Escitalopram
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Efficacy of Treatments for Patients with Obsessive-Compulsive Disorder: a Systematic Review
REVIEW Efficacy of treatments for patients with obsessive-compulsive disorder: A systematic review Yun-Jung Choi, PhD, RN, PMHNP (Lecturer) Keywords Abstract Systematic review; obsessive-compulsive disorder; efficacy of medication. Purpose: This systematic review examines the efficacy of pharmacological therapy for obsessive-compulsive disorder (OCD), addressing two major issues: Correspondence which treatment is most effective in treating the patient’s symptoms and which Yun-Jung Choi, PhD, RN, PMHNP, Red Cross is beneficial for maintaining remission. College of Nursing, 98 Saemoonan-Gil, Data sources: Seven databases were used to acquire articles. The key words Jongno-Gu, Seoul 110-102, Korea; used to search for the relative topics published from 1996 to 2007 were Tel: +82-2-3700-3676; fax: +82-2-3700-3400; ‘‘obsessive-compulsive disorder’’ and ‘‘Yale-Brown obsession-compulsion E-mail: [email protected] scale.’’ Based on the inclusion and exclusion criteria, 25 studies were selected Received: August 2007; from 57 potentially relevant studies. accepted: March 2008 Conclusions: The effects of treatment with clomipramine and selective sero- tonin reuptake inhibitors (SSRIs: fluvoxamine, sertraline, fluoxetine, citalo- doi:10.1111/j.1745-7599.2009.00408.x pram, and escitalopram) proved to be similar, except for the lower adherence rate in case of clomipramine because of its side effects. An adequate drug trial involves administering an effective daily dose for a minimum of 8 weeks. An augmentation strategy proven effective for individuals refractory to monother- apy with SSRI treatment alone is the use of atypical antipsychotics (risperidone, olanzapine, and quetiapine). Implications for practice: Administration of fluvoxamine or sertraline to patients for an adequate duration is recommended as the first-line prescription for OCD, and augmentation therapy with risperidone, olanzapine, or quetiapine is recommended for refractory OCD. -

Antinociceptive Effects of Monoamine Reuptake Inhibitors in Assays of Pain-Stimulated and Pain-Depressed Behaviors
Virginia Commonwealth University VCU Scholars Compass Theses and Dissertations Graduate School 2012 Antinociceptive Effects of Monoamine Reuptake Inhibitors in Assays of Pain-Stimulated and Pain-Depressed Behaviors Marisa Rosenberg Virginia Commonwealth University Follow this and additional works at: https://scholarscompass.vcu.edu/etd Part of the Medical Pharmacology Commons © The Author Downloaded from https://scholarscompass.vcu.edu/etd/2715 This Thesis is brought to you for free and open access by the Graduate School at VCU Scholars Compass. It has been accepted for inclusion in Theses and Dissertations by an authorized administrator of VCU Scholars Compass. For more information, please contact [email protected]. ANTINOCICEPTIVE EFFECTS OF MONOAMINE REUPTAKE INHIBITORS IN ASSAYS OF PAIN-STIMULATED AND PAIN-DEPRESSED BEHAVIOR A thesis submitted in partial fulfillment of the requirements for the degree of Master of Science at Virginia Commonwealth University By Marisa B. Rosenberg Bachelor of Science, Temple University, 2008 Advisor: Sidney Stevens Negus, Ph.D. Professor, Department of Pharmacology/Toxicology Virginia Commonwealth University Richmond, VA May, 2012 Acknowledgement First and foremost, I’d like to thank my advisor Dr. Steven Negus, whose unwavering support, guidance and patience throughout my graduate career has helped me become the scientist I am today. His dedication to education, learning and the scientific process has instilled in me a quest for knowledge that I will continue to pursue in life. His thoroughness, attention to detail and understanding of pharmacology has been exemplary to a young person like me just starting out in the field of science. I’d also like to thank all of my committee members (Drs. -

Meta-Analysis of the Dose-Response Relationship of SSRI in Obsessive
Molecular Psychiatry (2010) 15, 850–855 & 2010 Macmillan Publishers Limited All rights reserved 1359-4184/10 www.nature.com/mp ORIGINAL ARTICLE Meta-analysis of the dose-response relationship of SSRI in obsessive-compulsive disorder MH Bloch1, J McGuire1, A Landeros-Weisenberger1, JF Leckman1 and C Pittenger2 1Yale Child Study Center, Yale University School of Medicine, New Haven, CT, USA and 2Department of Psychiatry, Yale University School of Medicine, New Haven, CT, USA We sought to determine differences in efficacy and tolerability between different doses of selective serotonin reuptake inhibitors in the treatment of obsessive-compulsive disorder (OCD) using meta-analysis. We identified 9 studies involving 2268 subjects that were randomized, double-blind placebo-controlled clinical trials that compared multiple, fixed- doses of selective serotonin reuptake inhibitors (SSRIs) to each other and to placebo in the treatment of adults with OCD. Change in Y-BOCS score, proportion of treatment responders, and dropouts (all-cause and due to side-effects) were determined for each included study. Weighted mean difference was used to examine mean change in Y-BOCS score. Pooled absolute risk difference was used to examine dichotomous outcomes. Meta-analysis was performed using a fixed effects model in RevMan 4.2.8. We found that compared with either low or medium doses, higher doses of SSRIs were associated with improved treatment efficacy, using either Y-BOCS score or proportion of treatment responders as an outcome. Dose of SSRIs was not associated with the number of all-cause dropouts. Higher doses of SSRIs were associated with significantly higher proportion of dropouts due to side-effects. -

A Synbiotic Mixture Augmented the Efficacy of Doxepin, Venlafaxine
A synbiotic mixture augmented the efficacy of doxepin, venlafaxine, and fluvoxamine in mice model of depression Azadeh Mesripour1, Andiya Meshkati1, Valiolah Hajhashemi2 1Department of Pharmacology and Toxicology, School of Pharmacy and Pharmaceutical Sciences, Isfahan University of Medical Sciences, Isfahan, IRAN. 2‐ Isfahan Pharmaceutical Sciences Research Center, School of Pharmacy and Pharmaceutical Sciences, Isfahan University of Medical Sciences, Isfahan, IRAN. ABSTRACT Objective: Currently available antidepressant drugs have notable downsides; in addition to their side effects and slow onset of action their moderate efficacy in some individuals, may influence compliance. Previous literature has shown that probiotics may have antidepressant effects. Introducing complementary medicineproof in order to augment the efficacy of therapeutic doses of antidepressant drugs seems to be very important. Therefore the effect of adding a synbiotic cocktail in drinking water was assessed in mice model of despair following administrating three antidepressant drugs belonging to different classes. Methods: The marble burring test (MBT), and forced swimming test (FST) were used as animal model of obsessive behavior and despair. The synbiotic cocktail was administered in mice drinking water (6.25×106 CFU) for 14 days and the tests were performed on the days 7 and 14 thirty minutes after injecting the lowest dose of doxepin (1 mg/kg), venlafaxine (15 mg/kg), and fluvoxamine (15 mg/kg). Results: After 7 days of the synbiotic ingestion immobility time decreased in FST for doxepin (92 sec ± 5.5) and venlafaxine (17.3 sec ± 2.5) compared to their control group (drinking water) but fluvoxamine could decrease immobility time after 14 days of ingesting the synbiotic (70 sec ± 7.5). -
Drug Class Review on Second Generation Antidepressants
Drug Class Review on Second Generation Antidepressants FINAL REPORT November 2004 The Agency for Healthcare Research and Quality has not yet seen or approved this report Gerald Gartlehner, M.D., M.P.H. Richard A. Hansen, Ph.D. Leila Kahwati, M.D., M.P.H. Kathleen N. Lohr, Ph.D. Bradley Gaynes, M.D., M.P.H Tim Carey, M.D., M.P.H. Produced by RTI-UNC Evidence-based Practice Center Cecil G. Sheps Center for Health Services Research University of North Carolina at Chapel Hill 725 Airport Road, CB# 7590 Chapel Hill, NC 27599-7590 Tim Carey, M.D., M.P.H., Director Final Report Drug Effectiveness Review Project Table of Contents Introduction........................................................................................................................ 4 Overview................................................................................................................. 4 Scope and Key Questions ....................................................................................... 7 Methods............................................................................................................................. 10 Literature Search................................................................................................... 10 Study Selection ..................................................................................................... 10 Data Abstraction ................................................................................................... 12 Quality Assessment.............................................................................................. -

Emerging Drug List CANADIAN COORDINATING OFFICE for HEALTH ESCITALOPRAM TECHNOLOGY ASSESSMENT
Emerging Drug List CANADIAN COORDINATING OFFICE FOR HEALTH ESCITALOPRAM TECHNOLOGY ASSESSMENT NO. 35 JANUARY 2003 Generic (Trade Name): Escitalopram (LexaproTM) Manufacturer: Forest Laboratories, Inc. Indication: For the treatment of major depressive disorders in adults.1 Current Regulatory Escitalopram was approved by the US FDA for the above indication in August 2002.2 It Status: was just recently launched in the US, according to the company's web site.3 It was launched in June 2002 in the UK under the trade name Cipralex by Lundbeck for both the treatment of depression and panic disorder.4 In Canada, escitalopram has been sub- mitted for review; no planned marketing date is available (Drug Information, Lundbeck Canada, Montreal: personal communication, 2002 Sep 30). Description: Escitalopram is the S(+) enantiomer of the chiral compound citalopram. It is a selective serotonin reuptake inhibitor that exerts activity in both depressive and anxiety disorders. After oral administration of a single dose, maximal concentrations are reached within three to four hours. It is extensively metabolized via the liver, with eight percent excreted unchanged by the kidneys. After a 20 mg dose, the elimination half-life (of the parent compound) ranges from 22 to 27 hours.5 Current Treatment: Options for the treatment of depressive disorders are vast and include selective serotonin norepinephrine reuptake inhibitors (SNRI), norepinephrine dopamine reuptake inhibitors (NDRI), serotonin-2 antagonists/reuptake inhibitors (SARI), noradrenergic/specific -
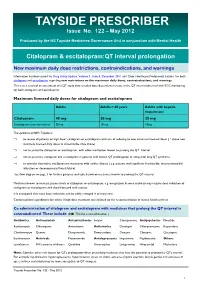
TAYSIDE PRESCRIBER Issue No
TAYSIDE PRESCRIBER Issue No. 122 – May 2012 Produced by the NS Tayside Medicines Governance Unit in conjunction with Mental Health Citalopram & escitalopram:QT interval prolongation New maximum daily dose restrictions, contraindications, and warnings Information has been issued via Drug Safety Update, Volume 5, Issue 5, December 2011 and ‘Dear Healthcare Professional Letters’ for both citalopram and escitalopram regarding new restrictions on the maximum daily doses, contraindications, and warnings. This is as a result of an assessment of a QT study that revealed dose-dependent increase in the QT interval observed with ECG monitoring for both citalopram and escitalopram. Maximum licensed daily doses for citalopram and escitalopram Adults Adults > 65 years Adults with hepatic impairment Citalopram 40 mg 20 mg 20 mg Escitalopram (non-formulary) 20 mg 10 mg 10mg The guidance in NHS Tayside is: ⇒ to review all patients on high dose* citalopram or escitalopram with aim of reducing to new maximum licensed doses ( * above new maximum licensed daily doses as stated in the table above) ⇒ not to prescribe citalopram or escitalopram with other medication known to prolong the QT interval ⇒ not to prescribe citalopram and escitalopram in patients with known QT prolongation or congenital long QT syndrome ⇒ to consider alternative antidepressant in patients with cardiac disease ( e.g. patients with significant bradycardia; recent myocardial infarction or decompensated heart failure) See flow diagram on page 3 for further guidance and table below on medicines known to prolong the QT interval. Medicines known to increase plasma levels of citalopram or escitalopram, e.g. omeprazole & some antivirals may require dose reduction of citalopram or escitalopram and should be used with caution. -
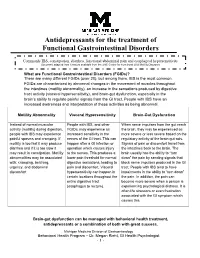
Antidepressants for Functional Gastrointestinal Disorders
Antidepressants for the treatment of Functional Gastrointestinal Disorders Commonly IBS, constipation, diarrhea, functional abdominal pain and esophageal hypersensitivity Document adapted from literature available from the UNC Center for Functional GI & Motility Disorders What are Functional Gastrointestinal Disorders (FGIDs)? There are many different FGIDs (over 20), but among them, IBS is the most common. FGIDs are characterized by abnormal changes in the movement of muscles throughout the intestines (motility abnormality), an increase in the sensations produced by digestive tract activity (visceral hypersensitivity), and brain-gut dysfunction, especially in the brain’s ability to regulate painful signals from the GI tract. People with IBS have an increased awareness and interpretation of these activities as being abnormal. Motility Abnormality Visceral Hypersensitivity Brain-Gut Dysfunction Instead of normal muscular People with IBS, and other When nerve impulses from the gut reach activity (motility) during digestion, FGIDs, may experience an the brain, they may be experienced as people with IBS may experience increased sensitivity in the more severe or less severe based on the painful spasms and cramping. If nerves of the GI tract. This can regulatory activity of the brain-gut axis. motility is too fast it may produce happen after a GI infection or Signals of pain or discomfort travel from diarrhea and if it is too slow it operation which causes injury the intestines back to the brain. The may result in constipation. Motility to the nerves. This produces a brain usually has the ability to “turn abnormalities may be associated lower pain threshold for normal down” the pain by sending signals that with: cramping, belching, digestive sensations, leading to block nerve impulses produced in the GI urgency, and abdominal pain and discomfort. -

Doxepin Exacerbates Renal Damage, Glucose Intolerance, Nonalcoholic Fatty Liver Disease, and Urinary Chromium Loss in Obese Mice
pharmaceuticals Article Doxepin Exacerbates Renal Damage, Glucose Intolerance, Nonalcoholic Fatty Liver Disease, and Urinary Chromium Loss in Obese Mice Geng-Ruei Chang 1,* , Po-Hsun Hou 2,3, Wei-Cheng Yang 4, Chao-Min Wang 1 , Pei-Shan Fan 1, Huei-Jyuan Liao 1 and To-Pang Chen 5,* 1 Department of Veterinary Medicine, National Chiayi University, 580 Xinmin Road, Chiayi 60054, Taiwan; [email protected] (C.-M.W.); [email protected] (P.-S.F.); [email protected] (H.-J.L.) 2 Department of Psychiatry, Taichung Veterans General Hospital, 1650 Taiwan Boulevard (Section 4), Taichung 40705, Taiwan; [email protected] 3 Faculty of Medicine, National Yang-Ming University, 155 Linong Street (Section 2), Taipei 11221, Taiwan 4 School of Veterinary Medicine, National Taiwan University, 1 Roosevelt Road (Section 4), Taipei 10617, Taiwan; [email protected] 5 Division of Endocrinology and Metabolism, Show Chwan Memorial Hospital, 542 Chung-Shan Road (Section 1), Changhua 50008, Taiwan * Correspondence: [email protected] (G.-R.C.); [email protected] (T.-P.C.); Tel.: +886-5-2732946 (G.-R.C.); +886-4-7256166 (T.-P.C.) Abstract: Doxepin is commonly prescribed for depression and anxiety treatment. Doxepin-related disruptions to metabolism and renal/hepatic adverse effects remain unclear; thus, the underlying mechanism of action warrants further research. Here, we investigated how doxepin affects lipid Citation: Chang, G.-R.; Hou, P.-H.; change, glucose homeostasis, chromium (Cr) distribution, renal impairment, liver damage, and fatty Yang, W.-C.; Wang, C.-M.; Fan, P.-S.; liver scores in C57BL6/J mice subjected to a high-fat diet and 5 mg/kg/day doxepin treatment for Liao, H.-J.; Chen, T.-P. -
A Synbiotic Mixture Augmented the Efficacy of Doxepin, Venlafaxine
Turk J Pharm Sci 2020;17(3):293-298 DOI: 10.4274/tjps.galenos.2019.94210 ORIGINAL ARTICLE A Synbiotic Mixture Augmented the Efficacy of Doxepin, Venlafaxine, and Fluvoxamine in a Mouse Model of Depression Sinbiyotik Karışım, Fare Depresyon Modelinde Doksepin, Venlafaksin ve Fluvoksaminin Etkinliğini Artırdı Azadeh MESRIPOUR1*, Andiya MESHKATI1, Valiollah HAJHASHEMI2 1Isfahan University of Medical Sciences, School of Pharmacy and Pharmaceutical Sciences, Department of Pharmacology and Toxicology, Isfahan, Iran 2Isfahan University of Medical Sciences, School of Pharmacy and Pharmaceutical Sciences, Isfahan Pharmaceutical Sciences Research Center, Isfahan, Iran ABSTRACT Objectives: Currently available antidepressant drugs have notable downsides; in addition to their side effects and slow onset of action their moderate efficacy in some individuals may influence compliance. Previous literature has shown that probiotics may have antidepressant effects. Introducing complementary medicine in order to augment the efficacy of therapeutic doses of antidepressant drugs appears to be very important. Therefore, the effect of adding a synbiotic mixture to drinking water was assessed in a mouse model of depression following the administration of three antidepressant drugs belonging to different classes. Materials and Methods: The marble burying test (MBT) and forced swimming test (FST) were used as animal models of obsessive behavior and despair. The synbiotic mixture was administered to the mice’s drinking water (6.25x106 CFU) for 14 days and the tests were performed 30 min after the injection of the lowest dose of doxepin (1 mg/kg), venlafaxine (15 mg/kg), and fluvoxamine (15 mg/kg) on days 7 and 14. Results: After 7 days of ingestion of the synbiotic mixture, immobility time decreased in the FST for doxepin (92±5.5 s) and venlafaxine (17.3±2.5 s) compared to the control group (drinking water), but fluvoxamine decreased immobility time after 14 days of ingestion of the synbiotic mixture (70±7.5 s). -

Arrhythmias Caused by Ondansetron: Case Report
CorSalud 2019 Apr-Jun;11(2):171-174 Cuban Society of Cardiology ________________________ Case Report Arrhythmias caused by ondansetron: Case report Juan M. Chala Tandrón1, MD; Liset Jiménez Fernández2, MD, MSc; Zoila Armada Esmores2, MD, MSc; Yudileidy Brito Ferrer2, MD, MSc; Melba Zayas González2, MD, MSc; and Maiyen García Arcia2, MD 1 Department of Anesthesiology and Resuscitation, Hospital Oncológico Universitario “Dr. Celestino Hernández Robau”. Santa Clara, Villa Clara, Cuba. 2 Department of Pharmacology, Universidad de Ciencias Médicas de Villa Clara. Santa Clara, Villa Clara, Cuba, Cuba. Este artículo también está disponible en español ARTICLE INFORMATION ABSTRACT The ondansetron is used to prevent nausea and vomiting caused by chemothera- Received: April 4, 2019 py, radiotherapy and surgery, belonging to the serotonin 5-HT3 receptor antago- Accepted: May 21, 2019 nists, a natural substance that can cause nausea and vomiting, and it blocks its action. The ondansetron is packaged in the form of rapid disintegration tablets, as Competing interests a solution to be taken orally and in ampules, for parenteral use. The case of a 67- The authors declare no competing year-old female patient is presented, with a diagnosis of breast carcinoma, who interests underwent radical mastectomy with axillary dissection was performed, and who received chemotherapy with adriamycin, cyclophosphamide and paclitaxel; as well as ondansetron to treat nausea and vomiting. The patient presented a wide QRS complex tachycardia after taking the drug. Keywords: Ondansetron, Cardiac arrhythmias, Wide QRS complex tachycardia Arritmias provocadas por ondansetrón: Presentación de un caso RESUMEN El ondansetrón se usa para prevenir las náuseas y los vómitos causados por la quimioterapia, radioterapia y cirugías, pertenece a los antagonistas de receptores de serotonina 5-HT3, una sustancia natural que puede causar náuseas y vómitos, y bloquea su acción. -

Impact of Citalopram and Fluvoxamine on Platelet Response To
S24_5 Impact of Citalopram and Fluvoxamine on Platelet Response to Clopidogrel, a Randomized, Double-blind, Crossover Trial Bruria Hirsh Racch1, Galia Spectre2, Ella Shai2, Amit Ritter3, David Varon2, Ronny Alcalai3 1School of Pharmacy, Hadassah Hebrew University Medical Center, Israel 2Coagulation Unit, Hematology, Hadassah Hebrew University Medical Center, Israel 3Heart Institute, Hadassah Hebrew University Medical Center, Israel Background: Selective serotonin reuptake inhibitors (SSRI) are widely used antidepressant agents. Studies have shown that use of SSRI in combination with aspirin or warfarin is associated with an increased risk bleeding, while little information is known about the interaction of SSRIs and clopidogrel. Fluvoxamine and citalopram are both SSRIs and while fluvoxamine is an inhibitor of CYP2C19 and thus might reduce the efficacy of clopidogrel, the effect of citalopram on liver metabolism is unknown. Aim: The aim was to assess the effect these two different SSRIs on platelet aggregation and on the laboratory response to clopidogrel. Methods: A randomized, double-blind, crossover study in 15 healthy volunteers comparing the antiplatelet effect of clopidogrel with and without fluvoxamine or citalopram .The response to clopidogrel was assessed by Light Transmittance Aggregometry with10µmol/L ADP and by vasodilator-stimulated phosphoprotein (VASP) phosphorylation, a measure of P2Y12 receptor reactivity. Results: Mean baseline platelet aggregation was 80.1%±3.4 and reduced to 23.5% after treatment with clopidogrel. Both fluvoxamine and citalopram had modest effect on platelet reactivity (65.8%±6.4, p=0.06 vs. baseline and 67.3%±6.3, p=0.07 vs. baseline respectively). Laboratory response to clopidogrel was significantly better in the presence of citalopram as compared to fluvoxamine both in aggregometry (23.4%±3 vs.