Clinical Medical Policy
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Optic Disc Drusen in Differential Diagnosis of Optic Neuritis Optik Nörit Ayrıcı Tanısında Optik Disk Druzeni
DO I:10.4274/tnd.56514 Images in Clinical Neurology Optic Disc Drusen in Differential Diagnosis of Optic Neuritis Optik Nörit Ayrıcı Tanısında Optik Disk Druzeni Erkingül Shugaiv1, Elif Aksoy Güzeller2, Sait Alim2 1Tokat State Hospital, Clinic of Neurology, Tokat, Turkey 2Tokat State Hospital, Clinic of Diases Eye, Tokat, Turkey Optic disc drusen is a condition where a hyaline-like calcific object is accumulated on the optical nerve ending, often bilaterally (1). Its prevalence in the general population is 0.34-3.7%. It can be confused with optic papillitis since it blurs the papillary border at the bottom of the eye. Drusens can be seen as opacity in B-scan ultrasonography and computerized tomography (2). Optic disc drusens present with slowly progressing visual field defects. The 21-year-old patient who complained of blurry vision on both eyes did not have a history of disease. Her vision was blurry for the past 10 days, especially on the left side. There was no history of eyeball pain, headache, infection or trauma. Her vision was 0.2 on the right and 0.1 on the left side. The papillary borders were undefined on both sides in the examination of the base of Figure 1. Optic disc drusen on both sides: Discs are protruded due the eyes (Figure 1). Due to the slow clinical decline over 10 days, to the drusen and their borders are not clearly defined. cranial and spinal magnetic resonance imaging was conducted in order to address any possible demyelinating disease but did not produce any remarkable findings. After this, cranial and orbital tomography was conducted with the pre-diagnosis of optic disc drusen. -

Posterior Uveitis Signs
Uveitis unplugged: sorting out infectious uveitis Hobart 2017 Peter McCluskey Save Sight Institute Sydney Eye Hospital Sydney Medical School University of Sydney Sydney Australia No financial or proprietary interest in any material discussed Immunosuppression for IED The fundamental principle for managing uveitis: Is the disease: infective inflammatory neoplastic What is the worst, most acute threat to vision this could be? Immunosuppression for IED The fundamental principle for managing uveitis: Is the disease: infective inflammatory neoplastic What is the worst, most acute threat to vision this could be? usually infection! Common Causes of Uveitis in Sydney 2015 Idiopathic 505 (50%) • idiopathic 424 Infective 203 (20%) • Fuchs 26 • Herpetic 105 • WDS 55 - anterior 83 - posterior 22 Inflammatory 358 (35%) • HLA B27 188 TB 40 (+systemic B27) 46 • • Toxoplasmosis 38 • sarcoid 56 • syphilis 10 (25) • Behcets 18 4 Assessing the patient with uveitis How do I sort this out??? • clinical assessment + carefully selected tests • clinical assessment is the key investigation • critical to take as comprehensive a history and review of systems as possible plus • thorough careful complete examination of each eye Sorting out Uveitis: anterior uveitis signs Anterior Uveitis Signs: • comprehensive a history and systems review • there are some unofficial “rules” can’t diagnose anterior uveitis without a normal fundus on dilated exam • anterior uveitis: mostly non specific signs • KPs, iris and pupil: useful clues Sorting out Uveitis: posterior uveitis -

A Case of Cerebral Granuloma and Optic Papillitis Due to Brucella Sp
Hindawi Case Reports in Infectious Diseases Volume 2020, Article ID 5216249, 3 pages https://doi.org/10.1155/2020/5216249 Case Report A Case of Cerebral Granuloma and Optic Papillitis due to Brucella sp. A. Chiappe-Gonzalez 1,2 and A Solano-Loza2 1Hospital Nacional Dos de Mayo, Lima, Peru 2Cl´ınica Angloamericana, San Isidro, Peru Correspondence should be addressed to A. Chiappe-Gonzalez; [email protected] Received 21 December 2019; Revised 18 April 2020; Accepted 29 June 2020; Published 18 July 2020 Academic Editor: Larry M. Bush Copyright © 2020 A. Chiappe-Gonzalez and A Solano-Loza. ,is is an open access article distributed under the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited. We document a case of a 24-year-old woman who presented with cerebral granuloma and optic papillitis associated to Brucella sp. infection, whose diagnosis was made with a brain biopsy and serology tests, with clinical improvement following specific antibiotic therapy. ,e patient was followed up for over a year without evidence of relapse. 1. Introduction Seven months prior to presentation, she had been eval- uated for this complaint; a head computed tomography (CT) Brucellosis is a common zoonotic infection in many angiography was performed which showed a hypodense, right countries, including Mediterranean and Middle Eastern occipital lesion with ill-defined borders and peripheral con- countries. In Peru, the prevalence of brucellosis has been trast enhancement (Figure 1); the study was followed by a poorly documented, with higher frequency in the cities of brain magnetic resonance imaging (MRI), which confirmed Lima, Callao, and Ica probably due to the informal goat the presence of a solid cortical formation of about 0.7 cen- farming in these regions. -

Myelin Oligodendrocyte Glycoprotein-Igg-Positive Recurrent Bilateral Optic Papillitis with Serous Retinal Detachment: a Case Report
doi: 10.2169/internalmedicine.9840-17 Intern Med Advance Publication http://internmed.jp 【 CASE REPORT 】 Myelin Oligodendrocyte Glycoprotein-IgG-positive Recurrent Bilateral Optic Papillitis with Serous Retinal Detachment: A Case Report Tomoya Kon 1, Hiroki Hikichi 1, Tatsuya Ueno 1, Chieko Suzuki 1, Jinichi Nunomura 1, Kimihiko Kaneko 2, Toshiyuki Takahashi 2,3, Ichiro Nakashima 2 and Masahiko Tomiyama 1 Abstract: Autoantibodies against myelin oligodendrocyte glycoprotein (MOG-IgG) have been detected in inflamma- tory demyelinating central nervous system diseases. A 30-year-old woman had blurred vision, marked optic nerve disc swelling, serous retinal detachment at the macular on optic coherence tomography, and MOG-IgG seropositivity. The patient was thought to have optic papillitis associated with MOG-IgG. Her symptoms rap- idly improved after high-dose methylprednisolone therapy. We hypothesize that serous retinal detachment was secondary, arising from optic papillitis. This is the first report of the concurrence of optic papillitis with MOG-IgG and serous retinal detachment. MOG-IgG should be tested in patients with marked optic disc swelling. Key words: IgA nephropathy, MOG, myelin oligodendrocyte glycoprotein, optic neuritis, optic papillitis, serous retinal detachment (Intern Med Advance Publication) (DOI: 10.2169/internalmedicine.9840-17) inflammatory diseases, such as Vogt-Koyanagi-Harada dis- Introduction ease, sarcoidosis, and Behçet’s disease, disrupt the blood- retinal barrier, resulting in the development of serous retinal Autoantibodies against myelin oligodendrocyte glycopro- detachment (4, 5). However, to our knowledge, serous reti- tein (MOG-IgG) have been detected in patients with central nal detachment in a patient with MOG-IgG-positive optic nervous system demyelinating diseases, including acute dis- neuritis has not been reported to date. -

Ophthalmology Ophthalomolgy
Ophthalmology Ophthalomolgy Description ICD10-CM Documentation Tips Description ICD10-CM Documentation Tips Cataracts Code Tip Glaucoma Code Tip Cortical age-related cataract, right eye H25.011 Right, left, or bilateral; Presenile, Open angle with borderline H40.011 Suspect, Open angle, Primary senile, traumatic, complicated; findings, low risk, right eye angle closure; type; acute vs., specific type (cortical, anterior or chronic; mild, moderate, severe, Cortical age-related cataract, left eye H25.012 Open angle with borderline H40.012 posterior subcapsular polar, etc) indeterminate findings, low risk, left eye Cortical age-related cataract, bilateral eye H25.013 Open angle with borderline H40.013 findings, low risk, bilateral eye Anterior subcapsular polar age-related H25.031 Anatomical narrow angle, right H40.031 cataract,right eye eye Anterior subcapsular polar age-related H25.032 Anatomical narrow angle, right H40.032 cataract, left eye eye Anterior subcapsular polar age-related H25.033 Anatomical narrow angle, H40.033 cataract, bilateral bilateral Age-related nuclear cataract, right eye H25.11 Primary open-angle H40.11x2 glaucoma, moderate stage Age-related nuclear cataract, left eye H25.12 Globe Rupture Code Tip Age-related nuclear cataract, bilateral eye H25.13 Penetrating wound without S05.62xS Contusion vs. laceration; If foreign body of left eyeball, laceration, with or without sequela prolapsed or loss of intraocular tissue; penetrating wound, with or Combined forms of age-related cataract, H25.811 Contusion of eyeball and -
Fluorescein Angiography Reference Number: OC.UM.CP.0028 Coding Implications Last Review Date: 05/2020 Revision Log
Clinical Policy: Fluorescein Angiography Reference Number: OC.UM.CP.0028 Coding Implications Last Review Date: 05/2020 Revision Log See Important Reminder at the end of this policy for important regulatory and legal information. Description Intravenous Fluorescein Angiography (IVFA) or fluorescent angiography is a technique for examining the circulation of the retina and choroid using a fluorescent dye and a specialized camera. It involves injection of sodium fluorescein into the systemic circulation, and then an angiogram is obtained by photographing the fluorescence emitted after illumination of the retina with blue light at a wavelength of 490 nanometers. This policy describes the medical necessity guidelines for fluorescein angiography. Policy/Criteria I. It is the policy of health plans affiliated with Envolve Vision, Inc.® that fluorescein angiography is medically necessary for the following indications: A. Initial evaluation of a patient with abnormal findings of the fundus / retina on ophthalmoscopy exam including one of the following: 1. Choroidal Neovascular Membranes (CNVM) 2. Lesions of the Retinal Pigment Epithelium (RPE) a. Serous Detachment of the RPE b. Tears or rips of the RPE c. Hemorrhagic detachment 3. Fibrovascular Disciform Scar 4. Vitreous Hemorrhage (patient presents with sudden loss of vision) 5. Drusen 6. Diabetic Retinopathy B. Evaluation of patient presenting with symptoms of sudden vision loss (especially central vision), blurred vision, distortion, etc., which may suggest a subretinal neovascularization and abnormal findings of the fundus / retina on ophthalmoscopy exam. C. Evaluation of patients with nonproliferative (background) and proliferative diabetic retinopathy without macular edema. Frequency is determined by disease progression and the treatment performed. Fluorescein angiography may be performed on the treated eye only at 6 weeks post-treatment and as often as every 8-12 weeks to assist in management of the retinopathy. -

Clinical Medical Policy
CLINICAL MEDICAL POLICY Scanning Computerized Ophthalmic Imaging (SCODI) Policy Name: (L34601) Policy Number: MP-078-MC-NC Responsible Department(s): Medical Management Provider Notice Date: 06/10/2019 Issue Date: 07/15/2019 Effective Date: 07/15/2019 Annual Approval Date: 05/15/2020 Revision Date: N/A Products: North Carolina Medicare Assured All participating and nonparticipating hospitals and Application: providers Page Number(s): 1 of 26 DISCLAIMER Gateway Health℠ (Gateway) medical policy is intended to serve only as a general reference resource regarding coverage for the services described. This policy does not constitute medical advice and is not intended to govern or otherwise influence medical decisions. POLICY STATEMENT Gateway Health℠ may provide coverage under the medical-surgical benefits of the Company’s Medicare products for medically necessary scanning computerized ophthalmic imaging. This policy is designed to address medical necessity guidelines that are appropriate for the majority of individuals with a particular disease, illness or condition. Each person’s unique clinical circumstances warrant individual consideration, based upon review of applicable medical records. Policy No. MP-078-MC-NC Page 1 of 26 DEFINITIONS Abstract: Glaucoma is a leading cause of blindness, and a disease for which treatment methods clearly are available and in common use. Glaucoma also is diagnostically challenging. Almost 50% of glaucoma cases remain undetected. Elevated intraocular pressure is a clear risk factor for glaucoma, but over 30% of those suffering from the disease have pressures in the normal range. Further, most patients having abnormally high pressures will never suffer glaucomatous damage to their vision. Scanning computerized ophthalmic diagnostic imaging (SCODI) allows for early detection of glaucomatous damage to the nerve fiber layer or optic nerve of the eye. -

Anterior Uveitis
Clinical Education Session https://ashm.org.au/training/SSHC-sessions/ About These Slide These slides should not be altered, published, posted online, or used in commercial presentations without permission. Please contact ASHM Sexual Health Project Officer Sabdy Ma at [email protected] if you have any enquiries. ASHM SSHC 2019 HIV/Sexual Health Clinical Education Centre Journal Club 6th May 2020 Dr Anna McNulty Pelvic Inflammatory Disease • Very few publications per year • No recent PID trials ( PEACH study late 1990s, POPI 2005-6) • Search of • Lancet ID • Sexual Health •STD •STI • PLOS one •JID • 4 O&G journals Safety and immunogenicity of the chlamydia vaccine candidate CTH522 adjuvanted with CAF01 liposomes or aluminium hydroxide: a first-in-human, randomised, double-blind, placebo-controlled, phase 1 trial: Abraham S et al Lancet ID Oct 2019 Background -No impact from screening and treatment on prevalence - Some evidence for natural immunity lower bacterial loads if previous infection lower concordance in older sex partners young women who cleared infection spontaneously resisted re-infection Method • CTH 522 ( segments of MOMP) vaccine • different adjuvants • followed by intranasal inoculations • 35 women Results and discussion • All well tolerated • All immunogenic ( cell mediated IFN γ responses and Ab titres), one adjuvant better • Mucosal IgA responses thought to be important • Unknown what is marker for protection • Dose optimisation study planned Trends in diagnosis of pelvic inflammatory disease in an Australian sexual -
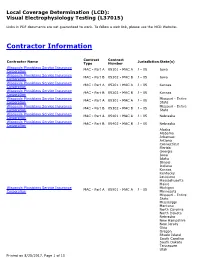
Local Coverage Determination for Visual Electrophysiology Testing
Local Coverage Determination (LCD): Visual Electrophysiology Testing (L37015) Links in PDF documents are not guaranteed to work. To follow a web link, please use the MCD Website. Contractor Information Contract Contract Contractor Name Jurisdiction State(s) Type Number Wisconsin Physicians Service Insurance MAC - Part A 05101 - MAC A J - 05 Iowa Corporation Wisconsin Physicians Service Insurance MAC - Part B 05102 - MAC B J - 05 Iowa Corporation Wisconsin Physicians Service Insurance MAC - Part A 05201 - MAC A J - 05 Kansas Corporation Wisconsin Physicians Service Insurance MAC - Part B 05202 - MAC B J - 05 Kansas Corporation Wisconsin Physicians Service Insurance Missouri - Entire MAC - Part A 05301 - MAC A J - 05 Corporation State Wisconsin Physicians Service Insurance Missouri - Entire MAC - Part B 05302 - MAC B J - 05 Corporation State Wisconsin Physicians Service Insurance MAC - Part A 05401 - MAC A J - 05 Nebraska Corporation Wisconsin Physicians Service Insurance MAC - Part B 05402 - MAC B J - 05 Nebraska Corporation Alaska Alabama Arkansas Arizona Connecticut Florida Georgia Iowa Idaho Illinois Indiana Kansas Kentucky Louisiana Massachusetts Maine Wisconsin Physicians Service Insurance Michigan MAC - Part A 05901 - MAC A J - 05 Corporation Minnesota Missouri - Entire State Mississippi Montana North Carolina North Dakota Nebraska New Hampshire New Jersey Ohio Oregon Rhode Island South Carolina South Dakota Tennessee Utah Printed on 8/25/2017. Page 1 of 15 Contract Contract Contractor Name Jurisdiction State(s) Type Number Virginia -

University of Massachusetts Medical School Eye Care
University of Massachusetts Medical School Eye Care Emergency Department Avoidance (EyEDA) Model: Quantitative Analysis for the PTAC Preliminary Review Team November 1, 2019 Summary This document provides an analysis of Medicare claims data regarding several issues relevant to the proposal submitted by the University of Massachusetts Medical School entitled “Eye Care Emergency Department Avoidance (EyEDA) Model” to the Physician-Focused Payment Model Technical Advisory Committee (PTAC). Those issues include beneficiary use of eye care specialists (optometrists and ophthalmologists), rates of visits (events) for conditions identified by the submitter as being “ED- avoidable” in emergency department (ED) and non-ED locations, and the distribution and rate of events by provider type for the non-ED events. Data used in this analysis are from the 20-percent sample of Medicare Fee-for-Service (FFS) claims maintained in the Centers for Medicare & Medicaid Services (CMS) Chronic Conditions Data Warehouse (CCW). Data were accessed on August 29, 2019, and cover claims with end dates in calendar year (CY) 2017. Appendix A contains definitions of measures used in the analysis. Appendices B and C contain the provider and diagnosis codes used, respectively. Exhibit 1 shows the count of Medicare beneficiaries who saw an ophthalmologist or optometrist on a FFS basis during CY 2017 by selected medical conditions: whether they were ever diagnosed with diabetes, ever diagnosed with glaucoma, or had cataract surgery during the year. These three conditions were selected because Medicare provides expanded coverage of eye care services for beneficiaries with these conditions. Exhibit 2 shows the number of events observed in CY 2017 for eye conditions identified by the submitter. -

Neuro-Ophthalmology ICD-10-CM Quick Reference Guide
American Academy of Ophthalmic Executives® Neuro-Ophthalmology ICD-10-CM Quick Reference Guide Effective Oct. 1, 2020 Disorders of the Nervous System TYPE RT LT BOTH SINGLE CODE UNSPECIFIED Amaurosis fugax X X X G45.3 X Arnold-chiari malformation X X X G93.5 X Benign intracranial hypertension X X X G93.2 X Blepharospasm X X X G24.5 X Clonic hemifacial spasm G51.31 G51.32 G51.33 X G51.39 Horner’s Syndrome X X X G90.2 X Multiple sclerosis X X X G35 X Myasthenia gravis with (acute) exacerbation X X X G70.01 X Myasthenia gravis without (acute) X X X G70.00 X exacerbation Ophthalmoplegic migraine, intractable X X X G43.B1 X Ophthalmoplegic migraine, not intractable X X X G43.B0 X Transient cerebral ischemic attack, X X X G45.9 X unspecified (eg. TIA) Disorders of Optic Nerve & Visual Pathways TYPE RT LT BOTH SINGLE CODE UNSPECIFIED Cortical blindness H47.611 H47.612 X X H47.619 Disorders of optic chiasm X X X H47.49 X Disorders of optic chiasm associated with X X X H47.41 X inflammatory disorders Disorders of optic chiasm associated with X X X H47.42 X other neoplasms Disorders of optic chiasm associated with X X X H47.43 X vascular disorders Drusen of optic nerve H47.321 H47.322 H47.323 X H47.329 Glaucomatous optic atrophy H47.231 H47.232 H47.233 X H47.239 Hereditary optic atrophy X X X H47.22 X Ischemic optic neuropathy H47.011 H47.012 H47.013 X H47.019 Page 1 of 5 © American Academy of Ophthalmology Neuro-Ophthalmology ICD-10-CM Quick Reference Guide Effective Oct. -

Electroretinography Reference Number: CP.VP.86 Coding Implications Last Review Date: 12/2020 Revision Log
Clinical Policy: Electroretinography Reference Number: CP.VP.86 Coding Implications Last Review Date: 12/2020 Revision Log See Important Reminder at the end of this policy for important regulatory and legal information. Description Electroretinography (ERG) measures the electrical activity generated by neural and non-neuronal cells in the retina in response to a light stimulus to detect loss of retinal function or distinguish between retinal and optic nerve lesions. This policy describes the medical necessity requirements for ERG. Policy/Criteria I. It is the policy of health plans affiliated with Centene Corporation® (Centene) that ERG is medically necessary for any of the following indications: A. Toxic retinopathies and maculopathies; B. Diabetic retinopathy; C. Retinal vascular disease; D. Autoimmune retinopathies; E. Retinal detachment; F. Assessment of retinal function after trauma; G. Retinitis pigmentosa and diseases mimicking retinitis pigmentosa; H. Retinitis punctate albescens; I. Leber’s congenital amaurosis; J. Choroideremia; K. Gyrate atrophy of the retinal and choroid; L. Goldman-Favre syndrome; M. Congenital stationary night blindness; N. X-linked juvenile retinoschisis; O. Achromatopsia; P. Cone dystrophy; Q. Usher syndrome. II. It is the policy of health plans affiliated with Centene that ERG is not medically necessary for any of the following indications: A. Management or diagnosis of glaucoma; B. Management or diagnosis of autism. Background Information ERGs are usually obtained using electrodes embedded in a corneal contact lens or a thin wire inside the lower eyelid that measure a summation of retinal electrical activity at the corneal surface. The ERG helps to distinguish retinal degeneration and dystrophies. Multi-focal electroretinography (mfERG) is a higher resolution form of ERG enabling assessment of ERG activity in small areas of the retina.