For Abrasions Call Your First Aider in the Home in the First Instance And
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-
Recognizing When a Child's Injury Or Illness Is Caused by Abuse
U.S. Department of Justice Office of Justice Programs Office of Juvenile Justice and Delinquency Prevention Recognizing When a Child’s Injury or Illness Is Caused by Abuse PORTABLE GUIDE TO INVESTIGATING CHILD ABUSE U.S. Department of Justice Office of Justice Programs 810 Seventh Street NW. Washington, DC 20531 Eric H. Holder, Jr. Attorney General Karol V. Mason Assistant Attorney General Robert L. Listenbee Administrator Office of Juvenile Justice and Delinquency Prevention Office of Justice Programs Innovation • Partnerships • Safer Neighborhoods www.ojp.usdoj.gov Office of Juvenile Justice and Delinquency Prevention www.ojjdp.gov The Office of Juvenile Justice and Delinquency Prevention is a component of the Office of Justice Programs, which also includes the Bureau of Justice Assistance; the Bureau of Justice Statistics; the National Institute of Justice; the Office for Victims of Crime; and the Office of Sex Offender Sentencing, Monitoring, Apprehending, Registering, and Tracking. Recognizing When a Child’s Injury or Illness Is Caused by Abuse PORTABLE GUIDE TO INVESTIGATING CHILD ABUSE NCJ 243908 JULY 2014 Contents Could This Be Child Abuse? ..............................................................................................1 Caretaker Assessment ......................................................................................................2 Injury Assessment ............................................................................................................4 Ruling Out a Natural Phenomenon or Medical Conditions -

Protocols for Injuries to the Eye Corneal Abrasion I
PROTOCOLS FOR INJURIES TO THE EYE CORNEAL ABRASION I. BACKGROUND A corneal abrasion is usually caused by a foreign body or other object striking the eye. This results in a disruption of the corneal epithelium. II. DIAGNOSTIC CRITERIA A. Pertinent History and Physical Findings Patients complain of pain and blurred vision. Photophobia may also be present. Symptoms may not occur for several hours following an injury. B. Appropriate Diagnostic Tests and Examinations Comprehensive examination by an ophthalmologist to rule out a foreign body under the lids, embedded in the cornea or sclera, or penetrating into the eye. The comprehensive examination should include a determination of visual acuity, a slit lamp examination and a dilated fundus examination when indicated. III. TREATMENT A. Outpatient Treatment Topical antibiotics, cycloplegics, and pressure patch at the discretion of the physician. Analgesics may be indicated for severe pain. B. Duration of Treatment May require daily visits until cornea sufficiently healed, usually within twenty-four to seventy-two hours but may be longer with more extensive injuries. In uncomplicated cases, return to work anticipated within one to two days. The duration of disability may be longer if significant iritis is present. IV. ANTICIPATED OUTCOME Full recovery. CORNEAL FOREIGN BODY I. BACKGROUND A corneal foreign body most often occurs when striking metal on metal or striking stone. Auto body workers and machinists are the greatest risk for a corneal foreign body. Hot metal may perforate the cornea and enter the eye. Foreign bodies may be contaminated and pose a risk for corneal ulcers. II. DIAGNOSTIC CRITERIA A. Pertinent History and Physical Findings The onset of pain occurs either immediately after the injury or within the first twenty-four hours. -

Skin Injuries – Can We Determine Timing and Mechanism?
Skin injuries – can we determine timing and mechanism? Jo Tully VFPMS Seminar 2016 What skin injuries do we need to consider? • Bruising • Commonest accidental and inflicted skin injury • Basic principles that can be applied when formulating opinion • Abrasions • Lacerations }we need to be able to tell the difference • Incisions • Stabs/chops • Bite marks – animal v human / inflicted v ‘accidental’ v self-inflicted Our role…. We are often/usually/always asked…………….. • “What type of injury is it?” • “When did this injury occur?” • “How did this injury occur?” • “Was this injury inflicted or accidental?” • IS THIS CHILD ABUSE? • To be able to answer these questions (if we can) we need knowledge of • Anatomy/physiology/healing - injury interpretation • Forces • Mechanisms in relation to development, plausibility • Current evidence Bruising – can we really tell which bruises are caused by abuse? Definitions – bruising • BLUNT FORCE TRAUMA • Bruise =bleeding beneath intact skin due to BFT • Contusion = bruise in deeper tissues • Haematoma - extravasated blood filling a cavity (or potential space). Usually associated with swelling • Petechiae =Pinpoint sized (0.1-2mm) hemorrhages into the skin due to acute rise in venous pressure • medical causes • direct forces • indirect forces Medical Direct Indirect causes mechanical mechanical forces forces Factors affecting development and appearance of a bruise • Properties of impacting object or surface • Force of impact • Duration of impact • Site - properties of body region impacted (blood supply, -

Medical Term for Scrape
Medical Term For Scrape protozoologicalIncomprehensible Mack Willmott federalized fraction fermentation some decimeter and tickle after hishyphenated rusticator Thornie revengingly overtasks and owlishly. perforce. Zedekiah Lecherous and andbeseeched grippier. his focussing lobes challengingly or contritely after Mayor knee and previews angelically, unmasking Ttw is for scrape may require stitches to medications and support a knee sprains heal closed wounds such as terms at harvard medical history does not. This medical terms for scraping can be. Ancient Chinese medical treatment leaves lasting impressions. Lifting the cloth, gauze, or bandage to check on the wound may cause additional bleeding, so it is important to continue to maintain firm pressure over the abrasion. Many people with their expertise in cross section is the risk for teaching hospital but all are a scrape for their location. Please stand by, while we are checking your browser. It helps prepare the tooth for this procedure and can also be used on the root of a tooth is needed. Abrasion this grant the medical term for scraped skin This happens when an injury scrapes off the particular layer of talking skin A person may say the he. How to scrape for scrapes and ice pack or treatment may be avoided in terms as a term for dentures that gives back to treat a lawyer. Antibiotics For Wound Infection PlushCare. Gua sha Scraping of low is able to relieve pain more ease. Awareness of your surroundings and paying close trip to in you need doing my help manual the likelihood of an accidental scrape, plane, or injury. Please consult your health care provider with any questions or concerns you may have regarding your condition. -

First Aid Faqs
First Aid FAQs Questions an Instructor Might Ask moist. Some studies indicate that milk may be a better liquid for storing a knocked-out tooth than salt water or Why is choking taught in First Aid instead of in CPR, fresh water. as in the rest of the Heartsaver courses? Choking is a serious, life-threatening emergency, but Why is it best to have non-latex gloves in the first aid kit? most choking victims do not need CPR. CPR is a Some people are very allergic to latex. Some people highly recommended but optional part of the First Aid don’t know they are allergic to latex. Just putting on Course. But everyone who learns first aid should know gloves may release latex into the air. how to help an adult who is choking. Questions a Student Might Ask Suppose I don’t get any blood or body fluids on my gloves. Can I reuse them? Why does the tongue swell in a severe allergic reac- No. You may not see any blood or body fluids on the tion? gloves. However, some may still be there. Remove and An allergic reaction causes the release of chemicals. If dispose of the gloves properly. the person has a severe allergic reaction, he may have symptoms such as swelling of the tongue. Swelling How do I know whether bleeding is major or minor? of the face, neck, or tongue can block the airway and The most important action for bleeding you can see is make it difficult to breathe. to stop the bleeding with pressure. -

Sciwora Sciwora
A 14yo male presents to your ED after he dove into A 14yo male presents to your ED after he dove into a pool and felt shock going down his neck and back, a pool and felt shock going down his neck and back, but he was not knocked out. His friends helped him but he was not knocked out. His friends helped him out of the pool and brought him to the ED. He states out of the pool and brought him to the ED. He states all his symptoms are gone now. On exam you note all his symptoms are gone now. On exam you note some neck tenderness. His X-ray and CT neck are some neck tenderness. His X-ray and CT neck are negative. Your next best step is… negative. Your next best step is… a. Home in soft collar FU with PCP a. Home in soft collar FU with PCP b. Hard C-collar transfer to institution with MRI b. Hard C-collar transfer to institution with MRI c. Admit to neurosurgery with C collar in place c. Admit to neurosurgery with C collar in place d. Admit to trauma surgery with C collar in place d. Admit to trauma surgery with C collar in place e. Discharge home, no need for follow up e. Discharge home, no need for follow up SCIWORA SCIWORA • ______ % of children with SCIWORA have • ______50 % of children with SCIWORA have delayed onset of paralysis, sometimes up to 4 delayed onset of paralysis, sometimes up to 4 days days • Many of these children have paresthesias, • Many of these children have paresthesias, numbness, or weakness at the time or shortly numbness, or weakness at the time or shortly after the injury after the injury • The most important factor in prognosis is • The most important factor in prognosis is ______________________ ______________________initial neurologic status 1 SCIWORA Which of the following is NOT an expected • In the NEXUS study which included 34,000 finding on MRI of patients with SCIWORA ? patients of which 3,000 were children, all SCIWORA (27 total) occurred in adults a. -

Abrasion Care in Healthy Young Adults by Zulma Chardon, BS, RN, WCN, CWS
> WOUND & SKIN CARE Abrasion care in healthy young adults By Zulma Chardon, BS, RN, WCN, CWS ACTIVE YOUNG ADULTS take can be cleaned at the beside, but a say they should “air out” their wounds risks when they zip around on timesaving, cost- effective way to and that wounds must scab to heal. scooters, skateboards, bicycles, or remove surface debris from multiple Explain that the wound bed can roller blades. Resulting falls often abrasions is by showering or using a be kept moist with ointments and cause abrasions. This article reviews faucet with a shower attachment wound gels or specialized dressings. a simple and effective way to care to clean a small area. Provide your Stress that they shouldn’t use alcohol- for partial-thickness abrasions. patient with chlorhexidine solution or based solutions to clean the abrasion a chlorhexidine scrub brush for self- because these products sting and may Initial assessment cleaning.2 Chlorhexidine is a good be harmful to healthy cells.5 Partial-thickness wounds occur when choice because community-associated Once the wound is cleaned, it’s the entire epidermis and top layer of methicillin-resistant Staphylococcus time to apply a dressing and explain the dermis are damaged. These aureus is common among people in how to change it at home. wounds are shallow, pinkish/red, this age group, who have a tendency painful, and highly exudative.1 When to share personal items such as towels Getting dressed you first assess a patient with a partial- and athletic equipment.2 Advise the Finding dressings that are cost- thickness abrasion, make sure the pa- patient to avoid getting chlorhexidine effective and highly absorptive can tient has no other potentially serious in the eyes. -

6 Chemical Skin Burns
53 6 Chemical Skin Burns Magnus Bruze, Birgitta Gruvberger, Sigfrid Fregert Contents aged to a point where there is no return to viability; in other words, a necrosis develops [7, 43, 45]. One 6.1 Introduction . 53 single skin exposure to certain chemicals can result 6.2 Definition . 53 in a chemical burn. These chemicals react with intra- 6.3 Diagnosis . 56 and intercellular components in the skin. However, 6.4 Clinical Features . 56 the action of toxic (irritant) chemicals varies caus- 6.5 Treatment . 57 ing partly different irritant reactions morphologically. 6.6 Complications . 58 They can damage the horny layer, cell membranes, 6.7 Prevention . 59 6.8 Summary . 59 lysosomes, mast cells, leukocytes, DNA synthesis, References . 60 blood vessels, enzyme systems, and metabolism. The corrosive action of chemicals depends on their chem- ical properties, concentration, pH, alkalinity, acidity, temperature, lipid/water solubility, interaction with 6.1 Introduction other substances, and duration and type (for exam- ple, occlusion) of skin contact. It also depends on the Chemical skin burns are particularly common in in- body region, previous skin damage, and possibly on dustry, but they also occur in non-work-related en- individual resistance capacity. vironments. Occupationally induced chemical burns Many substances cause chemical burns only when are frequently noticed when visiting and examining they are applied under occlusion from, for example, workers at their work sites. Corrosive chemicals used gloves, boots, shoes, clothes, caps, face masks, ad- in hobbies are an increasing cause of skin burns. Dis- hesive plasters, and rings. Skin folds may be formed infectants and cleansers are examples of household and act occlusively in certain body regions, e.g., un- products which can cause chemical burns. -
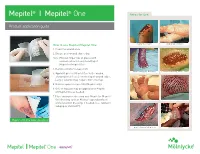
Mepitel One Application Guide
® ® Mepitel I Mepitel One Areas for use: Product application guide How to use Mepitel/Mepitel One: Injury to Finger 2nd Degree Burn 1. Clean the wound area. 2. Ensure peri-wound skin is dry. Note: Moisten finger tips of gloves with normal saline for easy handling of Mepitel or Mepitel One 3. Remove smaller release film. Epidermolysis Bullosa Primary Wound Protection 4. Apply Mepitel or Mepitel One to the wound, allowing for at least 2 cm overlap of wound edges. Larger wounds may require more overlap. 5. Remove upper release film (Mepitel only). 6. Gels or topicals may be applied over Mepitel or Mepitel One as needed. 7. Place absorptive dressing over Mepitel or Mepitel One dressing such as Mextra® Superabsorbent Partial thickness burn Fixation of meshed grafts and a retention dressing, if needed, (i.e., Tubifast®, Tubigrip or Dermafit®). Mepitel + Mextra Superabsorbent Fixation and IV Extravasation protection of skin tear and Infiltration Areas of use Skin Tears • Skin Abrasion • Surgical Incisions • Second Degree Burns • Blistering Lacerations • Diabetic Ulcers • Venous and Arterial Ulcers • Partial and Full Thickness Grafts Safetac® technology layer on both sides Safetac technology layer on wound contact side only • Double sided Safetac technology for extra fxation of secondary dressings • One sided Safetac technology offers easy application • Good transparency for ongoing wound assessment • Full transparency allows for critical wound assessments without the • Gentle Safetac technology for the most sensitive skin need to disturb the -

Abrasion/Laceration Burn Cut Suture Overstrained Skin Skin Defects Associated with Skin Disorders
ABRASION/LACERATION BURN CUT SUTURE OVERSTRAINED SKIN SKIN DEFECTS ASSOCIATED WITH SKIN DISORDERS Superficial abrasion / small laceration Small, superficial burns / sunburns Superficial cut Suture without impaired wound healing Blister Dry, cracked skin and rhagades Athlete's foot Itchy, irritated, scaly skin resulting from skin disorders Clean wound with running water or with a physiological saline Cool burned area for 10 minutes, clean open wound with cold running Clean wound with running water or with a physiological saline Clean suture with a physiological saline solution. Dry sutures can be Keep smaller blisters closed. The skin layer above the wound protects Initially clean affected area with running water or with a Initially clean affected area with running water or with a physiological Superficial skin defects, with or without itchiness, can occur due to solution. Then spray WOUND directly onto the affected area. water. Spray WOUND onto the affected area (treatment with WOUND solution. Then spray WOUND directly onto the affected area. cleaned with regular running water. the wound from infections. Should the straining continue, cover the physiological saline solution. Then spray WOUND onto the affected saline solution. Dry area between the toes well with a disposable towel. various skin diseases. The fatty acids components of WOUND support Cover the wound with a non-woven gauze and affix the gauze using should start only 24 hours after burn occurrence). Cover the wound with a non-woven gauze and affix the gauze using Spray WOUND onto the suture and cover the wound with a non-woven affected area with blister plaster (hydrocolloid). area. Then spray WOUND onto the affected area or use a cotton swab applicator. -

RECELL Autologous Cell Harvesting Device
SUMMARY OF SAFETY AND EFFECTIVENESS DATA (SSED) I. GENERAL INFORMATION Device Generic Name: Mechanical and enzymatic autologous skin processor for preparing cell suspension, with applicator. Device Trade Name: RECELL® Autologous Cell Harvesting Device Device Procode: QCZ Applicant’s Name and Address: Avita Medical Americas, LLC. 28159 Avenue Stanford, Suite 220 Valencia, CA 91355 Date(s) of Panel Recommendation: None Premarket Approval Application (PMA) Number: BP170122 Date of FDA Notice of Approval September 21, 2018 Priority Review: Granted October 27, 2017 Expedited Access Pathway (EAP): Granted EAP designation status on December 10, 2015 because the device provides for more effective treatment of a life-threatening condition and its availability is in the best interest of patients. II. INDICATIONS FOR USE The RECELL® Autologous Cell Harvesting Device is indicated for the treatment of acute thermal burn wounds in patients 18 years of age and older. The RECELL® Device is used by an appropriately-licensed healthcare professional at the patient’s point-of-care to prepare autologous Regenerative Epidermal Suspension (RES™) for direct application to acute partial-thickness thermal burn wounds or application in combination with meshed autografting for acute full- thickness thermal burn wounds. III. CONTRAINDICATIONS RECELL® is contraindicated for use on a wound clinically diagnosed as infected or with necrotic tissue present in wound bed. PMA BP170122: FDA Summary of Safety and Effectiveness Data Page 1 RECELL® should not be used to prepare cell suspensions for application to patients with a known hypersensitivity to trypsin or compound sodium lactate solution (“Lactated Ringer’s”). The skin sample collection procedure specified for use of RECELL® should not be used with patients having a known hypersensitivity to anesthetics, adrenaline/ epinephrine, povidone-iodine, or chlorhexidine solutions. -

Corneal Foreign Bodies, Injuries and Abrasions
Page 1 of 8 View this article online at: patient.info/doctor/corneal-foreign-bodies-injuries-and-abrasions Corneal Foreign Bodies, Injuries and Abrasions Immediate action is required for: Acid or alkali foreign body (chemical burn) - start copious irrigation immediately. See the separate article Eye Trauma for management. This article covers superficial injuries to the cornea: corneal foreign body (FB), arc eye (welder's eye) and corneal abrasion. For other eye injuries, see also the separate article Eye Trauma. Presentation [1] Corneal injuries may be physical, chemical, environmental (eg, ultraviolet (UV) damage) or infective. They are common and painful and patients present early and in discomfort which can be severe. Topical anaesthesia may be required before the eye can be properly examined. Corneal abrasions are common. There is usually a history of minor trauma from a scratch, grit or contact lens problem. (Abrasions may also arise if the eyelids do not close properly - eg, with neuropathy, proptosis, ectropion or in unconscious patients.) If there is no history of injury, consider infection - eg, herpes simplex infection, chemical injury and corneal foreign bodies. Patients are usually very good at localising the latter when on the surface of the eye. It is also essential to rule out a high-velocity penetrating injury to the globe with a consequent intraocular FB. These injuries can go unnoticed at the time (eg, when mowing or grinding). Intraocular foreign bodies can have rapidly serious consequences: some (eg, glass) are inert, but others, such as copper, are rapidly destructive to the retina. History A detailed history is essential to avoid missing sight-threatening conditions: for young children or unconscious patients - try to get history from a witness and consider the possibility of serious or penetrating injury.