Business Media (www.springer.com) To my children. And especially to my granddaughter, Enna Rae Selina Sherwin, born 5th August, 2009. Contents Contributors ................................. ix Introduction by H. Selin ........................... xiii Birth and the Big Bad Wolf: An Evolutionary Perspective ........ 1 Robbie Davis-Floyd and Melissa Cheyney Breastfeeding and Child Spacing .....................