Effect of Behaviour Change Communication on Iodised Salt
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Districts of Ethiopia
Region District or Woredas Zone Remarks Afar Region Argobba Special Woreda -- Independent district/woredas Afar Region Afambo Zone 1 (Awsi Rasu) Afar Region Asayita Zone 1 (Awsi Rasu) Afar Region Chifra Zone 1 (Awsi Rasu) Afar Region Dubti Zone 1 (Awsi Rasu) Afar Region Elidar Zone 1 (Awsi Rasu) Afar Region Kori Zone 1 (Awsi Rasu) Afar Region Mille Zone 1 (Awsi Rasu) Afar Region Abala Zone 2 (Kilbet Rasu) Afar Region Afdera Zone 2 (Kilbet Rasu) Afar Region Berhale Zone 2 (Kilbet Rasu) Afar Region Dallol Zone 2 (Kilbet Rasu) Afar Region Erebti Zone 2 (Kilbet Rasu) Afar Region Koneba Zone 2 (Kilbet Rasu) Afar Region Megale Zone 2 (Kilbet Rasu) Afar Region Amibara Zone 3 (Gabi Rasu) Afar Region Awash Fentale Zone 3 (Gabi Rasu) Afar Region Bure Mudaytu Zone 3 (Gabi Rasu) Afar Region Dulecha Zone 3 (Gabi Rasu) Afar Region Gewane Zone 3 (Gabi Rasu) Afar Region Aura Zone 4 (Fantena Rasu) Afar Region Ewa Zone 4 (Fantena Rasu) Afar Region Gulina Zone 4 (Fantena Rasu) Afar Region Teru Zone 4 (Fantena Rasu) Afar Region Yalo Zone 4 (Fantena Rasu) Afar Region Dalifage (formerly known as Artuma) Zone 5 (Hari Rasu) Afar Region Dewe Zone 5 (Hari Rasu) Afar Region Hadele Ele (formerly known as Fursi) Zone 5 (Hari Rasu) Afar Region Simurobi Gele'alo Zone 5 (Hari Rasu) Afar Region Telalak Zone 5 (Hari Rasu) Amhara Region Achefer -- Defunct district/woredas Amhara Region Angolalla Terana Asagirt -- Defunct district/woredas Amhara Region Artuma Fursina Jile -- Defunct district/woredas Amhara Region Banja -- Defunct district/woredas Amhara Region Belessa -- -

Download E-Book (PDF)
Journal of Public Health and Epidemiology Volume 9 Number 6 June 2017 ISSN 2141-2316 ABOUT JPHE The Journal of Public Health and Epidemiology (JPHE) is published monthly (one volume per year) by Academic Journals. Journal of Public Health and Epidemiology (JPHE) is an open access journal that provides rapid publication (monthly) of articles in all areas of the subject such as health observatory, biostatistics, occupational health, behavioral medicine etc. The Journal welcomes the submission of manuscripts that meet the general criteria of significance and scientific excellence. Papers will be published shortly after acceptance. All articles published in JPHE are peer-reviewed. Contact Us Editorial Office: [email protected] Help Desk: [email protected] Website: http://www.academicjournals.org/journal/JPHE Submit manuscript online http://ms.academicjournals.me/ Editors Professor Mostafa A. Abolfotouh Professor of Family & Community Medicine Head of Medical Team - Biobanking Section. King Abdullah International Medical Research CEnter, King Saud Bin-Abdulaziz University for Health Sciences, National Guard Health Affairs, Saudi Arabia Editorial Board Dr. Guolian Kang Prof. Tariq Javed The University of Alabama at Birmingham/1665 Department of Pathology, Faculty of Veterinary Science, University Blvd, Ryals 443 University of Agriculture, Faisalabad-38040. Guolian Pakistan. USA Dr. María Elena Dávila L Universidad Centroccidental “Lisandro Alvarado”. Dr. Mohammed Danlami Salihu School of Medicine/ School of Health Science . Av. Public Health Department Andrés Bello C/ Av. Libertador. Barquisimeto, Lara, Faculty of Veterinary Medicine Venezuela, SA Usmanu Danfodiyo University, Sokoto. Nigeria. Dr. Lay Ching Chai Centre of Excellence for Food Safety Research, Faculty of Prof. Jahanfar Jahanban Food Science and Technology, Universiti Putra Malaysia, Oral Pathology Dept.Dental faculty of Tehran Islamic 43400 UPM Serdang, Selangor, Azad University/ Malaysia Address:B 107 Pezeshkan-Farabi Build No 67 Javanshir St. -

D.Table 9.5-1 Number of PCO Planned 1
D.Table 9.5-1 Number of PCO Planned 1. Tigrey No. Woredas Phase 1 Phase 2 Phase 3 Expected Connecting Point 1 Adwa 13 Per Filed Survey by ETC 2(*) Hawzen 12 3(*) Wukro 7 Per Feasibility Study 4(*) Samre 13 Per Filed Survey by ETC 5 Alamata 10 Total 55 1 Tahtay Adiyabo 8 2 Medebay Zana 10 3 Laelay Mayechew 10 4 Kola Temben 11 5 Abergele 7 Per Filed Survey by ETC 6 Ganta Afeshum 15 7 Atsbi Wenberta 9 8 Enderta 14 9(*) Hintalo Wajirat 16 10 Ofla 15 Total 115 1 Kafta Humer 5 2 Laelay Adiyabo 8 3 Tahtay Koraro 8 4 Asegede Tsimbela 10 5 Tselemti 7 6(**) Welkait 7 7(**) Tsegede 6 8 Mereb Lehe 10 9(*) Enticho 21 10(**) Werie Lehe 16 Per Filed Survey by ETC 11 Tahtay Maychew 8 12(*)(**) Naeder Adet 9 13 Degua temben 9 14 Gulomahda 11 15 Erob 10 16 Saesi Tsaedaemba 14 17 Alage 13 18 Endmehoni 9 19(**) Rayaazebo 12 20 Ahferom 15 Total 208 1/14 Tigrey D.Table 9.5-1 Number of PCO Planned 2. Affar No. Woredas Phase 1 Phase 2 Phase 3 Expected Connecting Point 1 Ayisaita 3 2 Dubti 5 Per Filed Survey by ETC 3 Chifra 2 Total 10 1(*) Mile 1 2(*) Elidar 1 3 Koneba 4 4 Berahle 4 Per Filed Survey by ETC 5 Amibara 5 6 Gewane 1 7 Ewa 1 8 Dewele 1 Total 18 1 Ere Bti 1 2 Abala 2 3 Megale 1 4 Dalul 4 5 Afdera 1 6 Awash Fentale 3 7 Dulecha 1 8 Bure Mudaytu 1 Per Filed Survey by ETC 9 Arboba Special Woreda 1 10 Aura 1 11 Teru 1 12 Yalo 1 13 Gulina 1 14 Telalak 1 15 Simurobi 1 Total 21 2/14 Affar D.Table 9.5-1 Number of PCO Planned 3. -

(Tor) Assessment of Production, Economic and Social Impact of Interventions with Innovations on Selected Fa
Terms of Reference (ToR) Assessment of production, economic and social impact of interventions with Innovations on selected farms with wheat and faba bean production in Arsi 1. Background Ethiopia has very diverse bio-physical environment with a variety of ecosystems, with significant differences in climate, soil properties, vegetation types, agricultural potential, biodiversity and water resources. That results in different farming systems and farming products. The crop subsector which, on average, accounted for about 30 percent of GDP has been the major contributor to the growth of the agricultural value added during the period of the GTP (Growth and Transformation Plan). The productivity of major food crops (Cereals, Pulses, and Oil seeds) reached an annual average level of 17.6 quintal (100 kg) per hectare. Further increase in production and productivity of major crops will continue to be a priority in the next five years (2016-2020) by fully implementing strategies such as delivering effective extension services, supplying agricultural inputs and conducting famers training. The participation of several actors like international partners and private business will be encouraged and supported as well by the government. In general, during the period of the second Growth and Transformation Plan, objectives are broadly set in terms of increasing crop and livestock production and productivity, promoting natural resource conservation and utilization, ensuring food security and disaster prevention and preparedness. In this regard, the German -
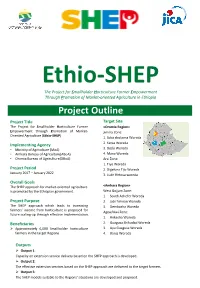
Ethio-SHEP Project Outline
Ethio-SHEP The Project for Smallholder Horticulture Farmer Empowerment Through Promotion of Market-oriented Agriculture in Ethiopia Project Outline Project Title Target Site The Project for Smallholder Horticulture Farmer <Oromia Region> Empowerment through Promotion of Market- Jimma Zone: Oriented Agriculture (Ethio-SHEP) 1. Seka chokorsa Woreda Implementing Agency 2. Kersa Woreda • Ministry of Agriculture (MoA) 3. Dedo Woreda • Amhara Bureau of Agriculture(ABoA) 4. Mana Woreda • Oromia Bureau of Agriculture(OBoA) Arsi Zone: 1. Tiyo Woreda Project Period 2. Digeluna Tijo Woreda January 2017 – January 2022 3. Lude Hetosa woreda Overall Goals The SHEP approach for market-oriented agriculture <Amhara Region> is promoted by the Ethiopian government. West Gojjam Zone: 1. South Achefer Woreda Project Purpose 2. Jabi Tehnan Woreda The SHEP approach which leads to increasing 3. Dembacha Woreda farmers' income from horticulture is proposed for Agew/Awi Zone: future scaling-up through effective implementation. 1. Ankesha Woreda Beneficiaries 2. Guagusa Shikudad Woreda ➢ Approximately 6,000 Smallholder horticulture 3. Ayu Guagusa Woreda farmers in the target Regions 4. Banja Woreda Outputs ➢ Output 1: Capacity on extension service delivery based on the SHEP approach is developed. ➢ Output 2: The effective extension services based on the SHEP approach are delivered to the target farmers. ➢ Output 3: The SHEP models suitable to the Regions' situations are developed and proposed. Concept of SHEP Approach Promoting “Farming as a Business” Empowering and motivating people Sharing information among market actors & farmers for Three psychological needs to motivate people improving efficiency of local economies Autonomy Market Info. People need to feel in control of (variety, price, Market their own behaviors and goals season, etc.) Family budgeting Survey by Farmers farmers Competence Sharing SHEP People need to gain mastery market Linkage of tasks and learn different information forum skills Relatedness Market actors Producer Info. -

Median Urinary Iodine Concentration and Associated Factors Among Children Age 6 to 59 Months in Central Highland of Ethiopia
Research Article ISSN: 2574 -1241 DOI: 10.26717/BJSTR.2019.17.003026 Median Urinary Iodine Concentration and Associated Factors Among Children Age 6 to 59 Months in Central Highland of Ethiopia Abebe Ferede*1, Muluemebet Abera2 and Tefera Belachew2 1.Arsi University, College of Health Science, Department of Public Health, Asella, Ethiopia 2.Jimma University, Faculty of Public Health, Department of Population and Family Health, Jimma, Ethiopia *Corresponding author: Abebe Ferede, Arsi University, College of Health Science, Department of Public Health, Asella, Ethiopia ARTICLE INFO abstract Received: April 20, 2019 Introduction: Mid Urine Iodine Concentration (MUIC) is one of the biomarkers Published: April 29, 2019 that are typically used to measure the concentration of iodide found in plasma thyroxin Citation: Abebe Ferede, Muluemebet level. This study aimed to assess MUIC and associated factors among children age 6 to 59 in human being and used to predict the risk of Iodine nutrient deficiency at population Abera, Tefera Belachew. Median Urinary months in the Central highland area of Ethiopia after an over a decade of intervention of Iodine Concentration and Associated with iodized salt by Ethiopian Government. Factors Among Children Age 6 to 59 Methods: Community-based cross-sectional study was applied with multistage Months in Central Highland of Ethiopia. sampling method to select individual household (HH) and correspondent mothers/ Biomed J Sci & Tech Res 17(4)-2019. caregivers with their pair children age 6 to 59 months according to the proportion of BJSTR. MS.ID.003026. population found in each Keble (small administrative unit). Collected samples of mid urine Abbreviations: MUIC: Mid Urine Io- specimens taken from selected children were transferred to and stored in laboratory with dine Concentration; HH: Household; great percussion. -

Woreda-Level Crop Production Rankings in Ethiopia: a Pooled Data Approach
Woreda-Level Crop Production Rankings in Ethiopia: A Pooled Data Approach 31 January 2015 James Warner Tim Stehulak Leulsegged Kasa International Food Policy Research Institute (IFPRI) Addis Ababa, Ethiopia INTERNATIONAL FOOD POLICY RESEARCH INSTITUTE The International Food Policy Research Institute (IFPRI) was established in 1975. IFPRI is one of 15 agricultural research centers that receive principal funding from governments, private foundations, and international and regional organizations, most of which are members of the Consultative Group on International Agricultural Research (CGIAR). RESEARCH FOR ETHIOPIA’S AGRICULTURE POLICY (REAP): ANALYTICAL SUPPORT FOR THE AGRICULTURAL TRANSFORMATION AGENCY (ATA) IFPRI gratefully acknowledges the generous financial support from the Bill and Melinda Gates Foundation (BMGF) for IFPRI REAP, a five-year project to support the Ethiopian ATA. The ATA is an innovative quasi-governmental agency with the mandate to test and evaluate various technological and institutional interventions to raise agricultural productivity, enhance market efficiency, and improve food security. REAP will support the ATA by providing research-based analysis, tracking progress, supporting strategic decision making, and documenting best practices as a global public good. DISCLAIMER This report has been prepared as an output for REAP and has not been reviewed by IFPRI’s Publication Review Committee. Any views expressed herein are those of the authors and do not necessarily reflect the policies or views of IFPRI, the Federal Reserve Bank of Cleveland, or the Board of Governors of the Federal Reserve System. AUTHORS James Warner, International Food Policy Research Institute Research Coordinator, Markets, Trade and Institutions Division, Addis Ababa, Ethiopia [email protected] Timothy Stehulak, Federal Reserve Bank of Cleveland Research Analyst, P.O. -

Dairy Products in the Agro-Commodities Procurement Zone of the Pilot Integrated Agro-Industrial Park in Central-Eastern Oromia, Ethiopia
Strategic analysis and intervention plan for cow milk and dairy products in the Agro-Commodities Procurement Zone of the pilot Integrated Agro-Industrial Park in Central-Eastern Oromia, Ethiopia Project UNJP/ETH/092/UID Technical Support for the Implementation of an Integrated Agro-Industrial Park (IAIP) in Ethiopia Strategic analysis and intervention plan for cow milk and dairy products in the Agro-Commodities Procurement Zone of the pilot Integrated Agro-Industrial Park in Central-Eastern Oromia, Ethiopia Filippo Brasesco FAO Agribusiness Officer Desta Asgedom Senior National Value Chain Expert Valentina Sommacal International Gender/Value Chain Expert FOOD AND AGRICULTURE ORGANIZATION OF THE UNITED NATIONS Addis Ababa, 2019 Required citation: Brasesco, F., Asgedom, D., Sommacal, V. 2019. Strategic analysis and intervention plan for cow milk and dairy products in the Agro-Commodities Procurement Zone of the pilot Integrated Agro-Industrial Park in Central-Eastern Oromia, Ethiopia. Addis Ababa, FAO. 116 pp. Licence: CC BY-NC-SA 3.0 IGO. The designations employed and the presentation of material in this information product do not imply the expression of any opinion whatsoever on the part of the Food and Agriculture Organization of the United Nations (FAO) concerning the legal or development status of any country, territory, city or area or of its authorities, or concerning the delimitation of its frontiers or boundaries. The mention of specific companies or products of manufacturers, whether or not these have been patented, does not imply that these have been endorsed or recommended by FAO in preference to others of a similar nature that are not mentioned. The views expressed in this information product are those of the author(s) and do not necessarily reflect the views or policies of FAO. -
Urban Water Supply Universal Access Plan.Pdf
Federal Democratic Republic of Ethiopia Ministry of Water and Energy PART III Urban Water Supply Universal Access Plan (UWSPUAP) 2011-2015 December 2011 Addis Ababa 1 URBAN WATER SUPPLY UAP Table of Contents Executive Summary .............................................................................................................................................. 1 1. Introduction ................................................................................................................................................... 2 2. Background ................................................................................................................................................... 2 3. The Urban UAP model and Assumptions ..................................................................................................... 4 4. Sector policy and Strategy ............................................................................................................................. 7 5. Cross cutting Issues ..................................................................................................................................... 10 6. Physical Plan ............................................................................................................................................... 10 7. Financial Plan .............................................................................................................................................. 12 7.1. Financial plan for Project Implementation ......................................................................................... -
Explanatory Notes
GEOLOGICAL HAZARDS AND ENGINEERING GEOLOGY MAPS OF HOSAINA NB 37-2 EXPLANATORY NOTES Debebe Nida and Yekoye Bizuye (Compilers) Vladislav Rapprich (Editor) The Main Project Partners The Czech Development Agency (CzDA) cooperates with the Ministry of Foreign Affairs on the establishment of an institutional framework of Czech development cooperation and actively participates in the creation and financing of development cooperation programs between the Czech Republic and partner countries. www.czda.cz The Geological Survey of Ethiopia (GSE) is accountable to the Ministry of Mines and Energy, collects and assesses geology, geological engineering and hydrogeology data for publication. The project beneficiary. www.gse.gov.et The Czech Geological Survey collects data and information on geology and processes it for political, economical and environmental management. The main contractor. www.geology.cz AQUATEST a.s. is a Czech consulting and engineering company in water management and environmental protection. The main aquatest subcontractor. www.aquatest.cz Copyright © 2014 Czech Geological Survey, Klarov 3, 118 21 Prague 1, Czech Republic First edition AcknowledgmentAcknowledgment Fieldwork and primary compilation of the map and explanatory notes was done by a team from the Geological Survey of Ethiopia (GSE) consisting of staff from the Geo Hazard Investigation Directorate, Groundwater Resources Assessment Directorate and Czech experts from AQUATEST a.s. and the Czech Geological Survey in the framework of the Czech Development Cooperation Program. We would like to thank the SNNPR Regional Water Bureau, the Dila, Sidamo and Sodo- Woleita Zone Administrations, Water, Mines and Energy offices for their hospitality, guidance and relevant data delivery. The team is grateful to the management of the Geological Survey of Ethiopia, particularly to Director General (GSE) Mr. -

REPUBLIC of SOUTH SUDAN SOMALIA UGANDA DJIBOUTI KENYA YEMEN ETHIOPIA ERITREA SUDAN Djibouti Asmara Addis Ababa
! ACT Alliance Ethiopia Operational Map January 2018 ! ! Asmara Sanaa ERITREA R Tahitay Adiyabo v® Zalambesa Dawuhan Gerihu Sernay ! ! E Laelay ! Erop Shiraro Rama v® Gulo ! Adiabo ! !( Meheda Erop D v® v® Mereb Leha Ê Ahiferom Dalol HumeÊ®ra North Westernv® Humer!va Town v® Chasa ! Bazev®t!Adi Gir!at Town Adwa Adkuwa Tigray !( ! Dalol Adwa Town Ganta Afeshum! EDEGA HAMUS Tahitay Qoraro ! ! v®! v® Saesi Tsadamba S v®! Akisuvm Town Nebelat ! n Selekileha Ê Berehale Qafta Humera Shire Atsbi Enida We!(reilehi H!(awzen TIGRAY Asegede Tahitay ! Wonberta! YEMEN n E Silase Western Tsimbila Maychew Hawzen KonÊaba Central Atsbi Endasilasie ! Not Covered Medebay Nader ñ ! Berahile Tigray Mezega Tigray !( Ê Konaba by Field Work A ! Zana Adet ! Wekero Welqayet v® Klite n Kola Temben Hagere Sñelam Awlalo ! ! Ê Tselemt Abiyi adi Degua Tsegede ! May Tsebri d ÊDebuvb® & Abrha jara Temben SÊe!men MIrab ! Adi Arikay v® v®v® ! Abala Armacho Tselemet Tanqua !Mekele Ê Zone 02 Adiarikay Tselemt Sehart$i SUDAN Abeñrgele Samre Enderta ! Ê Not Covered Adiarikay Beyeda ! Ê Tegede Gijet Abala Lakora v® Adiarikay $ ! Afdera by Field Work ! ® d Afdera ! Dvebark $ Hintalo ! Debarq Jan Dil Yibza Abergele South ! Wajirat Erebti Amora Ê Ê Assab Tach Armacho Tigray ! Dabat ! Mekane Berhan Aden Metema Sanja ! ! v® Dabat $ ! Ambalage v® Gedebge Sehale Seyemt Abergele Ê Megale Chilga Alibuko ! Sehal$e ! Metema Ê Seyemt $ ! Lay ! Wag Himra ! Lile Chlga ! Wv®egera Tsitsika Maychew Town ² Chilga ® Armvachew ZIKWALA Sekota v® $ Ofla Rya ®Gondar Sek!ota Endamehone Teru Gondvar -

Effect of Nutrition Behaviour Change Intervention on Improving
Integrative Food, Nutrition and Metabolism Research Article ISSN: 2056-8339 Effect of nutrition behaviour change intervention on improving micronutrients concentration and linear growth of children age 6 to 59 months in central highland of Ethiopia: Cluster randomized control trial Abebe Ferede1*, Tefera Belachew2 and Muluemebet Abera3 1Department of Public Health, College of Health Science, Arsi University, Ethiopia 2Department of Nutrition and Dietetics, Jimma University, Ethiopia 3Department of Population and Family Health, Jimma University, Ethiopia Abstract Background: Young children are vulnerable to micronutrient (MN) deficiency especially in developing countries. This study aimed to determine the effect of nutrition behavior change intervention on improving micronutrients concentration and linear growth of children age 6 to 59 months in Central Highland of Ethiopia: Design: A cluster-randomized controlled Community Trial was carried out from February 2017 to April 2019 for women who had children age 6 to 59 months. Comparing mean and Generalized Estimating Equa tions (GEE) models were fitted to children’s linear growth and identify predictors of child linear growth Setting: The study was conducted in six districts found in the central highland of Ethiopia. Households (HH) and correspondent mothers/caregivers with their index children were included in the study assigned to the intervention group received monthly nutrition education and counseling. Participants: About 1012 at baseline followed up and end-line data were collected for 815 study subjects. Results: Iodine deference (ID) and Iron deficiency anemia (IDA) lowered to 6.15% and 8.83% respectively at the end of the intervention. The mean end-line-baseline difference (MD) of iodine concentration the differences between intervention and control groups (MD=198.38 μg/L P<0.05) and MD of hemoglobin concentration (Hbc) MD=3.87 g/L, P<0.05.