Gastroenterology
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Real World Efficacy and Tolerability of Acotiamide, in Relieving Meal
testinal & in D o i tr g s e Journal of Gastrointestinal & a s t G i v f e o Narayanan et al., J Gastrointest Dig Syst 2018, 8:1 S l y a s n r ISSN: 2161-069Xt Digestive System DOI: 10.4172/2161-069X.1000553 e u m o J Research Article Open Access Real World Efficacy and Tolerability of Acotiamide, in Relieving Meal- related Symptoms of Functional Dyspepsia Varsha Narayanan*, Amit Bhargava and Shailesh Pallewar 1Department of Medical Services and Research, Lupin Ltd., India *Corresponding author: Narayanan V, Department of Medical Services and Research, Lupin Ltd., Mumbai, India, Tel: +912266402222; E-mail: [email protected] Received date: February 09, 2018; Accepted date: February 21, 2018; Published date: February 27, 2018 Copyright: © 2018 Narayanan V, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited. Abstract Background: Functional Dyspepsia (FD) is a highly prevalent clinical condition that imposes negative economic burden on health-care system as well as greatly impairs quality of life. Treatment of non-specific and bothersome meal-related FD symptoms like post-prandial fullness, upper abdominal bloating and early satiety, is a therapeutic challenge for the clinicians as poorly-defined and ill-understood pathogenesis has hampered efforts to develop effective treatments. Acotiamide is first-in-class drug that exerts its gastro-kinetic effect by enhancing acetylcholine release. Though evidence of its efficacy and tolerance are available through randomized clinical trials, real world data from its regular in-clinic use is lacking. -

Gastrointestinal (GI) Motility, Chronic Therapeutic Class Review
Gastrointestinal (GI) Motility, Chronic Therapeutic Class Review (TCR) March 7, 2019 No part of this publication may be reproduced or transmitted in any form or by any means, electronic or mechanical, including photocopying, recording, digital scanning, or via any information storage or retrieval system without the express written consent of Magellan Rx Management. All requests for permission should be mailed to: Magellan Rx Management Attention: Legal Department 6950 Columbia Gateway Drive Columbia, Maryland 21046 The materials contained herein represent the opinions of the collective authors and editors and should not be construed to be the official representation of any professional organization or group, any state Pharmacy and Therapeutics committee, any state Medicaid Agency, or any other clinical committee. This material is not intended to be relied upon as medical advice for specific medical cases and nothing contained herein should be relied upon by any patient, medical professional or layperson seeking information about a specific course of treatment for a specific medical condition. All readers of this material are responsible for independently obtaining medical advice and guidance from their own physician and/or other medical professional in regard to the best course of treatment for their specific medical condition. This publication, inclusive of all forms contained herein, is intended to be educational in nature and is intended to be used for informational purposes only. Send comments and suggestions to [email protected]. March 2019 Proprietary Information. Restricted Access – Do not disseminate or copy without approval. © 2004–2019 Magellan Rx Management. All Rights Reserved. FDA-APPROVED INDICATIONS Drug Manufacturer Indication(s) alosetron (Lotronex®)1 generic, . -

PN0496-Acotiamide.Pdf
Acotiamide hydrochloride hydrate (Acofide®) 盐酸阿考替胺 Z-338 in Zeria; YM-443 in Astellas Tablet, oral, EQ 100 mg acotiamide Acotiamide is a peripheral acetylcholinesterase inhibitor, indicated for the treatment of functional dyspepsia (FD), which was first-in-class drug to treat FD in the world and approved in 2013 by Japan PMDA. It was originally discovered by Zeria, and co-developed with Astellas. The drug is co-marketing in Japan with a single brand name. The human recommended starting dose is 100 mg at a time, and 3 times a day before meals. Worldwide Key Approvals Global Sales ($Million) Key Substance Patent Expiration 2016-May (US5981557A) 2016-May (EP0870765B1) 2013-Mar (JP) Not available 2021-May (JP3181919B2) 2016-May (CN1063442C) Mechanism of Action Acotiamide hydrochloride hydrate is an acetylcholinesterase (AChE) inhibitor and enhanced the acetylcholine (ACh)-induced contraction and motility of the gastric antrum and the gastric body. Target Binding Selectivity In vitro Efficacy In vivo Efficacy Mixed pattern: Ki1= 0.61 µM Effect dose of contraction in gastric sample: Significantly improved the gastrointestinal motility: Ki2= 2.7 µM ACh-induced: at 1 µM In normal and gastric hypomotility dogs: at 10 mg/kg. Inhibition: IC50= 3 µM Electrical-induced: at 0.3 µM In gastric hypomotility rats: at 100 mg/kg. Pharmacokinetics Parameters Rats Dogs Healthy Humans 3 10 3 10 50 mg 100 mg 200 mg 400 mg 800 mg Dose (mg/kg) (i.v.) (p.o.) (i.v.) (p.o.) (p.o.) (p.o.) (p.o.) (p.o.) (p.o.) Tmax (hr) - 0.08 - 0.5 2.75 2.42 2.08 2.25 2.13 Cmax -

New Developments in Prokinetic Therapy for Gastric Motility Disorders
REVIEW published: 24 August 2021 doi: 10.3389/fphar.2021.711500 New Developments in Prokinetic Therapy for Gastric Motility Disorders Michael Camilleri* and Jessica Atieh Clinical Enteric Neuroscience Translational and Epidemiological Research (CENTER), Division of Gastroenterology and Hepatology, Mayo Clinic, Rochester, MN, United States Prokinetic agents amplify and coordinate the gastrointestinal muscular contractions to facilitate the transit of intra-luminal content. Following the institution of dietary recommendations, prokinetics are the first medications whose goal is to improve gastric emptying and relieve symptoms of gastroparesis. The recommended use of metoclopramide, the only currently approved medication for gastroparesis in the United States, is for a duration of less than 3 months, due to the risk of reversible or irreversible extrapyramidal tremors. Domperidone, a dopamine D2 receptor antagonist, is available for prescription through the FDA’s program for Expanded Access to Investigational Drugs. Macrolides are used off label and are associated with tachyphylaxis and variable duration of efficacy. Aprepitant relieves some symptoms of gastroparesis. There are newer agents in the pipeline targeting diverse gastric (fundic, antral and pyloric) motor functions, including novel serotonergic 5-HT4 agonists, dopaminergic D2/3 antagonists, neurokinin NK1 antagonists, and ghrelin agonist. Novel Edited by: targets with potential to improve gastric motor functions include the pylorus, macrophage/ Jan Tack, inflammatory function, oxidative -

Pharmacological Agents Currently in Clinical Trials for Disorders in Neurogastroenterology
Pharmacological agents currently in clinical trials for disorders in neurogastroenterology Michael Camilleri J Clin Invest. 2013;123(10):4111-4120. https://doi.org/10.1172/JCI70837. Clinical Review Esophageal, gastrointestinal, and colonic diseases resulting from disorders of the motor and sensory functions represent almost half the patients presenting to gastroenterologists. There have been significant advances in understanding the mechanisms of these disorders, through basic and translational research, and in targeting the receptors or mediators involved, through clinical trials involving biomarkers and patient responses. These advances have led to relief of patients’ symptoms and improved quality of life, although there are still significant unmet needs. This article reviews the pipeline of medications in development for esophageal sensorimotor disorders, gastroparesis, chronic diarrhea, chronic constipation (including opioid-induced constipation), and visceral pain. Find the latest version: https://jci.me/70837/pdf Review Pharmacological agents currently in clinical trials for disorders in neurogastroenterology Michael Camilleri Clinical Enteric Neuroscience Translational and Epidemiological Research (CENTER), Mayo Clinic, Rochester, Minnesota, USA. Esophageal, gastrointestinal, and colonic diseases resulting from disorders of the motor and sensory functions represent almost half the patients presenting to gastroenterologists. There have been significant advances in under- standing the mechanisms of these disorders, through basic and translational research, and in targeting the recep- tors or mediators involved, through clinical trials involving biomarkers and patient responses. These advances have led to relief of patients’ symptoms and improved quality of life, although there are still significant unmet needs. This article reviews the pipeline of medications in development for esophageal sensorimotor disorders, gastropa- resis, chronic diarrhea, chronic constipation (including opioid-induced constipation), and visceral pain. -

Classification Decisions Taken by the Harmonized System Committee from the 47Th to 60Th Sessions (2011
CLASSIFICATION DECISIONS TAKEN BY THE HARMONIZED SYSTEM COMMITTEE FROM THE 47TH TO 60TH SESSIONS (2011 - 2018) WORLD CUSTOMS ORGANIZATION Rue du Marché 30 B-1210 Brussels Belgium November 2011 Copyright © 2011 World Customs Organization. All rights reserved. Requests and inquiries concerning translation, reproduction and adaptation rights should be addressed to [email protected]. D/2011/0448/25 The following list contains the classification decisions (other than those subject to a reservation) taken by the Harmonized System Committee ( 47th Session – March 2011) on specific products, together with their related Harmonized System code numbers and, in certain cases, the classification rationale. Advice Parties seeking to import or export merchandise covered by a decision are advised to verify the implementation of the decision by the importing or exporting country, as the case may be. HS codes Classification No Product description Classification considered rationale 1. Preparation, in the form of a powder, consisting of 92 % sugar, 6 % 2106.90 GRIs 1 and 6 black currant powder, anticaking agent, citric acid and black currant flavouring, put up for retail sale in 32-gram sachets, intended to be consumed as a beverage after mixing with hot water. 2. Vanutide cridificar (INN List 100). 3002.20 3. Certain INN products. Chapters 28, 29 (See “INN List 101” at the end of this publication.) and 30 4. Certain INN products. Chapters 13, 29 (See “INN List 102” at the end of this publication.) and 30 5. Certain INN products. Chapters 28, 29, (See “INN List 103” at the end of this publication.) 30, 35 and 39 6. Re-classification of INN products. -

PHARMACEUTICAL APPENDIX to the TARIFF SCHEDULE 2 Table 1
Harmonized Tariff Schedule of the United States (2020) Revision 19 Annotated for Statistical Reporting Purposes PHARMACEUTICAL APPENDIX TO THE HARMONIZED TARIFF SCHEDULE Harmonized Tariff Schedule of the United States (2020) Revision 19 Annotated for Statistical Reporting Purposes PHARMACEUTICAL APPENDIX TO THE TARIFF SCHEDULE 2 Table 1. This table enumerates products described by International Non-proprietary Names INN which shall be entered free of duty under general note 13 to the tariff schedule. The Chemical Abstracts Service CAS registry numbers also set forth in this table are included to assist in the identification of the products concerned. For purposes of the tariff schedule, any references to a product enumerated in this table includes such product by whatever name known. -

( 12 ) United States Patent
US010317418B2 (12 ) United States Patent ( 10 ) Patent No. : US 10 ,317 ,418 B2 Goosens (45 ) Date of Patent: * Jun . 11 , 2019 (54 ) USE OF GHRELIN OR FUNCTIONAL 7 , 479 ,271 B2 1 / 2009 Marquis et al . GHRELIN RECEPTOR AGONISTS TO 7 ,632 , 809 B2 12 / 2009 Chen 7 ,666 , 833 B2 2 /2010 Ghigo et al. PREVENT AND TREAT STRESS -SENSITIVE 7 , 901 ,679 B2 3 / 2011 Marquis et al . PSYCHIATRIC ILLNESS 8 ,013 , 015 B2 9 / 2011 Harran et al . 8 ,293 , 709 B2 10 /2012 Ross et al . (71 ) Applicant: Massachusetts Institute of 9 ,724 , 396 B2 * 8 / 2017 Goosens A61K 38 /27 9 , 821 ,042 B2 * 11 /2017 Goosens .. A61K 39/ 0005 Technology , Cambridge , MA (US ) 10 , 039 ,813 B2 8 / 2018 Goosens 2002/ 0187938 A1 12 / 2002 Deghenghi (72 ) Inventor : Ki Ann Goosens, Cambridge , MA (US ) 2003 / 0032636 Al 2 /2003 Cremers et al. 2004 / 0033948 Al 2 / 2004 Chen ( 73 ) Assignee : Massachusetts Institute of 2005 / 0070712 A1 3 /2005 Kosogof et al. Technology , Cambridge , MA (US ) 2005 / 0148515 Al 7/ 2005 Dong 2005 / 0187237 A1 8 / 2005 Distefano et al. 2005 /0191317 A1 9 / 2005 Bachmann et al. ( * ) Notice : Subject to any disclaimer , the term of this 2005 /0201938 A1 9 /2005 Bryant et al. patent is extended or adjusted under 35 2005 /0257279 AL 11 / 2005 Qian et al. U . S . C . 154 ( b ) by 0 days. 2006 / 0025344 Al 2 /2006 Lange et al. 2006 / 0025566 A 2 /2006 Hoveyda et al. This patent is subject to a terminal dis 2006 / 0293370 AL 12 / 2006 Saunders et al . -
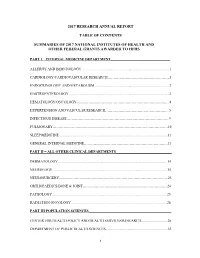
2017 Research Annual Report Table of Contents Summaries of 2017
2017 RESEARCH ANNUAL REPORT TABLE OF CONTENTS SUMMARIES OF 2017 NATIONAL INSTITUTES OF HEALTH AND OTHER FEDERAL GRANTS AWARDED TO HFHS PART I – INTERNAL MEDICINE DEPARTMENT_________________________________ ALLERGY AND IMMUNOLOGY ................................................................................................. 1 CARDIOLOGY/CARDIOVASCULAR RESEARCH…………………………………………….1 ENDOCRINOLOGY AND METABOLISM .................................................................................. 2 GASTROENTEROLOGY ............................................................................................................. .3 HEMATOLOGY/ONCOLOGY…………………………………………………………………...4 HYPERTENSION AND VASCULAR RESEARCH……………………………………………...5 INFECTIOUS DISEASE…………………………………………………………………………..9 PULMONARY……………………………………………………………………………………10 SLEEP MEDICINE ....................................................................................................................... 11 GENERAL INTERNAL MEDICINE…………………………………………………………….13 PART II – ALL OTHER CLINICAL DEPARTMENTS_______________________________ DERMATOLOGY ........................................................................................................................ 14 NEUROLOGY .............................................................................................................................. 15 NEUROSURGERY……………………………………………………………………………….23 ORTHOPAEDICS/BONE & JOINT……………………………………………………………..24 PATHOLOGY .............................................................................................................................. -

COMPARISON of the WHO ATC CLASSIFICATION & Ephmra/Intellus Worldwide ANATOMICAL CLASSIFICATION
COMPARISON OF THE WHO ATC CLASSIFICATION & EphMRA/Intellus Worldwide ANATOMICAL CLASSIFICATION: VERSION June 2019 2 Comparison of the WHO ATC Classification and EphMRA / Intellus Worldwide Anatomical Classification The following booklet is designed to improve the understanding of the two classification systems. The development of the two systems had previously taken place separately. EphMRA and WHO are now working together to ensure that there is a convergence of the 2 systems rather than a divergence. In order to better understand the two classification systems, we should pay attention to the way in which substances/products are classified. WHO mainly classifies substances according to the therapeutic or pharmaceutical aspects and in one class only (particular formulations or strengths can be given separate codes, e.g. clonidine in C02A as antihypertensive agent, N02C as anti-migraine product and S01E as ophthalmic product). EphMRA classifies products, mainly according to their indications and use. Therefore, it is possible to find the same compound in several classes, depending on the product, e.g., NAPROXEN tablets can be classified in M1A (antirheumatic), N2B (analgesic) and G2C if indicated for gynaecological conditions only. The purposes of classification are also different: The main purpose of the WHO classification is for international drug utilisation research and for adverse drug reaction monitoring. This classification is recommended by the WHO for use in international drug utilisation research. The EphMRA/Intellus Worldwide classification has a primary objective to satisfy the marketing needs of the pharmaceutical companies. Therefore, a direct comparison is sometimes difficult due to the different nature and purpose of the two systems. -

Guts and Butts: Treatment Options for IBS and Functional Dyspepsia
7/2/2020 Guts and Butts: Treatment Options for IBS and Functional Dyspepsia Amy McCracken, DNP, APRN 1 Learning Objectives: ● Discuss the diagnosis and management of IBS and functional dyspepsia in order to optimize treatment strategies ● Describe pharmacological and alternative treatment approaches of IBS-C, IBS-D, IBS-M, and functional dyspepsia ● Articulate patient-specific treatment options for those with IBS and functional dyspepsia as derived from case studies 2 1 7/2/2020 Irritable Bowel Syndrome (IBS)-Definition and Epidemiology ● Comprises a group of functional bowel disorders in which abdominal discomfort or pain is associated with defecation or a change in bowel habits in the absence of an organic disease. ● The prevalence of IBS in North America is estimated at approximately 10-15%. ● More common in women compared to men. ● Second highest cause of work absenteeism ● IBS accounts for approximately 25 to 50% of all referrals to gastroenterologists. ● Important to remember: This is a diagnosis of exclusion! 3 IBS-Etiology ● Stress ● Visceral hypersensitivity ● Psychosocial factors ● Common-cannot be explained ● Chronic and benign ● High association with stress in the pathophysiology and clinical presentation of IBS 4 2 7/2/2020 IBS-Signs and Symptoms ● Chronic abdominal pain-usually a cramping sensation that varies in intensity with periodic exacerbations ● The character and location of pain can vary widely and often times related to defecation ● Abdominal fullness, bloating or swelling ● Diarrhea, constipation or alternating -

New Treatment Options for Chronic Constipation: Mechanisms, Efficacy and Safety
View metadata, citation and similar papers at core.ac.uk brought to you by CORE CHRONIC CONSTIPATION – CHALLENGES AND REMEDIES provided by Crossref New treatment options for chronic constipation: Mechanisms, efficacy and safety Michael Camilleri MD M Camilleri. New treatment options for chronic constipation: De nouvelles options thérapeutiques contre la Mechanisms, efficacy and safety. Can J Gastroenterol constipation chronique : leurs mécanismes, leur 2011;(Suppl B):29B-35B. efficacité et leur innocuité The present review has several objectives, the first of which is to review the pharmacology and selectivity of serotonergic agents to La présente analyse comporte plusieurs objectifs, le premier étant de contrast the older serotonergic agents (which were withdrawn because réviser la pharmacologie et la sélectivité des sérotoninergiques pour of cardiac or vascular adverse effects) with the newer generation sero- comparer les anciens sérotoninergiques (retirés du marché en raison de tonin receptor subtype 4 agonists. Second, the chloride ion secret- leurs effets cardiaques ou vasculaires) avec les agonistes de récepteurs agogues that act through the guanylate cyclase C receptor are appraised de la sérotonine de sous-type 4 de nouvelle génération. En deuxième and their pharmacology is compared with the approved medication, lieu, les sécrétagogues des ions chlorures qui agissent par le récepteur lubiprostone. Third, the efficacy and safety of the application of bile du guanylatecyclase C sont évalués, et leur pharmacologie est com- acid modulation to treat constipation are addressed. The long-term parée avec celle du lubiprostone, un médicament approuvé. En studies of surgically induced excess bile acid delivery to the colon are troisième lieu, l’efficacité et l’innocuité de l’application de la modula- reviewed to ascertain the safety of this therapeutic approach.