Detection of Previously Undetected Leprosy Cases in Firozabad District (U.P.), India During 2006–2009: a Short Communication
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Section-VIII : Laboratory Services
Section‐VIII Laboratory Services 8. Laboratory Services 8.1 Haemoglobin Test ‐ State level As can be seen from the graph, hemoglobin test is being carried out at almost every FRU studied However, 10 percent medical colleges do not provide the basic Hb test. Division wise‐ As the graph shows, 96 percent of the FRUs on an average are offering this service, with as many as 13 divisions having 100 percent FRUs contacted providing basic Hb test. Hemoglobin test is not available at District Women Hospital (Mau), District Women Hospital (Budaun), CHC Partawal (Maharajganj), CHC Kasia (Kushinagar), CHC Ghatampur (Kanpur Nagar) and CHC Dewa (Barabanki). 132 8.2 CBC Test ‐ State level Complete Blood Count (CBC) test is being offered at very few FRUs. While none of the sub‐divisional hospitals are having this facility, only 25 percent of the BMCs, 42 percent of the CHCs and less than half of the DWHs contacted are offering this facility. Division wise‐ As per the graph above, only 46 percent of the 206 FRUs studied across the state are offering CBC (Complete Blood Count) test service. None of the FRUs in Jhansi division is having this service. While 29 percent of the health facilities in Moradabad division are offering this service, most others are only a shade better. Mirzapur (83%) followed by Gorakhpur (73%) are having maximum FRUs with this facility. CBC test is not available at Veerangna Jhalkaribai Mahila Hosp Lucknow (Lucknow), Sub Divisional Hospital Sikandrabad, Bullandshahar, M.K.R. HOSPITAL (Kanpur Nagar), LBS Combined Hosp (Varanasi), -

“Everyone Has Been Silenced”; Police
EVERYONE HAS BEEN SILENCED Police Excesses Against Anti-CAA Protesters In Uttar Pradesh, And The Post-violence Reprisal Citizens Against Hate Citizens against Hate (CAH) is a Delhi-based collective of individuals and groups committed to a democratic, secular and caring India. It is an open collective, with members drawn from a wide range of backgrounds who are concerned about the growing hold of exclusionary tendencies in society, and the weakening of rule of law and justice institutions. CAH was formed in 2017, in response to the rising trend of hate mobilisation and crimes, specifically the surge in cases of lynching and vigilante violence, to document violations, provide victim support and engage with institutions for improved justice and policy reforms. From 2018, CAH has also been working with those affected by NRC process in Assam, documenting exclusions, building local networks, and providing practical help to victims in making claims to rights. Throughout, we have also worked on other forms of violations – hate speech, sexual violence and state violence, among others in Uttar Pradesh, Haryana, Rajasthan, Bihar and beyond. Our approach to addressing the justice challenge facing particularly vulnerable communities is through research, outreach and advocacy; and to provide practical help to survivors in their struggles, also nurturing them to become agents of change. This citizens’ report on police excesses against anti-CAA protesters in Uttar Pradesh is the joint effort of a team of CAH made up of human rights experts, defenders and lawyers. Members of the research, writing and advocacy team included (in alphabetical order) Abhimanyu Suresh, Adeela Firdous, Aiman Khan, Anshu Kapoor, Devika Prasad, Fawaz Shaheen, Ghazala Jamil, Mohammad Ghufran, Guneet Ahuja, Mangla Verma, Misbah Reshi, Nidhi Suresh, Parijata Banerjee, Rehan Khan, Sajjad Hassan, Salim Ansari, Sharib Ali, Sneha Chandna, Talha Rahman and Vipul Kumar. -

Training Needs of Basic School Teachers in Agra & Firozabad
See discussions, stats, and author profiles for this publication at: https://www.researchgate.net/publication/232175269 TRAINING NEEDS OF BASIC SCHOOL TEACHERS IN AGRA & FIROZABAD DISTRICT OF UTTAR PRADESH Article · June 2012 CITATIONS READS 0 46 Some of the authors of this publication are also working on these related projects: Gender Sensitization View project Value Education View project All content following this page was uploaded by Rajshree . on 27 March 2016. The user has requested enhancement of the downloaded file. International Journal of Educational Research and Technology Volume 3 Issue 2 June 2012: 172 - 174 ISSN 0976 - 4089 www.soeagra.com/ijert.htm IIJJEERRTT © Society of Education, India Original Article Training Needs of Basic School Teachers in Agra & Firozabad District of Uttar Pradesh Rajshree Department of Education, DEI, Deemed University, Dayalbagh, Agra ABSTRACT The teacher occupies a very important place in society because he brings about the transfer of the values and tradition from one generation to next. He maintains the level of technological skill and keeps the light of civilization burning bright. He is expected to help in the level of social revolution that is taking place in the country. His duty does not end in the classroom with his students. He should be able to constantly adjust his methods and approach to suit the changing times. Teachers need training for better results to students and society. Need of training for primary and secondary teachers have been emphasized by many educational commissions/committees, therefore this study has been conducted to know the training needs of basic schools teachers. INTRODUCTION The world continues to experience constant change. -

Report on Proposed Plantation Scheme in and Around Agra City
Report on Proposed plantation scheme in and around Agra City Central Pollution Control Board, Delhi, on the basis of values of Particulate Matter (PM10- Particle Matter Size less than 10 micron) in ambient air has identified 15 cities of Uttar Pradesh as Non- attainment cities. Agra is one of the fifteen non attainment city. U P Pollution Control Board prepared draft action plans for 15 non- attainment cities of Uttar Pradesh. The Action Plans comprises of 06 Major categories as given below:- a. Vehicle Emission Control b. Suspension of Road Dust and Fugitive Emission Control c. Control of Emissions form Biomass/ Crop residue/ Garbage/ Municipal Solid Waste burning d. Control of Industrial Emissions e. Control of Air Pollution from constructions and demolition activities. f. Other Steps to Control Air Pollution. The Action Plans comprises of 58 Short and long term Action Points. The short term (immediate) activities which don't need advance preparedness and are to be implemented by concerned department/ agencies immediately and the long term action points require preparedness including making of DPRs, Sanctions, Budget allocation and implementation. Two main action points of this plan to mitigate pollution are to prepare plan for creation of green buffers along the traffic corridors and Plantation of specific types of species of plants which are helpful in pollution control and Tree Plantation for mitigation of air pollution based upon location of pollution sources and Wind rose data. ABOUT THE CITY: Agra - has been immortalized as the City of the Taj. Taj Mahal is the universally admired masterpiece of the world's heritage. -
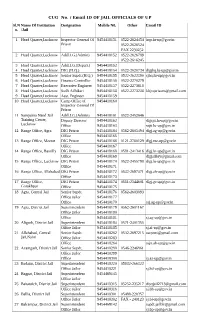
CUG No. / Email ID of JAIL OFFICIALS of up Sl.N Name of Institution Designation Mobile N0
CUG No. / Email ID OF JAIL OFFICIALS OF UP Sl.N Name Of Institution Designation Mobile N0. Other Email ID o. /Jail 1 Head Quarter,Lucknow Inspector General Of 9454418151 0522-2624454 [email protected] Prison 0522-2626524 FAX 2230252 2 Head Quarter,Lucknow Addl.I.G.(Admin) 9454418152 0522-2626789 0522-2616245 3 Head Quarter,Lucknow Addl.I.G.(Depart.) 9454418153 4 Head Quarter,Lucknow DIG (H.Q.) 9454418154 0522-2620734 [email protected] 5 Head Quarter,Lucknow Senior Supdt.(H.Q.) 9454418155 0522-2622390 [email protected] 6 Head Quarter,Lucknow Finance Controller 9454418156 0522-2270279 7 Head Quarter,Lucknow Executive Engineer 9454418157 0522-2273618 8 Head Quarter,Lucknow Sodh Adhikari 9454418158 0522-2273238 [email protected] 9 Head Quarter,Lucknow Asst. Engineer 9454418159 10 Head Quarter,Lucknow Camp Office of 9454418160 Inspector General Of Prison 11 Sampurna Nand Jail Addl.I.G.(Admin) 9454418161 0522-2452646 Training Center, Deputy Director 9454418162 [email protected] Lucknow Office 9454418163 [email protected] 12 Range Office, Agra DIG Prison 9454418164 0562-2605494 [email protected] Office 9454418165 13 Range Office, Meerut DIG Prison 9454418166 0121-2760129 [email protected] Office 9454418167 14 Range Office, Bareilly DIG Prison 9454418168 0581-2413416 [email protected] Office 9454418169 [email protected] 15 Range Office, Lucknow DIG Prison 9454418170 0522-2455798 [email protected] Office 9454418171 16 Range Office, Allahabad DIG Prison 9454418172 0532-2697471 [email protected] Office 9454418173 17 Range Office, DIG Prison 9454418174 0551-2344601 [email protected] Gorakhpur Office 9454418175 18 Agra, Central Jail Senior Supdt. -

Existing Housing and Feeding Management Practices of Buffaloes in Firozabad District of Uttar Pradesh, India
Int.J.Curr.Microbiol.App.Sci (2017) 6(5): 1831-1838 International Journal of Current Microbiology and Applied Sciences ISSN: 2319-7706 Volume 6 Number 5 (2017) pp. 1831-1838 Journal homepage: http://www.ijcmas.com Original Research Article https://doi.org/10.20546/ijcmas.2017.605.200 Existing Housing and Feeding Management Practices of Buffaloes in Firozabad District of Uttar Pradesh, India Raj Kumar1*, P.K. Singh1, R.K. Goyal1, Hitesh Singh2 and B.L. Kumhar3 1Department of Animal Husbandry and Dairying, R.B.S. College, Bichpuri, Agra-283105, India 2Department of A.H, SVPUAT, Meerut, India 3GKMS Project, Agricultural Research Station, Ummedganj, Kota, India *Corresponding author ABSTRACT Study was carried out in Firozabad district of Uttar Pradesh involving 120 buffalo owners scattered in eight villages of two Tehsil. The farmers were further categorized into three groups viz., small (< 2 adult buffaloes), medium (> 2 and < 5 adult bufalloes) and large (> K e yw or ds 5 adult buffaloes) householders. Data pertaining to various aspects of housing and feeding practices were collected through a pre- tested questionnaire. The results indicate that only Buffaloes, 60per cent of buffalo owners provide proper housing shelter to their buffaloes, 68.33 per Housing, feeding, cent respondent’s possessed animal house with Kachcha floor with very poor ventilation management facilities. Only 54.17 per cent houses have slope for proper drainage of urine and faeces practices, and 64.17 percent respondent’s made additional arrangement to protect buffaloes against households. extreme weather. More than three fourth respondents provide green fodder to buffaloes Article Info throughout the year and of them nearly half of them fed it after chaffing. -

A Study of Economics of Milk Production in Firozabad District of Western Uttar Pradesh, India Abstract
1 Plant Archives Vol. 20, Supplement 2, 2020 pp. 4280-4283 e-ISSN:2581-6063 (online), ISSN:0972-5210 A STUDY OF ECONOMICS OF MILK PRODUCTION IN FIROZABAD DISTRICT OF WESTERN UTTAR PRADESH, INDIA Kulshrestha R.K. 1, Sharma V.K. 2 and Sharma Amod* 3 1. Department of Agricultural Economics, Raja Balwant Singh College, Bichpuri, District-Agra (Uttar Pradesh), India 2. Department of Agricultural Extension, Raja Balwant Singh College, Bichpuri, District-Agra (Uttar Pradesh), India 3. Department of Agricultural Economics, Nagaland University, SASRD, Medziphema Campus, District: Dimapur Nagaland – 797112, India. *Corresponding author : Amod Sharma ABSTRACT Dairy farming plays a significant role in the socio-economic development in India. Milk production in India is mainly concentrated on marginal and small farms in rural areas as a subsidiary occupation to agriculture. In addition to this, there are number of organized dairy farms under the cooperative milk producers’ union. In the country, the low genetic potential of animals results in the high cost and low milk production. A survey based study was carried out to ascertain the cost of milk production, using a pretested schedule for sample size of 28 farms. Dairy farmers in Hathwanth block of Firozabad District of Uttar Pradesh. The profit margin can be increased by decreasing the cost of production. The overall cost of milk production per litre was Rs. 16.49. Keywords: Milk, production, gross, maintenance, cost, net. Introduction population. In an average Indian diet, however, animal proteins make up only less than 10 per cent of the total In ancient as less than a divine status the ancient scriptures declare that A God lives where women are protein. -

Investigation on Ethnomedicinal Plants of District Firozabad
www.sospublication.co.in Journal of Advanced Laboratory Research in Biology We- together to save yourself society e-ISSN 0976-7614 Volume 1, Issue 1, July 2010 Article Investigation on Ethnomedicinal Plants of District Firozabad Kalpana Singh*, Sweety Gupta and P.K. Mathur *Department of Botany, BSA College, Mathura (U.P.)-281001, India. Abstract: A survey in Firozabad District has been done for documented ethnomedicinal plants. About 71 plants have reported in this manuscript which is used for various diseases. This manuscript is very useful for those who work with herbal plants. Keywords: Firozabad, Ethnomedicinal, Aegle marmelos L., Allium cepa, Ethnobotanical. 1. Introduction Tribal in this northern District of U.P. carried out the survey in remote villages of Distt. Firozabad to India is a veritable emporium of medicinal and identify the common and cultivated medicinal plants aromatic plants. It has been estimated that out of 15,000 and their utilization. The study area selected in higher plants occurring in India. 9,000 are commonly Firozabad lies between 27°00’ and 27°24’ north latitude used, of which 7,500 are medicinal, 3,900 are culturally and 77°66’ and 70°04’ east longitude. It is bounded in important, 525 are used for fiber, 400 are for fodder, north by Etah district, in east by Etawah and Mainpuri, 300 for pesticide and insecticide, 300 for gum and in the south by Yamuna River and in the west by Agra resin, and 100 for incense and perfumes [1]. In terms of district. The climate of Firozabad is characterized by the plant materials used for traditional medicine, it is hot summer, pleasant winter and general dryness except estimated that local communities have used over 7,500 during rainy season. -

Basic Information of Urban Local Bodies – Uttar Pradesh
BASIC INFORMATION OF URBAN LOCAL BODIES – UTTAR PRADESH As per 2006 As per 2001 Census Election Name of S. Growth Municipality/ Area No. of No. Class House- Total Rate Sex No. of Corporation (Sq. Male Female SC ST (SC+ ST) Women Rate Rate hold Population (1991- Ratio Wards km.) Density Membe rs 2001) Literacy 1 2 3 4 5 6 7 8 9 10 11 12 13 14 15 16 I Saharanpur Division 1 Saharanpur District 1 Saharanpur (NPP) I 25.75 76430 455754 241508 214246 39491 13 39504 21.55 176 99 887 72.31 55 20 2 Deoband (NPP) II 7.90 12174 81641 45511 36130 3515 - 3515 23.31 10334 794 65.20 25 10 3 Gangoh (NPP) II 6.00 7149 53913 29785 24128 3157 - 3157 30.86 8986 810 47.47 25 9 4 Nakur (NPP) III 17.98 3084 20715 10865 9850 2866 - 2866 36.44 1152 907 64.89 25 9 5 Sarsawan (NPP) IV 19.04 2772 16801 9016 7785 2854 26 2880 35.67 882 863 74.91 25 10 6 Rampur Maniharan (NP) III 1.52 3444 24844 13258 11586 5280 - 5280 17.28 16563 874 63.49 15 5 7 Ambehta (NP) IV 1.00 1739 13130 6920 6210 1377 - 1377 27.51 13130 897 51.11 12 4 8 Titron (NP) IV 0.98 1392 10501 5618 4883 2202 - 2202 30.53 10715 869 54.55 11 4 9 Nanauta (NP) IV 4.00 2503 16972 8970 8002 965 - 965 30.62 4243 892 60.68 13 5 10 Behat (NP) IV 1.56 2425 17162 9190 7972 1656 - 1656 17.80 11001 867 60.51 13 5 11 Chilkana Sultanpur (NP) IV 0.37 2380 16115 8615 7500 2237 - 2237 27.42 43554 871 51.74 13 5 86.1 115492 727548 389256 338292 65600 39 65639 23.38 8451 869 67.69 232 28 2 Muzaffarnagar District 12 Muzaffarnagar (NPP) I 12.05 50133 316729 167397 149332 22217 41 22258 27.19 2533 892 72.29 45 16 13 Shamli -

13 2 2019 12 40 41 GZB RECRUITMENT.Pdf
from Downloaded www.upsrtc.com 2nd Merit List for Postal Address S.No. Merit Name of Applicant Father's Name Address Regi. No. Caste No. 1 703 UTTAM PANDEY SURESH PANDEY VILL-MUNDERA URF GZB-378 General DEURWA POST-SHAJAHAPUR THANA-RAMPUR KARKHANA DIST-DEORIA UP 2 704 SUDHANSHU ARVIND KUMAR VILLAGE NIYAMATPUR POSTfrom GZB-8193 General TIWARI TIWARI SONBARSHA DISTT FAIZABAD STATE UTTAR PRADESH 224208 3 705 RAM KRISHAN RAGURAJ PRATAP DHANMAU KINHAWAR GZB-14321 General SINGH MAINPURI 205267 4 706 NAVEEN SHIVRAJ SINGH BICHHIYA ROAD TEACHER GZB-20304 General CHAUHAN COLONY KRISHNA NAGAR MAINPURI 205001 5 707 HUNDILAL SATYA DEV VILLAGE SINGHPUR GZB-9564 General SHARMA SHARMA HIMMATPUR POST TEOTHU TEHSIL ATRAULI DISTRICT ALIGARH PIN CODE 202280 6 708 Sanjeev Sharma Radhe Shyam Pahra, Kaila, Etah, UP GZB-25706 General 7 709 VIKASH GUPTA SHIV KUMAR VILL NASIRPUR SAIDAN PO GZB-10156 General GUPTA KISHUNDASPUR TEH KADIPUR DISTT SULTANPUR UP PIN 228145 8 710 DURGESH AMICHAND VILL AJANIYAN MAJRA GZB-7761 General SHARMA SHARMA JAMANKA POST BISARA DIST DownloadedALIGARH www.upsrtc.com 9 711 UMA KANT KARUN CHANDRA VILL KALU PURWA PAKDI GZB-21270 General SHUKLA SHUKLA MARUDEEH POST BICHHUDI KAURIA BAZAR DISTT GONDA PIN 271122 10 712 RAHUL SHARMA MAHA VEER VILLAGE SINGHOLA CHET GZB-7053 General SHARMA SINGH POST SINGHOLA DAULAT SINGH THANA RAJPURA TEHSIL GUNNOUR from SAMBHAL 11 713 MUKESH RAKESH KUMAR B-239, KARAN VIHAR PART-5, GZB-112 General KUMAR KIRARI SULEMAN NAGAR DELHI 110086 12 714 SACHIN MANOJ VILLAGE AND POST GZB-11942 General UPADHYAY -

Housing Management Practices Prevailed Among Livestock Owners
International Journal of Chemical Studies 2018; 6(6): 2812-2816 P-ISSN: 2349–8528 E-ISSN: 2321–4902 IJCS 2018; 6(6): 2812-2816 Housing management practices prevailed among © 2018 IJCS Received: 24-09-2018 livestock owners in Firozabad district of western UP Accepted: 28-10-2018 Raj Kumar Raj Kumar, PK Singh, Jagdeep Kumar, Hitesh Singh, Satyaveer Singh Ph.D., Fellow, Department of and Pawan Kumar Animal Husbandry, College of Veterinary and Animal Sciences, Sardar Vallabhbhai Patel Abstract University of Agriculture & Livestock is one of the most important activities among the rural farmers. It provides sustainable income Technology, Meerut, Uttar and reduces unemployment to a large number of the rural poor. The study on housing management Pradesh, India practices of buffaloes was purposively conducted in Firozabad district of Uttar Pradesh since it has got predominant buffalo based dairy production system. Out of four two Tehsil viz., Jasarana and Shikohabad PK Singh Associate Professor, Department of the district were randomly selected for the study. A total of 120 buffalo farmers were selected for the Animal Husbandry and Dairying, study. An exploratory research design and multistage random sampling technique was applied for the Bichpuri, Agra, Uttar Pradesh, study and data were collected using a structured interview schedule. The study revealed that majority of India the farmers the farmers were further categorized into three groups viz., small (< 2 adult buffaloes), medium (> 2 and < 5 adult buffaloes) and large (> 5 adult buffaloes) householders. The results indicate Jagdeep Kumar that only 60% of buffalo owners provide proper housing shelter to their buffaloes. 68.33% respondents Ph.D., Fellow, Department of possessed animal house with Kachcha floor with very poor ventilation facilities. -
Doubling the Farmers' Income in Uttar Pradesh by 2022
DOUBLING THE FARMERS’ INCOME IN UTTAR PRADESH BY 2022 - - OPPORTUNITIES & CONSTRAINTS AMARNATH TRIPATHI INSTITUTE OF ECONOMIC GROWTH, DELHI CONTENTS 1 INTRODUCTION .................................................................................................................................. 1 1.1 WHY UTTAR PRADESH ............................................................................................................................ 2 1.2 IMPORTANCE OF AGRICULTURE SECTOR IN UP ............................................................................................ 2 1.3 OBJECTIVES OF THE PRESENT STUDY .......................................................................................................... 6 1.3.1 Farmer level objectives ............................................................................................................. 6 1.3.2 Macro level objectives .............................................................................................................. 7 1.4 ORGANIZATION OF THE REPORT ................................................................................................................ 8 2 THEORY OF FARMERS’ INCOME ........................................................................................................ 18 2.1 SOURCES OF INCOME GROWTH WITHIN AGRICULTURE SECTOR ...................................................................... 19 2.2 SOURCES OF INCOME GROWTH OUTSIDE AGRICULTURE SECTOR ..................................................................... 21 3 SAMPLES