The Eshowe Hiv Project
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Kwazulu-Natal Province Facility, Sub-District and District
KWAZULU-NATAL PROVINCE FACILITY, SUB-DISTRICT AND DISTRICT Facility Posts Period Field of Study Province District Sub-District Facility 2017 Audiologist kz KwaZulu-Natal Province kz Amajuba District Municipality kz Dannhauser Local Municipality kz Dannhauser CHC 1 kz Dannhauser Local Municipality Total 1 kz Newcastle Local Municipality kz Madadeni Hospital 1 kz Newcastle Local Municipality Total 1 kz Amajuba District Municipality Total 2 kz eThekwini Metropolitan Municipality kz eThekwini Metropolitan Municipality Sub kz Hlengisizwe CHC 1 kz Tongaat CHC 1 kz eThekwini Metropolitan Municipality Sub Total 2 kz eThekwini Metropolitan Municipality Total 2 kz Harry Gwala District Municipality kz Greater Kokstad Local Municipality kz East Griqualand and Usher Memorial Hospital 1 kz Greater Kokstad Local Municipality Total 1 kz Ubuhlebezwe Local Municipality kz Christ the King Hospital 1 kz Ubuhlebezwe Local Municipality Total 1 kz Umzimkhulu Local Municipality kz Rietvlei Hospital 1 kz St Margaret's TB MDR Hospital 1 kz Umzimkhulu Local Municipality Total 2 kz Harry Gwala District Municipality Total 4 kz iLembe District Municipality kz Mandeni Local Municipality kz Sundumbili CHC 1 kz Mandeni Local Municipality Total 1 kz Ndwedwe Local Municipality kz Montebello Hospital 1 kz Ndwedwe Local Municipality Total 1 kz iLembe District Municipality Total 2 kz Ugu District Municipality kz Hibiscus Coast Local Municipality kz Gamalakhe CHC 1 kz Hibiscus Coast Local Municipality Total 1 kz Ugu District Municipality Total 1 kz uMgungundlovu District Municipality -

South Africa
Safrica Page 1 of 42 Recent Reports Support HRW About HRW Site Map May 1995 Vol. 7, No.3 SOUTH AFRICA THREATS TO A NEW DEMOCRACY Continuing Violence in KwaZulu-Natal INTRODUCTION For the last decade South Africa's KwaZulu-Natal region has been troubled by political violence. This conflict escalated during the four years of negotiations for a transition to democratic rule, and reached the status of a virtual civil war in the last months before the national elections of April 1994, significantly disrupting the election process. Although the first year of democratic government in South Africa has led to a decrease in the monthly death toll, the figures remain high enough to threaten the process of national reconstruction. In particular, violence may prevent the establishment of democratic local government structures in KwaZulu-Natal following further elections scheduled to be held on November 1, 1995. The basis of this violence remains the conflict between the African National Congress (ANC), now the leading party in the Government of National Unity, and the Inkatha Freedom Party (IFP), the majority party within the new region of KwaZulu-Natal that replaced the former white province of Natal and the black homeland of KwaZulu. Although the IFP abandoned a boycott of the negotiations process and election campaign in order to participate in the April 1994 poll, following last minute concessions to its position, neither this decision nor the election itself finally resolved the points at issue. While the ANC has argued during the year since the election that the final constitutional arrangements for South Africa should include a relatively centralized government and the introduction of elected government structures at all levels, the IFP has maintained instead that South Africa's regions should form a federal system, and that the colonial tribal government structures should remain in place in the former homelands. -

The Cholera Outbreak
The Cholera Outbreak: A 2000-2002 case study of the source of the outbreak in the Madlebe Tribal Authority areas, uThungulu Region, KwaZulu-Natal rdsn Edward Cottle The Rural Development Services Network (RDSN) Private Bag X67 Braamfontein 2017 Tel: (011) 403 7324 www.rdsn.org.za Hameda Deedat International Labour and Research Information Group (ILRIG) P.O. Box 1213 Woodstock 7915 Tel: (021) 447 6375 www.aidc.org.za/ilrig Edited by Dudley Moloi Sub-edited by Nicolas Dieltiens Funders: Municipal Services Project SOUTH AFRICAN MUNICIPAL WORKERS’ UNION Acknowledgements A special word of thanks to: Fieldworkers Dudu Khumalo and Sikhumbuso Khanyile from SAMWU KZN, for their help with the community interviews. And to our referees: Dr. David Hemson (Human Science Research Council) Dr. David Sanders (Public Health Programme, University of the Western Cape) Sue Tilley (Social Consultant) Stephen Greenberg (Social Consultant) Contents Executive summary 1 Section 1: Introduction 7 1.1 Objectives of the study 9 Section 2: Methodology 10 2.1 Research methods 10 2.1.1 Transepts 10 2.1.2 In-depth Interviews 11 2.1.3 Interviews in Ngwelezane 11 2.1.4 Interviews in the rural areas 12 2.1.5 Interviews with municipal officials 12 2.2 Limitations of the research 13 Section 3: The Policy Context 14 Section 4: The Geographic Context 16 4.1 A description of the area under Investigation 16 4.1.1 Introduction 16 4.1.2 Brief History 16 4.1.3 Demographic information 17 4.1.4 Economic Expansion 18 4.1.5 Climate & Disease 20 4.1.6 Water & Sanitation 20 4.2 Post-apartheid -

Umlalazi Strategic Planning Session
UMLALAZI STRATEGIC PLANNING SESSION INTEGRATED DEVELOPMENT PLANNING Lizette Dirker IDP Coordination Business Unit INFORMANTS OF THE IDP SOUTH AFRICAN PLANNING SYSTEMS National Provincial Local District wide PGDS Vision 2030 DGDP (Vision 2035) (Vision 2035) National IDP PGDP Development 5 years Plan National Provincial Municipal Planning Planning Council Commission Commission WARD BASED SDGs SDGs PLANS “KZN as a prosperous Province with healthy, secure and skilled population, living in dignity and harmony, acting as a gateway to Africa and the World” Sustainable Development Goals AGENDA 2063 50 Year Vision • Agenda 2063 is a strategic framework for the socio-economic transformation of the continent over the next 50 years. It builds on, and seeks to accelerate the implementation of past and existing continental initiatives for growth and sustainable development Adopted in January 2015 • Adopted in January 2015, in Addis Ababa, Ethiopia by the 24th African Union (AU) Assembly of Heads of State and Government 10 Year implementation cycle • Five ten year implementation plan – the first plan 2014-2023 1. A prosperous Africa based on inclusive growth and sustainable 5. An Africa with a strong cultural development identity, common heritage, shared values and ethics 2. An integrated continent, politically united and based on the ideals of Pan-Africanism and the 6. An Africa whose development vision of Africa’s Renaissance is people-driven, relying on the potential of African people, especially its women and youth, and caring for children 3. An Africa of good governance, democracy, respect for human rights, justice and the rule of law 7. Africa as a strong, united and influential global player and partner 4. -

Kwazulu Natal Province 1
KWAZULU NATAL PROVINCE 1. PCO CODE 088 LADYSMITH (UKHAHLAMBA REGIONAL OFFICE) MP Edna Molewa (NEC member) Cell 082 964 1256 PLO Errol E Makoba Cell 082 601 8181 Email [email protected] Administrator Thulani Dlamini Cell 073 6791439 Physical Address Tribent Building 220 Murchison Street Ladysmith, 3370 Postal Address P.O. Box 3791, Ladysmith, 3370 Tel 036 635 4701 Fax 036 635 4685 E-mail [email protected] Ward 1-25(25) Municipality Emnambithi Region Ukhahlamba 2. PCO CODE 802 PHOENIX MP Trevor Bonhomme Cell 082 8700 673 Administrator Stanley Moonsamy Cell 072 140 9017 Physical Address Phoenix Community Centre 20 Feathersstone Place Whetsone Phoenix 4068 Postal Address P.O.Box 311, Mount Edgecom Place.Whestone Phoenix 4300 Tel 031 5071800 Fax 031 500 8575 E-mail [email protected]/[email protected] Ward 48-57 (9) Municipality Ethekwini Region Ethekwini 3. PCO CODE 803 Moses Mabhida Regional Office MP Jackson Mthembu (NEC member) Cell 082 370 8401 Administrator Mlungisi Zondi Cell 0839472453 Physical Address 163 Jabu Ndlovu Street, Pietermaritzburg, 3200 Postal Address P.O. Box 1443, Pietermaritzburg, 3200 Tel 033 345 2753 /0716975765 Fax 033 342 3149 E-mail [email protected]/[email protected] Ward 1-9(9) Municipality Msunduzi Region Moses Mabhida 4. PCO CODE 805 PORT SHEPSTONE REGIONAL OFFICE MP Joyce Moloi-Moropa (NEC member) Cell 082718 4050 MPL Nonzwakazi Swartbooi Cell 083 441 9993 Administrator Lindiwe Mzele Cell 0731703811 Tel 039 682 6148 Fax 039 682 6141 E-mail [email protected]/[email protected] 10 October 2014 1 Physical Address 1st Flr, No.1 City Insurance Bldng, 44Wooley Street, Port Shepstone, 4240 Postal Address P.O. -

WWF-Mondi Wetlands Programme 25 Year Publication
WWF-MONDI WETLANDS PROGRammE B A quarter century of C wetlandconservation 1 Dragonflies are indicators of healthy wetlands. © PETER ChaDwiCK What’s in a name? Over the course of its 25-year journey, the now WWF-Mondi Wetlands Programme has changed its name three times. 1991–2000: 2013–present: Rennies Wetland Project WWF-Mondi Wetlands Programme The programme was named after the Rennies In late 2013, the management and implementation Group – the primary funder at the start – and was of the programme was transferred from WESSA managed and implemented by Ezemvelo KZN to WWF-SA. It formed an integral part of the new Wildlife (then the Natal Parks Board) from 1991 to global partnership between WWF and Mondi 1995, with WESSA taking over in 1996. and was formally renamed the WWF-Mondi Wetlands Programme. 2001–2012: WWF and Mondi acknowledge and thank all the Mondi Wetlands Programme previous funders and conservation management The programme’s name changed in 2001 when agencies for their roles and contributions in Mondi became the primary funder. WESSA was initiating, shaping and growing the success of still the lead management agency, with strategic the programme. support from WWF-SA in guiding the programme and expanding its global reach. In this publication, the programme is referred to by its current name, i.e. the WWF-Mondi Wetlands Programme (WWF-MWP). 2 Foreword 12 Supporting the wise use of communal wetlands 36 Message from Morné du Plessis CEO: WWF-SA 4 13 Growing young wetland and environmental professionals through Message from Ron -

Nkandla Forest Complex MP
Nkandla Forest Complex: Nkandla Forest Reserve Dhlabe Nature Reserve Edodweni Nature Reserve Mndunduzeli Nature Reserve Mome Nature Reserve Sibudeni Nature Reserve Vungwini Nature Reserve KwaZulu-Natal South Africa Protected Area Management Plan Prepared by Ezemvelo KwaZulu-Natal Wildlife Protected Area Management Planning Unit and Nkandla Forest Complex Planning Committee Citation: Nkandla Forest Complex: Management Plan. Version 1.0 (August 2015), Ezemvelo KZN Wildlife, Pietermaritzburg. Cover Photo Credits: Dr Hugh Chittenden, Sharon Louw, Shing Shan Lu. AUTHORISATION This Protected Area Management Plan for Nkandla Forest Complex is recommended by the Nkandla Forest Complex Planning Committee (NRPC), a multi-disciplinary team consisting of: Ezemvelo KZN Wildlife Ken Morty General Manager: East Roy Jones Conservation Manager: Ilembe, uThungulu & uMkhanyakhude Districts & PA’s Elliakim Zungu Officer in Charge: Nkandla Forest Complex Sharon Louw District Ecologist: Ilembe & uThungulu Cyril Buthelezi Community Conservation Officer (CCO): Ilembe & uThungulu Edward Khanyile District Conservation Officer (DCO): Eshowe Magda Goosen Protected Area Management Planner Shiven Rambarath Protected Area Management Junior Planner NKANDLA FOREST COMPLEX PROTECTED AREA MANAGEMENT PLAN i APPROVAL This Management Plan for the Nkandla Forest Complex is approved by: TITLE NAME DATE SIGNATURE KwaZulu-Natal MEC: Department of Economic M. Mabuyakhulu Development, Tourism and Environmental Affairs Recommended: TITLE NAME DATE SIGNATURE Chairperson: KZN Nature -
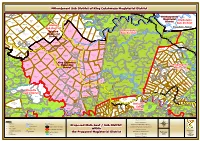
Threatened Ecosystems in South Africa: Descriptions and Maps
Threatened Ecosystems in South Africa: Descriptions and Maps DRAFT May 2009 South African National Biodiversity Institute Department of Environmental Affairs and Tourism Contents List of tables .............................................................................................................................. vii List of figures............................................................................................................................. vii 1 Introduction .......................................................................................................................... 8 2 Criteria for identifying threatened ecosystems............................................................... 10 3 Summary of listed ecosystems ........................................................................................ 12 4 Descriptions and individual maps of threatened ecosystems ...................................... 14 4.1 Explanation of descriptions ........................................................................................................ 14 4.2 Listed threatened ecosystems ................................................................................................... 16 4.2.1 Critically Endangered (CR) ................................................................................................................ 16 1. Atlantis Sand Fynbos (FFd 4) .......................................................................................................................... 16 2. Blesbokspruit Highveld Grassland -
KZN Kcsub 022018 Mthonjan
!C !C^ ñ!.!C !C $ !C^ ^ ^ !C !C !C!C !C !C !C ^ ^ !C !C ^ !C !C !C !C !C ^ !C ñ !C !C !C !C !C !C ^ !C ^ !C !C $ !C ^ !C !C !C !C !C !C ^ !C ^ ñ !C !C !C !C !C !C !C !C !C !C !C !C !. !C ^ ^ !C ñ !C !C !C !C !C $ !C !C ^ !C ^ !C !C !C ñ !C !C !C ^ !C !.ñ ñ!C !C !C !C ^ !C ^ !C ^ !C ^ !C !C !C !C !C !C !C !C ^ !C ñ !C !C !C !C !C ñ^ !C !C ñ !C !C !C !C !C !C !C !C !C !C !C !C ñ !C !C ^ ^ !C !C !C !. !C ñ ^!C ^ !C ñ!C !C ^ ^ !C !C $ ^ $!C ^ !C !C !C !C !C !C !C !C !C !C !C !C !. !C !.^ $ ñ !C !C !C ^ !C !C !C !C $ !C ^ !C !C $ !C !C ñ $ !. !C !C !C !C !C !C !. ^ ñ!C ^ ^ !C $!. ^ !C !C !C !C !C !C !C !C !C !C !C !C !C !. !C !C !C !C !C !C ^ !. !C !C ñ!C !C !C !C ^ñ !C !C ñ !C !C !. ^ !C !C !C !C !C !C !C ^ !C ñ ^ $ ^ !C ñ !C !. ñ!C ^ !C !. !C !C ^ ^ ñ !. !C !C $^ ^ñ ^ !C ^ ñ ^ ^ !C !C !C !C !C !C !C ^ !C !C !C !C !C !C !C !C !. !C ^ !C $ !. ñ!C !C !C ^ ñ!C. ^ !C !C !C !C !C !C !C !C $!C ^!. !. !. !C !C !C !. ^ !C !C ^ !C ^ !C !C ñ !C !. -

Profile: King Cetshwayo District
01/52 King Cetshwayo District 2 PROFILE: KING CETSHWAYO DISTRICT PROFILE: KING CETSHWAYO DISTRICT 3 CONTENTS 1. Executive Summary ........................................................................................... 5 2. Brief Overview .................................................................................................... 6 2.1. Historical Perspective ............................................................................................................... 6 2.2. Location .................................................................................................................................... 6 2.3. Spatial integration .................................................................................................................... 7 2.4. Land Ownership ....................................................................................................................... 7 3. Social Development Profile ............................................................................... 8 3.1. Key Social Demographics ......................................................................................................... 8 3.1.1. Population ............................................................................................................................. 8 3.1.2. Gender, Age and Race ........................................................................................................... 9 3.1.3. Household Profile ............................................................................................................... -

Women Crafters and Protected Areas in Kwazulu-Natal, South Africa AMY PANIKOWSKI
Woven Livelihoods: Women Crafters and Protected Areas in KwaZulu-Natal, South Africa AMY PANIKOWSKI From late April through June, I continued my fieldwork on the east coast of South Africa working with Zulu women and crafting materials. Every May, the iSimangaliso Wetland Park and Umlalazi Nature Reserve (every other May) allow women to harvest Juncus kraussii, a high quality reed mainly used for crafting bridal sleeping mats and traditional beer strainers. These items are valued in Zulu culture for their utilitarian properties as well as their cultural heritage. I interviewed individual crafters and crafting groups, most of which were women, about their harvesting and use of J. kraussii. Gaining insight into this economic oppor- tunity for a vulnerable population contrib- utes to the limited social research in and around these protected areas. In addition to on the financial, emotional, and physical ceremonies. My final stop was to interview this harvest, I also interviewed women who responsibilities of sustaining those in the women around Mbongolwane Wetland. I J. kraussii harvest iKhwani, which is like household unit. As a result, the need to quickly got a sense of how harvesting from but found in open-access wetlands within find alternative economic opportunities is this wetland works – seemingly no rules KwaZulu-Natal. I focused my research on greater in this population and can compro- on harvesting by community members and Mbongolwane Wetland, near Eshowe. mise their ability to support conservation those who come from afar. In South Africa, women head of protected areas. After spending time in these areas, almost half of all households because of First, I traveled to Umlalazi I have a better grasp of the interactions historical patterns of patriarchy, apartheid, Nature Reserve at Mtunzini where I had the between the protected areas, open-access macro-economic conditions, and HIV/ opportunity to meet with the community areas, and interacting community mem- AIDS. -

Ethembeni Cultural Heritage
PHASE 1 HERITAGE IMPACT ASSESSMENT REPORT: GINGINDLOVU TO MANDINI 132KV POWER LINE, uTHUNGULU DISTRICT MUNICIPALITY, KWAZULU-NATAL Prepared for Ludloko Developments cc Box 22964, Southgate Pietermaritzburg 3200 Telephone Edwin Ngidi 082 229 9502 Fax 086 570 8464 [email protected] Prepared by eThembeni Cultural Heritage Elizabeth Wahl and Len van Schalkwyk Box 20057 Ashburton 3213 Pietermaritzburg Telephone 033 326 1136 / 082 655 9077 / 082 529 3656 Facsimile 086 672 8557 [email protected] 15 December 2011 PHASE 1 HERITAGE IMPACT ASSESSMENT OF GINGINDLOVU TO MANDINI 132KV POWER LINE, KWAZULU-NATAL MANAGEMENT SUMMARY eThembeni Cultural Heritage was appointed by Ludloko Developments cc to undertake a Phase 1 Heritage Impact Assessment of a proposed power line upgrade between Gingindlovu and Mandini, as required by the National Environmental Management Act 107 of 1998 as amended, in compliance with Section 38 of the National Heritage Resources Act 25 of 1999 as amended. DESCRIPTION AND SIGNIFICANCE ASSESSMENT OF HERITAGE RESOURCES Virtually the entire proposed power line route is located within cultivated fields, dominated by sugar cane plantations. Places, buildings, structures and equipment Although we identified no buildings that constitute heritage resources within the proposed development area, we observed that the proposed power line immediately north of tower 10 traverses an occupied homestead. The servitude width for a 132 kV Sub-transmission line is 36m (18m on either side of the centre line of the power line) and no occupied residence is allowed within the servitude. Battlefields The proposed power line traverses the scenes of the Battles of Ndondakusuka and Gingindlovu, fought in 1856 and 1879, respectively.