ARHGDIA: a Novel Gene Implicated in Nephrotic Syndrome
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

ARHGDIA: a Novel Gene Implicated in Nephrotic Syndrome
Developmental defects J Med Genet: first published as 10.1136/jmedgenet-2012-101442 on 22 February 2013. Downloaded from ORIGINAL ARTICLE ARHGDIA: a novel gene implicated in nephrotic syndrome Indra Rani Gupta,1,2,3 Cindy Baldwin,4 David Auguste,4,5 Kevin C H Ha,3,6 Jasmine El Andalousi,2 Somayyeh Fahiminiya,3,6 Martin Bitzan,1,2 Chantal Bernard,7 Mohammad Reza Akbari,8,9 Steven A Narod,8,9 David S Rosenblatt,1,3,4 Open Access 3,6 2,4,5 Scan to access more Jacek Majewski, Tomoko Takano free content ▸ Additional material is ABSTRACT the barrier into the urine. The glomerular filtration published online only. To view Background Congenital nephrotic syndrome arises barrier consists of fenestrated endothelial cells, the please visit the journal online fi (http://dx.doi.org/10.1136/ from a defect in the glomerular ltration barrier that acellular glomerular basement membrane that is jmedgenet-2012-101442). permits the unrestricted passage of protein across the about 300 nm thick, and specialised epithelial cells barrier, resulting in proteinuria, hypoalbuminaemia, and called podocytes. The majority of children with For numbered affiliations see end of article. severe oedema. While most cases are due to mutations congenital nephrotic syndrome have a monogenic in one of five genes, in up to 15% of cases, a genetic basis for their disease due to mutations in genes Correspondence to cause is not identified. We investigated two sisters with that affect the structure and function of the actin Dr Indra Rani Gupta, a presumed recessive form of congenital nephrotic cytoskeleton within podocytes.1 In a large survey, Department of Pediatrics, ∼ Division of Nephrology, syndrome. -

Mir-34/449 Control Apical Actin Network Formation During Multiciliogenesis Through Small Gtpase Pathways
ARTICLE Received 7 Jul 2015 | Accepted 17 Aug 2015 | Published 18 Sep 2015 DOI: 10.1038/ncomms9386 OPEN miR-34/449 control apical actin network formation during multiciliogenesis through small GTPase pathways Benoıˆt Chevalier1,2,*, Anna Adamiok3,*, Olivier Mercey1,2,*, Diego R. Revinski3, Laure-Emmanuelle Zaragosi1,2, Andrea Pasini3, Laurent Kodjabachian3, Pascal Barbry1,2 & Brice Marcet1,2 Vertebrate multiciliated cells (MCCs) contribute to fluid propulsion in several biological processes. We previously showed that microRNAs of the miR-34/449 family trigger MCC differentiation by repressing cell cycle genes and the Notch pathway. Here, using human and Xenopus MCCs, we show that beyond this initial step, miR-34/449 later promote the assembly of an apical actin network, required for proper basal bodies anchoring. Identification of miR-34/449 targets related to small GTPase pathways led us to characterize R-Ras as a key regulator of this process. Protection of RRAS messenger RNA against miR-34/449 binding impairs actin cap formation and multiciliogenesis, despite a still active RhoA. We propose that miR-34/449 also promote relocalization of the actin binding protein Filamin-A, a known RRAS interactor, near basal bodies in MCCs. Our study illustrates the intricate role played by miR-34/449 in coordinating several steps of a complex differentiation programme by regulating distinct signalling pathways. 1 CNRS, Institut de Pharmacologie Mole´culaire et Cellulaire (IPMC), UMR-7275, 660 route des Lucioles, 06560 Sophia-Antipolis, France. 2 University of Nice-Sophia-Antipolis (UNS), Institut de Pharmacologie Mole´culaire et Cellulaire, 660 route des Lucioles, Valbonne, 06560 Sophia-Antipolis, France. -

The Human Gene Connectome As a Map of Short Cuts for Morbid Allele Discovery
The human gene connectome as a map of short cuts for morbid allele discovery Yuval Itana,1, Shen-Ying Zhanga,b, Guillaume Vogta,b, Avinash Abhyankara, Melina Hermana, Patrick Nitschkec, Dror Friedd, Lluis Quintana-Murcie, Laurent Abela,b, and Jean-Laurent Casanovaa,b,f aSt. Giles Laboratory of Human Genetics of Infectious Diseases, Rockefeller Branch, The Rockefeller University, New York, NY 10065; bLaboratory of Human Genetics of Infectious Diseases, Necker Branch, Paris Descartes University, Institut National de la Santé et de la Recherche Médicale U980, Necker Medical School, 75015 Paris, France; cPlateforme Bioinformatique, Université Paris Descartes, 75116 Paris, France; dDepartment of Computer Science, Ben-Gurion University of the Negev, Beer-Sheva 84105, Israel; eUnit of Human Evolutionary Genetics, Centre National de la Recherche Scientifique, Unité de Recherche Associée 3012, Institut Pasteur, F-75015 Paris, France; and fPediatric Immunology-Hematology Unit, Necker Hospital for Sick Children, 75015 Paris, France Edited* by Bruce Beutler, University of Texas Southwestern Medical Center, Dallas, TX, and approved February 15, 2013 (received for review October 19, 2012) High-throughput genomic data reveal thousands of gene variants to detect a single mutated gene, with the other polymorphic genes per patient, and it is often difficult to determine which of these being of less interest. This goes some way to explaining why, variants underlies disease in a given individual. However, at the despite the abundance of NGS data, the discovery of disease- population level, there may be some degree of phenotypic homo- causing alleles from such data remains somewhat limited. geneity, with alterations of specific physiological pathways under- We developed the human gene connectome (HGC) to over- come this problem. -

Silencing of METTL3 Effectively Hinders Invasion and Metastasis of Prostate Cancer Cells
Silencing of METTL3 effectively hinders invasion and metastasis of prostate cancer cells Yabing Chen1,2 #, Chun Pan1,2#, Xiaotong Wang3, Dihui Xu1,2, Yuhan Ma1,2 , Jianhang Hu1,2 , Peilin Chen1,2, Zou Xiang4, Qiu Rao3, Xiaodong Han1,2 1 Immunology and Reproduction Biology Laboratory & State Key Laboratory of Analytical Chemistry for Life Science, Medical School, Nanjing University, Nanjing 210093, China 2 Jiangsu Key Laboratory of Molecular Medicine, Nanjing University, Nanjing 210093, China 3 Department of Pathology, Jinling Hospital, Nanjing University School of Medicine, Nanjing 210002, China 4 Department of Health Technology and Informatics, Faculty of Health and Social Sciences, The Hong Kong Polytechnic University, Hung Hom, Kowloon, Hong Kong China #These authors contributed equally to this study. Corresponding authors: Qiu Rao, [email protected], Department of Pathology, Jinling Hospital, Nanjing 210002, China; Xiaodong Han, [email protected], Immunology and Reproduction Biology Laboratory, Medical School, Nanjing University, Nanjing 210093, China, Tel/fax: +86 25 83686497. 1 Table S1. Primary antibodies used in this study. Source Primary antibodies Catalog no. Working dilution Abcam Rabbit anti-METTL3 ab195352 WB, 1:2000 IHC, 1: 800 Abcam Mouse anti-FTO ab92981 WB, 1:1000 IHC, 1:400 Abcam Rabbit anti-ZEB1 ab203829 WB, 1:500 IHC Santa Cruz Biotechnology Mouse anti-ARHGDIB sc-376473 WB,1:500 Santa Cruz Biotechnology Mouse anti-E-cadherin sc-8426 WB,1:500 Santa Cruz Biotechnology Mouse anti-HNRNPD sc-166577 WB,1:500 Santa Cruz Biotechnology -

Supplemental Figures
Supplemental Figures A 160 140 120 100 80 60 ARHGDIA 40 ARHGDIB 20 Relative expresssion Relative 0 Undifferentiated Differentiated Lymphblasts podocytes podocytes ARHGDIA 115.3 99.9 64.2 ARHGDIB 1.1 1.0 139.9 B Supplemental Figure 1. Differential expression of ARHGDIA and ARHGDIB in podocytes (A) Expression measured by quantitative real-time PCR was normalized to GAPDH expression. Note that, whereas ARHGDIB is expressed more in lymphoblasts, ARHGDIA are 100 times more expressed in both undifferentiated and differentiated podocytes than ARHGDIB. Real-time PCR was performed using StepOnePlusTM Real-Time PCR System (Applied Biosystems). TaqMan probes for ARHGDIA (Hs00366348_g1), ARHGDIB (Hs00171288_m1), and glyceraldhyde-3- phosphate dehydrogenase (GAPDH) (Hs02758991_g1) were purchased from Applied Biosystems. The relative RNA expression levels were calculated via a comparative threshold cycle (Ct) method using GAPDH as control: ∆Ct=Ct(GAPDH)-Ct(ARHGDIA or ARHGDIB). The gene expression fold change, normalized to the GAPDH and relative to the control sample (ARHGDIB expression in the differentiated podocytes), was calculated as 2-∆∆Ct. Error bars, s.e.m. of six experiments. (B) Expression of ARHGDIA and ARHGDIB in various cell lines. ARHGDIB is more enriched in lymphoblasts, in contrast, ARHGDIA is expressed ubiquitously. ARHGDIB antibody was purchased from BD Pharmigen. A B Supplemental Figure 2. Interaction of ARHGDIA wild type (WT) and two mutants (p.R120X and p.G173V) with RHO GTPases in culture human podocytes. (A) Coimmunoprecipitation of FLAG-tagged ARHGDIA constructs with endogenous RHO GTPases. Coimmunoprecipation were performed using anti-FLAG antibody and rec-Protein G-Sepharose 4B Conjugate (Invitrogen). (B) GST pulldown with purified ARHGDIA (WT and mutants) proteins. -

Oxidized Phospholipids Regulate Amino Acid Metabolism Through MTHFD2 to Facilitate Nucleotide Release in Endothelial Cells
ARTICLE DOI: 10.1038/s41467-018-04602-0 OPEN Oxidized phospholipids regulate amino acid metabolism through MTHFD2 to facilitate nucleotide release in endothelial cells Juliane Hitzel1,2, Eunjee Lee3,4, Yi Zhang 3,5,Sofia Iris Bibli2,6, Xiaogang Li7, Sven Zukunft 2,6, Beatrice Pflüger1,2, Jiong Hu2,6, Christoph Schürmann1,2, Andrea Estefania Vasconez1,2, James A. Oo1,2, Adelheid Kratzer8,9, Sandeep Kumar 10, Flávia Rezende1,2, Ivana Josipovic1,2, Dominique Thomas11, Hector Giral8,9, Yannick Schreiber12, Gerd Geisslinger11,12, Christian Fork1,2, Xia Yang13, Fragiska Sigala14, Casey E. Romanoski15, Jens Kroll7, Hanjoong Jo 10, Ulf Landmesser8,9,16, Aldons J. Lusis17, 1234567890():,; Dmitry Namgaladze18, Ingrid Fleming2,6, Matthias S. Leisegang1,2, Jun Zhu 3,4 & Ralf P. Brandes1,2 Oxidized phospholipids (oxPAPC) induce endothelial dysfunction and atherosclerosis. Here we show that oxPAPC induce a gene network regulating serine-glycine metabolism with the mitochondrial methylenetetrahydrofolate dehydrogenase/cyclohydrolase (MTHFD2) as a cau- sal regulator using integrative network modeling and Bayesian network analysis in human aortic endothelial cells. The cluster is activated in human plaque material and by atherogenic lipo- proteins isolated from plasma of patients with coronary artery disease (CAD). Single nucleotide polymorphisms (SNPs) within the MTHFD2-controlled cluster associate with CAD. The MTHFD2-controlled cluster redirects metabolism to glycine synthesis to replenish purine nucleotides. Since endothelial cells secrete purines in response to oxPAPC, the MTHFD2- controlled response maintains endothelial ATP. Accordingly, MTHFD2-dependent glycine synthesis is a prerequisite for angiogenesis. Thus, we propose that endothelial cells undergo MTHFD2-mediated reprogramming toward serine-glycine and mitochondrial one-carbon metabolism to compensate for the loss of ATP in response to oxPAPC during atherosclerosis. -
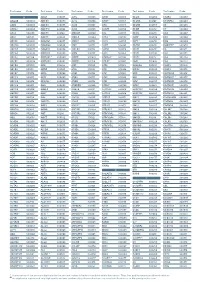
Aagab S00002 Aars S00003 Aars2 S00004 Aass S02483
Test name Code Test name Code Test name Code Test name Code Test name Code Test name Code A ADAR S00053 ALPL S00105 ARSB S00153 BCL10 S02266 C5AR2 S00263 AAGAB S00002 ADCK3 S00054 ALS2 S00106 ARSE * S00154 BCL11A S02167 C5ORF42 S00264 AARS S00003 ADCK4 S00055 ALX3 S00107 ARX S00155 BCL11B S02358 C6 S00265 AARS2 S00004 ADCY10 S02094 ALX4 S00108 ASAH1 S00156 BCOR S00212 C7 S00266 AASS S02483 ADCY3 S02184 AMACR S00109 ASL S00157 BCS1L S00213 C8A S00267 ABAT S02191 ADCY5 S02226 AMELX S02289 ASNS * S02508 BDNF S02509 C8B S00268 ABCA1 S00005 ADGRG1 S00057 AMER1 S00110 ASPA S00158 BDP1 * S00214 C8G S00269 ABCA12 S00006 ADGRG6 S02548 AMH S00111 ASPH S02425 BEAN1 S00215 C8ORF37 S00270 ABCA3 S00007 ADGRV1 S00058 AMHR2 S00112 ASPM S00159 BEST1 S00216 C9 S00271 ABCA4 S00008 ADIPOQ S00059 AMN S00113 ASS1 S00160 BFSP1 S02280 CA2 S00272 ABCA7 S02106 ADIPOR1 * S00060 AMPD1 S02670 ATAD3A * S02196 BFSP2 S00217 CA4 S02303 ABCB11 S00009 ADIPOR2 S00061 AMPD2 S02128 ATCAY S00162 BGN S02633 CA8 S00273 ABCB4 S00010 ADK S02595 AMT S00114 ATF6 S00163 BHLHA9 S00218 CABP2 S00274 ABCB6 S00011 ADNP S02320 ANG S00115 ATIC S02458 BICD2 S00220 CABP4 S00275 ABCB7 S00012 ADSL S00062 ANK1 S00116 ATL1 S00164 BIN1 S00221 CACNA1A S00276 ABCC2 S00013 AFF2 S00063 ANK2 S00117 ATL3 S00165 BLK S00222 CACNA1C * S00277 ABCC6 * S00014 AFG3L2 * S00064 ANKH S00118 ATM S00166 BLM S00223 CACNA1D S00278 ABCC8 S00015 AGA S00065 ANKRD11 * S02140 ATOH7 S02390 BLNK S02281 CACNA1F S00279 ABCC9 S00016 AGBL5 S02452 ANKS6 S00121 ATP13A2 S00168 BLOC1S3 S00224 CACNA1H S00280 ABCD1 * S00017 AGK * -

Rac1 Gtpase in Rodent Kidneys Is Essential for Salt-Sensitive Hypertension Via a Mineralocorticoid Receptor–Dependent Pathway
Rac1 GTPase in rodent kidneys is essential for salt-sensitive hypertension via a mineralocorticoid receptor–dependent pathway Shigeru Shibata, … , Miki Nagase, Toshiro Fujita J Clin Invest. 2011;121(8):3233-3243. https://doi.org/10.1172/JCI43124. Research Article Nephrology Hypertension is a leading contributor to cardiovascular mortality worldwide. Despite this, its underlying mechanism(s) and the role of excess salt in cardiorenal dysfunction are unclear. Previously, we have identified cross-talk between mineralocorticoid receptor (MR), a nuclear transcription factor regulated by the steroid aldosterone, and the small GTPase Rac1, which is implicated in proteinuric kidney disease. We here show that high-salt loading activates Rac1 in the kidneys in rodent models of salt-sensitive hypertension, leading to blood pressure elevation and renal injury via an MR-dependent pathway. We found that a high-salt diet caused renal Rac1 upregulation in salt-sensitive Dahl (Dahl-S) rats and downregulation in salt-insensitive Dahl (Dahl-R) rats. Despite a reduction of serum aldosterone levels, salt-loaded Dahl-S rats showed increased MR signaling in the kidneys, and Rac1 inhibition prevented hypertension and renal damage with MR repression. We further demonstrated in aldosterone-infused rats as well as adrenalectomized Dahl-S rats with aldosterone supplementation that salt-induced Rac1 and aldosterone acted interdependently to cause MR overactivity and hypertension. Finally, we confirmed the key role of Rac1 in modulating salt susceptibility in mice lacking Rho GDP– dissociation inhibitor α. Therefore, our data identify Rac1 as a determinant of salt sensitivity and provide insights into the mechanism of salt-induced hypertension and kidney injury. -

KDM6A-ARHGDIB Axis Blocks Metastasis of Bladder Cancer By
Liu et al. Molecular Cancer (2021) 20:77 https://doi.org/10.1186/s12943-021-01369-9 RESEARCH Open Access KDM6A-ARHGDIB axis blocks metastasis of bladder cancer by inhibiting Rac1 Lei Liu1,2,3†, Jianfeng Cui1,2,3†, Yajing Zhao4, Xiaochen Liu2, Lipeng Chen1,2,3, Yangyang Xia1,2,3, Yong Wang1,2,3, Shouzhen Chen1,2,3, Shuna Sun5, Benkang Shi1,3* and Yongxin Zou2* Abstract Background: KDM6A, a histone demethylase, is frequently mutated in bladder cancer (BCa). However, the role and detailed molecular mechanism of KDM6A involved in bladder cancer progression remains unknown. Methods: Tissue specimens were used to determine the expression levels and prognostic values of KDM6A and ARHGDIB. The MTT, colony formation, wound healing and Transwell migration and invasion assays were employed to detect the BCa cell proliferation, migration and invasion, respectively. Chemotaxis of macrophages was used to evaluate the ability of KDM6A to recruit macrophages. A subcutaneous tumour model and tail vein tumour injection in nude mice were used to assess the role of KDM6A in vivo. RNA sequencing, qPCR, Western blot, ChIP and phalloidin staining assay were performed to investigate the molecular functions of KDM6A. Dual-luciferase reporter assay was used to determine the effects of KDM6A and FOXA1 on the promoters of the ARHGDIB and KDM6A. Results: We showed that the KDM6A inhibited the motility and invasiveness of the BCa cells. Mechanistically, KDM6A promotes the transcription of ARHGDIB by demethylating histone H3 lysine di/trimethylation (H3K27me2/3) and consequently leads to inhibition of Rac1. EZH2, which catalyses the methylation of H3K27, functions to silence ARHGDIB expression, and an EZH2 inhibitor can neutralize the metastatic effect caused by KDM6A deficiency. -

Output Contraction and Decreased Bone Marrow Associated With
Downloaded from http://www.jimmunol.org/ by guest on September 27, 2021 is online at: average * The Journal of Immunology , 22 of which you can access for free at: 2013; 191:1210-1219; Prepublished online 3 July from submission to initial decision 4 weeks from acceptance to publication 2013; doi: 10.4049/jimmunol.1203462 http://www.jimmunol.org/content/191/3/1210 Increased ID2 Levels in Adult Precursor B Cells as Compared with Children Is Associated with Impaired Ig Locus Contraction and Decreased Bone Marrow Output Kristin Jensen, Magdalena B. Rother, Berit Sletbakk Brusletto, Ole K. Olstad, Hans Christian Dalsbotten Aass, Menno C. van Zelm, Peter Kierulf and Kaare M. Gautvik J Immunol cites 51 articles Submit online. Every submission reviewed by practicing scientists ? is published twice each month by http://jimmunol.org/subscription Submit copyright permission requests at: http://www.aai.org/About/Publications/JI/copyright.html Receive free email-alerts when new articles cite this article. Sign up at: http://jimmunol.org/alerts http://www.jimmunol.org/content/suppl/2013/07/03/jimmunol.120346 2.DC1 This article http://www.jimmunol.org/content/191/3/1210.full#ref-list-1 Information about subscribing to The JI No Triage! Fast Publication! Rapid Reviews! 30 days* Why • • • Material References Permissions Email Alerts Subscription Supplementary The Journal of Immunology The American Association of Immunologists, Inc., 1451 Rockville Pike, Suite 650, Rockville, MD 20852 Copyright © 2013 by The American Association of Immunologists, Inc. All rights reserved. Print ISSN: 0022-1767 Online ISSN: 1550-6606. This information is current as of September 27, 2021. -

Comprehensive Characterization of Protein-Protein Interaction Network
bioRxiv preprint doi: https://doi.org/10.1101/2020.09.18.302588; this version posted September 21, 2020. The copyright holder for this preprint (which was not certified by peer review) is the author/funder, who has granted bioRxiv a license to display the preprint in perpetuity. It is made available under aCC-BY-NC-ND 4.0 International license. Comprehensive characterization of protein-protein interaction network perturbations by human disease mutations Feixiong Cheng1-3,#, Junfei Zhao4,5,#, Yang Wang6,7,#, Weiqiang Lu8,#, Zehui Liu9, Yadi Zhou1, William Martin1, Ruisheng Wang10, Jin Huang9, Tong Hao 6,7, Hong Yue6,7, Jing Ma6,7, Yuan Hou1, Jessica Castrillon1, Jiansong Fang1, Justin D. Lathia2,3, Ruth A. Keri3,11, Felice C. Lightstone12, Elliott Marshall Antman13, Raul Rabadan4,5, David E. Hill6,7, Charis Eng1-3,14,15, Marc Vidal6,7, Joseph Loscalzo10,* 1Genomic Medicine Institute, Lerner Research Institute, Cleveland Clinic, Cleveland, OH 44195, USA 2Department of Molecular Medicine, Cleveland Clinic Lerner College of Medicine, Case Western Reserve University, Cleveland, OH 44195, USA 3Case Comprehensive Cancer Center, Case Western Reserve University School of Medicine, Cleveland, Ohio 44106, USA 4Department of Systems Biology, Herbert Irving Comprehensive Center, Columbia University, New York, NY 10032, USA 5Department of Biomedical Informatics, Columbia University, New York, NY 10032, USA 6Center for Cancer Systems Biology (CCSB) and Department of Cancer Biology, Dana- Farber Cancer Institute, Boston, MA 02215, USA. 7Department of Genetics, Blavatnik Institute, Harvard Medical School, 77 Avenue Louis Pasteur, Boston, MA 02115, USA. 8Shanghai Key Laboratory of Regulatory Biology, Institute of Biomedical Sciences and School of Life Sciences, East China Normal University, Shanghai 200062, China 9Shanghai Key Laboratory of New Drug Design, School of Pharmacy, East China bioRxiv preprint doi: https://doi.org/10.1101/2020.09.18.302588; this version posted September 21, 2020. -

Identification of Three Novel Ca Channel Subunit Genes Reveals
Downloaded from genome.cshlp.org on October 4, 2021 - Published by Cold Spring Harbor Laboratory Press Letter Identification of Three Novel Ca2+ Channel ␥ Subunit Genes Reveals Molecular Diversification by Tandem and Chromosome Duplication Daniel L. Burgess,1,2 Caleb F. Davis,1 Lisa A. Gefrides,1 and Jeffrey L. Noebels1 1Department of Neurology, Baylor College of Medicine, Houston, Texas 77030 USA Gene duplication is believed to be an important evolutionary mechanism for generating functional diversity within genomes. The accumulated products of ancient duplication events can be readily observed among the genes encoding voltage-dependent Ca2+ ion channels. Ten paralogous genes have been identified that encode isoforms of the ␣1 subunit, four that encode  subunits, and three that encode ␣2␦ subunits. Until recently, only a single gene encoding a muscle-specific isoform of the Ca2+ channel ␥ subunit (CACNG1) was known. Expression of a distantly related gene in the brain was subsequently demonstrated upon isolation of the Cacng2 gene, which is mutated in the mouse neurological mutant stargazer (stg). In this study, we sought to identify additional genes that encoded ␥ subunits. Because gene duplication often generates paralogs that remain in close syntenic proximity (tandem duplication) or are copied onto related daughter chromosomes (chromosome or whole-genome duplication), we hypothesized that the known positions of CACNG1 and CACNG2 could be used to predict the likely locations of additional ␥ subunit genes. Low-stringency genomic sequence analysis of targeted regions led to the identification of three novel Ca2+ channel ␥ subunit genes, CACNG3, CACNG4, and CACNG5,on chromosomes 16 and 17. These results demonstrate the value of genome evolution models for the identification of distantly related members of gene families.