High-Resolution Genomic Copy Number Profiling of Glioblastoma Multiforme by Single Nucleotide Polymorphism DNA Microarray
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Mouse Kcnrg Conditional Knockout Project (CRISPR/Cas9)
https://www.alphaknockout.com Mouse Kcnrg Conditional Knockout Project (CRISPR/Cas9) Objective: To create a Kcnrg conditional knockout Mouse model (C57BL/6J) by CRISPR/Cas-mediated genome engineering. Strategy summary: The Kcnrg gene (NCBI Reference Sequence: NM_206974 ; Ensembl: ENSMUSG00000046168 ) is located on Mouse chromosome 14. 2 exons are identified, with the ATG start codon in exon 1 and the TGA stop codon in exon 1 (Transcript: ENSMUST00000225582). Exon 1 will be selected as conditional knockout region (cKO region). Deletion of this region should result in the loss of function of the Mouse Kcnrg gene. To engineer the targeting vector, homologous arms and cKO region will be generated by PCR using BAC clone RP23-460E11 as template. Cas9, gRNA and targeting vector will be co-injected into fertilized eggs for cKO Mouse production. The pups will be genotyped by PCR followed by sequencing analysis. Note: Exon 1 covers 100.0% of the coding region. Start codon is in exon 1, and stop codon is in exon 1. The size of intron 1 for 3'-loxP site insertion: 3545 bp. The size of effective cKO region: ~833 bp. The cKO region does not have any other known gene. Page 1 of 7 https://www.alphaknockout.com Overview of the Targeting Strategy gRNA region Wildtype allele A gRNA region T 5' G 3' 3 1 2 Targeting vector A T G Targeted allele A T G Constitutive KO allele (After Cre recombination) Legends Exon of mouse Trim13 Homology arm Exon of mouse Kcnrg cKO region loxP site Page 2 of 7 https://www.alphaknockout.com Overview of the Dot Plot Window size: 10 bp Forward Reverse Complement Sequence 12 Note: The sequence of homologous arms and cKO region is aligned with itself to determine if there are tandem repeats. -

Comprehensive Identification and Characterization of Somatic Copy Number Alterations in Triple‑Negative Breast Cancer
INTERNATIONAL JOURNAL OF ONCOLOGY 56: 522-530, 2020 Comprehensive identification and characterization of somatic copy number alterations in triple‑negative breast cancer ZAIBING LI1,2*, XIAO ZHANG3*, CHENXIN HOU4, YUQING ZHOU4, JUNLI CHEN1, HAOYANG CAI5, YIFENG YE3, JINPING LIU3 and NING HUANG1 1Department of Pathophysiology, West China School of Basic Medical Sciences and Forensic Medicine, Sichuan University, Chengdu, Sichuan 610041; 2Department of Pathophysiology, School of Basic Medical Science, Southwest Medical University, Luzhou, Sichuan 646000; 3Department of Breast Surgery, Sichuan Provincial People's Hospital, University of Electronic Science and Technology of China, Chengdu, Sichuan 611731; 4West China Medical School, Sichuan University, Chengdu, Sichuan 610041; 5Center of Growth, Metabolism and Aging, Key Laboratory of Bio‑Resources and Eco‑Environment, College of Life Sciences, Sichuan University, Chengdu, Sichuan 610064, P.R. China Received January 30, 2019; Accepted August 30, 2019 DOI: 10.3892/ijo.2019.4950 Abstract. Triple-negative breast cancer (TNBC) accounts hierarchical clustering of tumors resulted in three main for ~15% of all breast cancer diagnoses each year. Patients subgroups that exhibited distinct CNA profiles, which with TNBC tend to have a higher risk for early relapse and may reveal the heterogeneity of molecular mechanisms in a worse prognosis. TNBC is characterized by extensive TNBC subgroups. These results will extend the molecular somatic copy number alterations (CNAs). However, the DNA understanding of TNBC and will facilitate the discovery of CNA profile of TNBC remains to be extensively investigated. therapeutic and diagnostic target candidates. The present study assessed the genomic profile of CNAs in 201 TNBC samples, aiming to identify recurrent CNAs that Introduction may drive the pathogenesis of TNBC. -
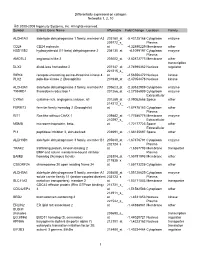
Differentially Expressed on Collagen Networks 1, 2, 10 © 2000-2009 Ingenuity Systems, Inc. All Rights Reserved. Symbol Entrez
Differentially expressed on collagen Networks 1, 2, 10 © 2000-2009 Ingenuity Systems, Inc. All rights reserved. Symbol Entrez Gene Name Affymetrix Fold Change Location Family ALDH1A3 aldehyde dehydrogenase 1 family, member A3 203180_at -5.43125168 Cytoplasm enzyme 209772_s_ Plasma CD24 CD24 molecule at -4.32890229 Membrane other HSD11B2 hydroxysteroid (11-beta) dehydrogenase 2 204130_at -4.1099197 Cytoplasm enzyme Plasma AMOTL2 angiomotin like 2 203002_at -2.82872773 Membrane other transcription DLX2 distal-less homeobox 2 207147_at -2.74996362 Nucleus regulator 221215_s_ RIPK4 receptor-interacting serine-threonine kinase 4 at -2.56556472 Nucleus kinase PLK2 polo-like kinase 2 (Drosophila) 201939_at -2.47054478 Nucleus kinase ALDH3A1 aldehyde dehydrogenase 3 family, memberA1 205623_at -2.30532989 Cytoplasm enzyme TXNRD1 thioredoxin reductase 1 201266_at -2.27936909 Cytoplasm enzyme Extracellular CYR61 cysteine-rich, angiogenic inducer, 61 201289_at -2.09052668 Space other 214212_x_ FERMT2 fermitin family homolog 2 (Drosophila) at -1.87478183 Cytoplasm other Plasma RIT1 Ras-like without CAAX 1 209882_at -1.77586775 Membrane enzyme 210297_s_ Extracellular MSMB microseminoprotein, beta- at -1.72177723 Space other Extracellular PI3 peptidase inhibitor 3, skin-derived 203691_at -1.68135697 Space other ALDH3B1 aldehyde dehydrogenase 3 family, member B1 205640_at -1.67376791 Cytoplasm enzyme 202124_s_ Plasma TRAK2 trafficking protein, kinesin binding 2 at -1.6367793 Membrane transporter BMP and activin membrane-bound inhibitor Plasma BAMBI -

Predicting Gene Ontology Biological Process from Temporal Gene Expression Patterns Astrid Lægreid,1,4 Torgeir R
Methods Predicting Gene Ontology Biological Process From Temporal Gene Expression Patterns Astrid Lægreid,1,4 Torgeir R. Hvidsten,2 Herman Midelfart,2 Jan Komorowski,2,3,4 and Arne K. Sandvik1 1Department of Cancer Research and Molecular Medicine, Norwegian University of Science and Technology, N-7489 Trondheim, Norway; 2Department of Information and Computer Science, Norwegian University of Science and Technology, N-7491 Trondheim, Norway; 3The Linnaeus Centre for Bioinformatics, Uppsala University, SE-751 24 Uppsala, Sweden The aim of the present study was to generate hypotheses on the involvement of uncharacterized genes in biological processes. To this end,supervised learning was used to analyz e microarray-derived time-series gene expression data. Our method was objectively evaluated on known genes using cross-validation and provided high-precision Gene Ontology biological process classifications for 211 of the 213 uncharacterized genes in the data set used. In addition,new roles in biological process were hypothesi zed for known genes. Our method uses biological knowledge expressed by Gene Ontology and generates a rule model associating this knowledge with minimal characteristic features of temporal gene expression profiles. This model allows learning and classification of multiple biological process roles for each gene and can predict participation of genes in a biological process even though the genes of this class exhibit a wide variety of gene expression profiles including inverse coregulation. A considerable number of the hypothesized new roles for known genes were confirmed by literature search. In addition,many biological process roles hypothesi zed for uncharacterized genes were found to agree with assumptions based on homology information. -

MOLECULAR G EN ETICS of the January, HUMAN X
MOLECULAR GENETICS OF THE HUMAN X CHROMOSOME BY DAVID ANDREW HARTLEY a thesis submitted for the degree of Doctor of Philosophy in the University of London January, 1984 Department of Biochemistry St. Mary's Hospital Medical School London W2 IPG 1 Abstract The comparison of frequency of recombination with chromosomal position has been possible only in Drosophila melanogaster but it is known that chiasma distribution in the human male (and many other species) is not random. A number of cloned DNA sequences have been isolated from a library enriched for X chromosome DNA by flow cytometry. The chromosomal loci complementary to these cloned sequences have been investigated by hybridization to somatic cell hybrid DNAs and by direct hybridization 1 in situ' to human metaphase spreads. In this way a cytological map of the X chromosome defined by DNA sequence markers has been constructed. Genetic distances complementary to the physical separations determined have been estimated by determining the segregation of DNA sequence variants at each locus in three generation p e d i g r e e s . The sequence variation is manifested as altered restriction fragment migration in agarose gels. It is intimated from these analyses that the pattern of recombination frequency along the human X chromosome mirrors the non-random chiasma distribution seen along male autosomes. This supports the chiasmatype theory and has implications on the availability of genetic components of the X chromosome to recombination. 2 To ray father in the hope of convincing him of life outside o f E.coli 3 ...scientists getting their kicks when deadly disease can do as it pleases results ain't hard to predict Gil Scott-Heron 4 Ack n ov; ledgements To my supervisor Bob Williamson for support. -

RNA Editing at Baseline and Following Endoplasmic Reticulum Stress
RNA Editing at Baseline and Following Endoplasmic Reticulum Stress By Allison Leigh Richards A dissertation submitted in partial fulfillment of the requirements for the degree of Doctor of Philosophy (Human Genetics) in The University of Michigan 2015 Doctoral Committee: Professor Vivian G. Cheung, Chair Assistant Professor Santhi K. Ganesh Professor David Ginsburg Professor Daniel J. Klionsky Dedication To my father, mother, and Matt without whom I would never have made it ii Acknowledgements Thank you first and foremost to my dissertation mentor, Dr. Vivian Cheung. I have learned so much from you over the past several years including presentation skills such as never sighing and never saying “as you can see…” You have taught me how to think outside the box and how to create and explain my story to others. I would not be where I am today without your help and guidance. Thank you to the members of my dissertation committee (Drs. Santhi Ganesh, David Ginsburg and Daniel Klionsky) for all of your advice and support. I would also like to thank the entire Human Genetics Program, and especially JoAnn Sekiguchi and Karen Grahl, for welcoming me to the University of Michigan and making my transition so much easier. Thank you to Michael Boehnke and the Genome Science Training Program for supporting my work. A very special thank you to all of the members of the Cheung lab, past and present. Thank you to Xiaorong Wang for all of your help from the bench to advice on my career. Thank you to Zhengwei Zhu who has helped me immensely throughout my thesis even through my panic. -

Mammalian Protein Expression and Characterization Tools for Next Generation Biologics
Mammalian protein expression and characterization tools for next generation biologics next generation for tools characterization and expression protein Mammalian Doctoral Thesis in Biotechnology Mammalian protein expression and characterization tools for next generation biologics NIKLAS THALÉN ISBN TRITACBHFOU: KTH www.kth.se Stockholm, Sweden Mammalian protein expression and characterization tools for next generation biologics NIKLAS THALÉN Academic Dissertation which, with due permission of the KTH Royal Institute of Technology, is submitted for public defence for the Degree of Doctor of Philosophy on June 11th, 2021 at 10:00, F3, Lindstedsvägen 26, våningsplan 2, Sing-Sing, KTH campus, Stockholm. Doctoral Thesis in Biotechnology KTH Royal Institute of Technology Stockholm, Sweden 2021 © Niklas Thalén ISBN 978-91-7873-927-1 TRITA-CBH-FOU-2021:21 Printed by: Universitetsservice US-AB, Sweden 2021 Till Sofia Abstract Protein therapeutics are increasingly important for modern medicine. Novel recombinant proteins developed today can bind towards their target with high specificity and with low adverse effect. This has enabled the treatment of diseases that for a few years ago were deemed uncurable. Discovery of therapeutic proteins is driven through protein engineering, a field that is in constant expansion. And, through artificial construction of recombinant proteins, a large array of diseases can be defeated. The function and quality of these protein therapeutics rely on the correct folding, assembly and residue modification that occurs during their production within a living production cell host. Furthermore, producing them in large quantities are essential for accessibility of the best biopharmaceuticals available. Commonly, mammalian cells are the production host of choice when it comes to production of biopharmaceuticals. -

Reproduction
REPRODUCTIONRESEARCH Focus on Mammalian Embryogenomics Molecular and subcellular characterisation of oocytes screened for their developmental competence based on glucose-6-phosphate dehydrogenase activity Helmut Torner2, Nasser Ghanem, Christina Ambros2, Michael Ho¨lker, Wolfgang Tomek2, Chirawath Phatsara, Hannelore Alm2, Marc-Andre´ Sirard1, Wilhelm Kanitz2, Karl Schellander and Dawit Tesfaye Animal Breeding and Husbandry Group, Department of Animal Breeding and Husbandry, Institute of Animal Science, University of Bonn, Endenicher allee 15, 53115 Bonn, Germany, 1De´partement des Sciences Animales, Centre de Recherche en Biologie de la Reproduction, Universite´ Laval, Pav. Comtois, Laval, Sainte-Foy, Que´bec, G1K 7P4, Canada and 2Research Institute for the Biology of Farm Animals, Wilhelm-Stahl-Allee 2, 18196 Dummerstorf, Germany Correspondence should be addressed to D Tesfaye; Email: [email protected] Abstract Oocyte selection based on glucose-6-phosphate dehydrogenase (G6PDH) activity has been successfully used to differentiate between competent and incompetent bovine oocytes. However, the intrinsic molecular and subcellular characteristics of these oocytes have not yet been investigated. Here, we aim to identify molecular and functional markers associated with oocyte developmental potential when selected based on G6PDH activity. Immature compact cumulus–oocyte complexes were stained with brilliant cresyl blue (BCB) for 90 min. Based on K C their colouration, oocytes were divided into BCB (colourless cytoplasm, high G6PDH activity) and BCB (coloured cytoplasm, low G6PDH activity). The chromatin configuration of the nucleus and the mitochondrial activityof oocytes were determined by fluorescence labelling and photometric measurement. The abundance and phosphorylation pattern of protein kinases Akt and MAP were estimated by Western blot C K analysis. -

Genomics Analysis of Potassium Channel Genes in Songbirds Reveals
Lovell et al. BMC Genomics 2013, 14:470 http://www.biomedcentral.com/1471-2164/14/470 RESEARCH ARTICLE Open Access Genomics analysis of potassium channel genes in songbirds reveals molecular specializations of brain circuits for the maintenance and production of learned vocalizations Peter V Lovell, Julia B Carleton and Claudio V Mello* Abstract Background: A fundamental question in molecular neurobiology is how genes that determine basic neuronal properties shape the functional organization of brain circuits underlying complex learned behaviors. Given the growing availability of complete vertebrate genomes, comparative genomics represents a promising approach to address this question. Here we used genomics and molecular approaches to study how ion channel genes influence the properties of the brain circuitry that regulates birdsong, a learned vocal behavior with important similarities to human speech acquisition. We focused on potassium (K-)Channels, which are major determinants of neuronal cell excitability. Starting with the human gene set of K-Channels, we used cross-species mRNA/protein alignments, and syntenic analysis to define the full complement of orthologs, paralogs, allelic variants, as well as novel loci not previously predicted in the genome of zebra finch (Taeniopygia guttata). We also compared protein coding domains in chicken and zebra finch orthologs to identify genes under positive selective pressure, and those that contained lineage-specific insertions/deletions in functional domains. Finally, we conducted comprehensive in situ hybridizations to determine the extent of brain expression, and identify K-Channel gene enrichments in nuclei of the avian song system. Results: We identified 107 K-Channel finch genes, including 6 novel genes common to non-mammalian vertebrate lineages. -

A Genome-Wide Association Study for Harness Racing Success in the Norwegian- Swedish Coldblooded Trotter Reveals Genes for Learning and Energy Metabolism Brandon D
Velie et al. BMC Genetics (2018) 19:80 https://doi.org/10.1186/s12863-018-0670-3 RESEARCHARTICLE Open Access A genome-wide association study for harness racing success in the Norwegian- Swedish coldblooded trotter reveals genes for learning and energy metabolism Brandon D. Velie1* , Kim Jäderkvist Fegraeus1, Marina Solé1, Maria K. Rosengren1, Knut H. Røed2, Carl-Fredrik Ihler3, Eric Strand3 and Gabriella Lindgren1,4 Abstract Background: Although harness racing is of high economic importance to the global equine industry, significant genomic resources have yet to be applied to mapping harness racing success. To identify genomic regions associated with harness racing success, the current study performs genome-wide association analyses with three racing performance traits in the Norwegian-Swedish Coldblooded Trotter using the 670 K Axiom Equine Genotyping Array. Results: Following quality control, 613 horses and 359,635 SNPs were retained for further analysis. After strict Bonferroni correction, nine genome-wide significant SNPs were identified for career earnings. No genome-wide significant SNPs were identified for number of gallops or best km time. However, four suggestive genome-wide significant SNPs were identified for number of gallops, while 19 were identified for best km time. Multiple genes related to intelligence, energy metabolism, and immune function were identified as potential candidate genes for harness racing success. Conclusions: Apart from the physiological requirements needed for a harness racing horse to be successful, the results of the current study also advocate learning ability and memory as important elements for harness racing success. Further exploration into the mental capacity required for a horse to achieve racing success is likely warranted. -

1471-2164-10-261.Pdf
BMC Genomics BioMed Central Research article Open Access Molecular signature of cell cycle exit induced in human T lymphoblasts by IL-2 withdrawal Magdalena Chechlinska*1, Jan Konrad Siwicki1, Monika Gos2, Malgorzata Oczko-Wojciechowska3, Michal Jarzab4, Aleksandra Pfeifer3, Barbara Jarzab3 and Jan Steffen1 Address: 1Department of Immunology, Maria Sklodowska-Curie Memorial Cancer Centre and Institute of Oncology, Warsaw, Poland, 2Department of Cell Biology, Maria Sklodowska-Curie Memorial Cancer Centre and Institute of Oncology, Warsaw, Poland, 3Department of Nuclear Medicine and Endocrine Oncology, Maria Sklodowska-Curie Memorial Cancer Centre and Institute of Oncology, Gliwice, Poland and 4Department of Tumor Biology and Clinical Oncology, Maria Sklodowska-Curie Memorial Cancer Centre and Institute of Oncology, Gliwice, Poland Email: Magdalena Chechlinska* - [email protected]; Jan Konrad Siwicki - [email protected]; Monika Gos - [email protected]; Malgorzata Oczko-Wojciechowska - [email protected]; Michal Jarzab - [email protected]; Aleksandra Pfeifer - [email protected]; Barbara Jarzab - [email protected]; Jan Steffen - [email protected] * Corresponding author Published: 8 June 2009 Received: 20 February 2009 Accepted: 8 June 2009 BMC Genomics 2009, 10:261 doi:10.1186/1471-2164-10-261 This article is available from: http://www.biomedcentral.com/1471-2164/10/261 © 2009 Chechlinska et al; licensee BioMed Central Ltd. This is an Open Access article distributed under the terms of the Creative Commons Attribution License (http://creativecommons.org/licenses/by/2.0), which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited. Abstract Background: The molecular mechanisms of cell cycle exit are poorly understood. -

Nº Ref Uniprot Proteína Péptidos Identificados Por MS/MS 1 P01024
Document downloaded from http://www.elsevier.es, day 26/09/2021. This copy is for personal use. Any transmission of this document by any media or format is strictly prohibited. Nº Ref Uniprot Proteína Péptidos identificados 1 P01024 CO3_HUMAN Complement C3 OS=Homo sapiens GN=C3 PE=1 SV=2 por 162MS/MS 2 P02751 FINC_HUMAN Fibronectin OS=Homo sapiens GN=FN1 PE=1 SV=4 131 3 P01023 A2MG_HUMAN Alpha-2-macroglobulin OS=Homo sapiens GN=A2M PE=1 SV=3 128 4 P0C0L4 CO4A_HUMAN Complement C4-A OS=Homo sapiens GN=C4A PE=1 SV=1 95 5 P04275 VWF_HUMAN von Willebrand factor OS=Homo sapiens GN=VWF PE=1 SV=4 81 6 P02675 FIBB_HUMAN Fibrinogen beta chain OS=Homo sapiens GN=FGB PE=1 SV=2 78 7 P01031 CO5_HUMAN Complement C5 OS=Homo sapiens GN=C5 PE=1 SV=4 66 8 P02768 ALBU_HUMAN Serum albumin OS=Homo sapiens GN=ALB PE=1 SV=2 66 9 P00450 CERU_HUMAN Ceruloplasmin OS=Homo sapiens GN=CP PE=1 SV=1 64 10 P02671 FIBA_HUMAN Fibrinogen alpha chain OS=Homo sapiens GN=FGA PE=1 SV=2 58 11 P08603 CFAH_HUMAN Complement factor H OS=Homo sapiens GN=CFH PE=1 SV=4 56 12 P02787 TRFE_HUMAN Serotransferrin OS=Homo sapiens GN=TF PE=1 SV=3 54 13 P00747 PLMN_HUMAN Plasminogen OS=Homo sapiens GN=PLG PE=1 SV=2 48 14 P02679 FIBG_HUMAN Fibrinogen gamma chain OS=Homo sapiens GN=FGG PE=1 SV=3 47 15 P01871 IGHM_HUMAN Ig mu chain C region OS=Homo sapiens GN=IGHM PE=1 SV=3 41 16 P04003 C4BPA_HUMAN C4b-binding protein alpha chain OS=Homo sapiens GN=C4BPA PE=1 SV=2 37 17 Q9Y6R7 FCGBP_HUMAN IgGFc-binding protein OS=Homo sapiens GN=FCGBP PE=1 SV=3 30 18 O43866 CD5L_HUMAN CD5 antigen-like OS=Homo