Acta Nr. 4 2012.Qxd
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

The National Economic Burden of Rare Disease Study February 2021
Acknowledgements This study was sponsored by the EveryLife Foundation for Rare Diseases and made possible through the collaborative efforts of the national rare disease community and key stakeholders. The EveryLife Foundation thanks all those who shared their expertise and insights to provide invaluable input to the study including: the Lewin Group, the EveryLife Community Congress membership, the Technical Advisory Group for this study, leadership from the National Center for Advancing Translational Sciences (NCATS) at the National Institutes of Health (NIH), the Undiagnosed Diseases Network (UDN), the Little Hercules Foundation, the Rare Disease Legislative Advocates (RDLA) Advisory Committee, SmithSolve, and our study funders. Most especially, we thank the members of our rare disease patient and caregiver community who participated in this effort and have helped to transform their lived experience into quantifiable data. LEWIN GROUP PROJECT STAFF Grace Yang, MPA, MA, Vice President Inna Cintina, PhD, Senior Consultant Matt Zhou, BS, Research Consultant Daniel Emont, MPH, Research Consultant Janice Lin, BS, Consultant Samuel Kallman, BA, BS, Research Consultant EVERYLIFE FOUNDATION PROJECT STAFF Annie Kennedy, BS, Chief of Policy and Advocacy Julia Jenkins, BA, Executive Director Jamie Sullivan, MPH, Director of Policy TECHNICAL ADVISORY GROUP Annie Kennedy, BS, Chief of Policy & Advocacy, EveryLife Foundation for Rare Diseases Anne Pariser, MD, Director, Office of Rare Diseases Research, National Center for Advancing Translational Sciences (NCATS), National Institutes of Health Elisabeth M. Oehrlein, PhD, MS, Senior Director, Research and Programs, National Health Council Christina Hartman, Senior Director of Advocacy, The Assistance Fund Kathleen Stratton, National Academies of Science, Engineering and Medicine (NASEM) Steve Silvestri, Director, Government Affairs, Neurocrine Biosciences Inc. -

Klinefelter Syndrome) at 9 Years of Age
17th SSBP International Research Symposium Developmental trajectories of behavioural phenotypes Programme Book 10–13 October 2014 • New York, USA 2 17th International SSBP Research Symposium The Society for the Study 3 of Behavioural Phenotypes 10th – 13th October 2014 The 17th SSBP International Meeting Developmental Trajectories of Behavioural Phenotypes New York, USA 10th – 13th October 2014, New York, USA Contents Contents Welcome ........................................................................................................................................................................................................9 New York Conference Organiser ..............................................................................................................................................10 Scientific Committee ..........................................................................................................................................................................11 4 The SSBP .......................................................................................................................................................................................................12 The SSBP Executive Committee : ...........................................................................................................................................................................12 Meetings of the SSBP ....................................................................................................................................................................................................13 -

Sema4 Noninvasive Prenatal Select
Sema4 Noninvasive Prenatal Select Noninvasive prenatal testing with targeted genome counting 2 Autosomal trisomies 5 Trisomy 21 (Down syndrome) 6 Trisomy 18 (Edwards syndrome) 7 Trisomy 13 (Patau syndrome) 8 Trisomy 16 9 Trisomy 22 9 Trisomy 15 10 Sex chromosome aneuploidies 12 Monosomy X (Turner syndrome) 13 XXX (Trisomy X) 14 XXY (Klinefelter syndrome) 14 XYY 15 Microdeletions 17 22q11.2 deletion 18 1p36 deletion 20 4p16 deletion (Wolf-Hirschhorn syndrome) 20 5p15 deletion (Cri-du-chat syndrome) 22 15q11.2-q13 deletion (Angelman syndrome) 22 15q11.2-q13 deletion (Prader-Willi syndrome) 24 11q23 deletion (Jacobsen Syndrome) 25 8q24 deletion (Langer-Giedion syndrome) 26 Turnaround time 27 Specimen and shipping requirements 27 2 Noninvasive prenatal testing with targeted genome counting Sema4’s Noninvasive Prenatal Testing (NIPT)- Targeted Genome Counting analyzes genetic information of cell-free DNA (cfDNA) through a simple maternal blood draw to determine the risk for common aneuploidies, sex chromosomal abnormalities, and microdeletions, in addition to fetal gender, as early as nine weeks gestation. The test uses paired-end next-generation sequencing technology to provide higher depth across targeted regions. It also uses a laboratory-specific statistical model to help reduce false positive and false negative rates. The test can be offered to all women with singleton, twins and triplet pregnancies, including egg donor. The conditions offered are shown in below tables. For multiple gestation pregnancies, screening of three conditions -

Orphanet Report Series Rare Diseases Collection
Marche des Maladies Rares – Alliance Maladies Rares Orphanet Report Series Rare Diseases collection DecemberOctober 2013 2009 List of rare diseases and synonyms Listed in alphabetical order www.orpha.net 20102206 Rare diseases listed in alphabetical order ORPHA ORPHA ORPHA Disease name Disease name Disease name Number Number Number 289157 1-alpha-hydroxylase deficiency 309127 3-hydroxyacyl-CoA dehydrogenase 228384 5q14.3 microdeletion syndrome deficiency 293948 1p21.3 microdeletion syndrome 314655 5q31.3 microdeletion syndrome 939 3-hydroxyisobutyric aciduria 1606 1p36 deletion syndrome 228415 5q35 microduplication syndrome 2616 3M syndrome 250989 1q21.1 microdeletion syndrome 96125 6p subtelomeric deletion syndrome 2616 3-M syndrome 250994 1q21.1 microduplication syndrome 251046 6p22 microdeletion syndrome 293843 3MC syndrome 250999 1q41q42 microdeletion syndrome 96125 6p25 microdeletion syndrome 6 3-methylcrotonylglycinuria 250999 1q41-q42 microdeletion syndrome 99135 6-phosphogluconate dehydrogenase 67046 3-methylglutaconic aciduria type 1 deficiency 238769 1q44 microdeletion syndrome 111 3-methylglutaconic aciduria type 2 13 6-pyruvoyl-tetrahydropterin synthase 976 2,8 dihydroxyadenine urolithiasis deficiency 67047 3-methylglutaconic aciduria type 3 869 2A syndrome 75857 6q terminal deletion 67048 3-methylglutaconic aciduria type 4 79154 2-aminoadipic 2-oxoadipic aciduria 171829 6q16 deletion syndrome 66634 3-methylglutaconic aciduria type 5 19 2-hydroxyglutaric acidemia 251056 6q25 microdeletion syndrome 352328 3-methylglutaconic -
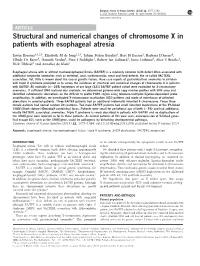
Structural and Numerical Changes of Chromosome X in Patients with Esophageal Atresia
European Journal of Human Genetics (2014) 22, 1077–1084 & 2014 Macmillan Publishers Limited All rights reserved 1018-4813/14 www.nature.com/ejhg ARTICLE Structural and numerical changes of chromosome X in patients with esophageal atresia Erwin Brosens*,1,2,5, Elisabeth M de Jong1,2,5, Tahsin Stefan Barakat3, Bert H Eussen1, Barbara D’haene4, Elfride De Baere4, Hannah Verdin4, Pino J Poddighe1, Robert-Jan Galjaard1, Joost Gribnau3, Alice S Brooks1, Dick Tibboel2 and Annelies de Klein1 Esophageal atresia with or without tracheoesophageal fistula (EA/TEF) is a relatively common birth defect often associated with additional congenital anomalies such as vertebral, anal, cardiovascular, renal and limb defects, the so-called VACTERL association. Yet, little is known about the causal genetic factors. Rare case reports of gastrointestinal anomalies in children with triple X syndrome prompted us to survey the incidence of structural and numerical changes of chromosome X in patients with EA/TEF. All available (n ¼ 269) karyotypes of our large (321) EA/TEF patient cohort were evaluated for X-chromosome anomalies. If sufficient DNA material was available, we determined genome-wide copy number profiles with SNP array and identified subtelomeric aberrations on the difficult to profile PAR1 region using telomere-multiplex ligation-dependent probe amplification. In addition, we investigated X-chromosome inactivation (XCI) patterns and mode of inheritance of detected aberrations in selected patients. Three EA/TEF patients had an additional maternally inherited X chromosome. These three female patients had normal random XCI patterns. Two male EA/TEF patients had small inherited duplications of the XY-linked SHOX (Short stature HOmeoboX-containing) locus. -
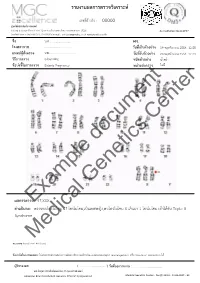
Example Document Medical Genetics Center
รายงานผลการตรวจววเคราะหย เลขทธรออางอนง : 00000 ศผนยยพวนธธศาสตรยการแพทยย 6/6 หมนม 6 ถนนสสขาภนบาล 5 ซอย 32 แขวงออเงนน เขตสายไหม กรสงเทพมหานคร 10220 Accreditation No.4148/57 โทรศกพทย/โทรสาร 086-8861203, 02-7920726 e-mail : [email protected] www.genetics.co.th ชชชอ น.ส............................. HN. ............. โรงพยาบาล .................................... ววนททชเกกบตววอยยาง 19 พฤศจนกายน 2558 12:55 แพทยยผผผสวชงตรวจ นพ.................................... ววนททชรวบตววอยยาง 20 พฤศจนกายน 2558 12:43 ววธทการตรวจ G-banding ชนวดตววอยยาง นนนาครรนา ขผอบยงชทชในการตรวจ Elderly Pregnancy หนยวยสยงตรวจ ไมมมธ Center document Genetics ผลการตรวจExample: 47,XXX คคาอธวบาย : ตรวจพบโครโมโซม 47 โครโมโซม,เปปนเพศหญนง,พบโครโมโซม X เกนนมา 1 โครโมโซม เขอาไดอกกบ Triple X Syndrome Medical หมายเหตธ: Band level 450 band ขผอจคากวดในการทดสอบ: ไมมสามารถตรวจสอบความผนดปกตนขนาดเลลกชนนด submicroscopic rearrangement หรรอ low-level mosaicism ไดอ ผผผรวบรองผล ( .................................. ) ววนททชออกรายงาน : ....................................... นพ.วทรยธทธ ประพวนธยพจนย,พบ.,วว.กธมารเวชศาสตรย American Board of Medical Genetics (Clinical Cytogenetics) Medical Genetics Center : Fo-QP-19/01 : 16-03-2015 : 02 เรียน อ.นพ...................................... ที่นับถือ ตามที่ผลตรวจโครโมโซมจากน ้าคร่้าของ นส........................ (HN .............., Lab no. ..............) พบ โครโมโซม X เกินมา 1 โครโมโซมนั น ความผิดปกติดังกล่าว เข้าได้กับกลุ่มอาการ trisomy X หรือ triple X syndrome ซึ่งเป็นความผิดปกติของโครโมโซมเพศที่พบได้บ่อยในทารกเพศหญิง โดยความผิดปกติของ โครโมโซมแบบนี -
Inside This Issue
Winter 2014 No. 77 Inside this issue Group News | Fundraising | Members’ Letters | One Family Living with Two Different Chromosome Disorders | Bristol Conference 2014 | Unique Leaflets | Christmas Card Order Form Sophie, Unique’s Chair of Trustees Dear Members, In the past month a few things have reminded me of why it is so important to make connections through Unique but also to draw support from other parents around us. I’ve just returned from Unique’s most recent family conference in Bristol where 150 of us parents and carers had a lovely time in workshops, meals and activities, chatting and watching our children milling around together like one big family since – although we had never met before – we have shared so many experiences in common. However in contrast I have also just met a new mum who has just moved to my area from far away with two toddlers, one with a rare joys of the internet, it is becoming easier to meet others with similar, chromosome disorder, who is starting from scratch with no even very rare, chromosome disorders around the world and to find professional, medical or social support. She reminds me of how yourself talking to them in the middle of the night about some lonely I felt when Max was newly diagnosed, when I knew no one interesting things our children share in common (obsession with with a disabled child let alone anyone with a rare chromosome catalogues, anyone?) And of course we also have an enormous disorder. Elsewhere our latest Unique Facebook group, Unique amount in common with so many parents of children with other Russia, is also just starting up – so far it includes just a small special needs or disabilities around us in our own communities who number of members sharing very different experiences to mine here will often be walking the same path as us. -

Prenatal Diagnosis by FISH of a 22Ql 1 Deletion in Two Families J Med Genet: First Published As 10.1136/Jmg.35.2.165 on 1 February 1998
I Med Genet 1998;35:165-168 165 Prenatal diagnosis by FISH of a 22ql 1 deletion in two families J Med Genet: first published as 10.1136/jmg.35.2.165 on 1 February 1998. Downloaded from Marie-France Portnoi, Nicole Joye, Marie Gonzales, Suzanne Demczuk, Laurent Fermont, Gilles Gaillard, Guy Bercau, Genevieve Morlier, Jean-Louis Taillemite Abstract balanced translocation t(I 1;22)(q23;ql 1) was We report on prenatal diagnosis by FISH shown in the father's karyotype; in the second of a sporadic 22qll deletion associated case trisomy X was associated with a 22ql 1 with DiGeorge syndrome (DGS) in two deletion in the fetus. fetuses after an obstetric ultrasonographic examination detected cardiac anomalies, Materials and methods an interrupted aortic arch in case 1 and KARYOTYPING AND FISH tetralogy of Fallot in case 2. The parents Fetal blood samples were obtained for karyo- decided to terminate the pregnancies. At type analysis and FISH. Cells were harvested necropsy, fetal examination showed char- from cultures of phytohaemagglutinin stimu- acteristic facial dysmorphism associated lated lymphocytes and spread onto slides for with congenital malformations, confirm- the production of G banded or R banded chro- ing full DGS in both fetuses. In addition to mosomes. the 22ql 1 deletion, trisomy X was found in FISH of metaphase chromosomes using dig- the second fetus and a reciprocal balanced oxigenin labelled cosmid probes D22S75 translocation t(l 1 ;22) (q23;ql 1) was found (N25, ONCOR) from the DGS chromosome in the clinically normal father of case 1. region was carried out basically according to These findings highlight the importance Pinkel et al.' This probe was premixed with a of performing traditional cytogenetic control cosmid (D22S39) in 22q13.3 facilitat- analysis and FISH in pregnancies with a ing chromosome identification. -

Double Aneuploidy in Down Syndrome
Chapter 6 Double Aneuploidy in Down Syndrome Fatma Soylemez Additional information is available at the end of the chapter http://dx.doi.org/10.5772/60438 Abstract Aneuploidy is the second most important category of chromosome mutations relat‐ ing to abnormal chromosome number. It generally arises by nondisjunction at ei‐ ther the first or second meiotic division. However, the existence of two chromosomal abnormalities involving both autosomal and sex chromosomes in the same individual is relatively a rare phenomenon. The underlying mechanism in‐ volved in the formation of double aneuploidy is not well understood. Parental ori‐ gin is studied only in a small number of cases and both nondisjunctions occurring in a single parent is an extremely rare event. This chapter reviews the characteristics of double aneuploidies in Down syndrome have been discussed in the light of the published reports. Keywords: Double aneuploidy, Down Syndrome, Klinefelter Syndrome, Chromo‐ some abnormalities 1. Introduction With the discovery in 1956 that the correct chromosome number in humans is 46, the new area of clinical cytogenetic began its rapid growth. Several major chromosomal syndromes with altered numbers of chromosomes were reported, such as Down syndrome (trisomy 21), Turner syndrome (45,X) and Klinefelter syndrome (47,XXY). Since then it has been well established that chromosome abnormalities contribute significantly to genetic disease resulting in reproductive loss, infertility, stillbirths, congenital anomalies, abnormal sexual development, mental retardation and pathogenesis of malignancy [1]. Clinical features of patients with common autosomal or sex chromosome aneuploidy is shown in Table 1. © 2015 The Author(s). Licensee InTech. This chapter is distributed under the terms of the Creative Commons Attribution License (http://creativecommons.org/licenses/by/3.0), which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited. -

Female Polysomy-X and Systemic Lupus Erythematosus
Seminars in Arthritis and Rheumatism 43 (2014) 508–512 Contents lists available at ScienceDirect Seminars in Arthritis and Rheumatism journal homepage: www.elsevier.com/locate/semarthrit Female polysomy-X and systemic lupus erythematosus Mordechai Slae, MDa,n, Merav Heshin-Bekenstein, MDb, Ari Simckes, MDb, Gali Heimer, MDb, Dan Engelhard, MDb, Eli M. Eisenstein, MDc a Department of Pediatrics, University of Alberta Hospital, Edmonton, Alberta, Canada b Department of Pediatrics, Hadassah-Hebrew University Hospital at Ein Kerem, Jerusalem, Israel c Department of Pediatrics, Hadassah-Hebrew University Hospital at Mount-Scopus, Jerusalem, Israel article info abstract Objectives: Systemic lupus erythematosus (SLE) occurs more commonly in females than in males. Recent Keywords: evidence suggests that genetic factors transmitted by the X-chromosome may confer increased risk for Gene dosage autoimmune disease in general, and for SLE in particular. It is therefore possible that X-chromosome Lupus genetics polysomy might confer further increased risk for lupus. In addition to describing the clinical and Polysomy-X immunologic features of a young woman with polysomy-X and SLE, we sought to review all other Sex differences published cases associating female or male polysomy-X with SLE or other forms of autoimmunity. SLE Methods: We report a case of a prepubertal girl with polysomy-X and SLE. We performed a systemic X-chromosome literature review for cases of polysomy-X and SLE and summarize previously published cases. In addition, we reviewed reports concerning the possible association between SLE and other connective tissue diseases and male polysomy-X. Results: An 11-year-old girl with tetrasomy-X (48 XXXX karyotype) presented with prolonged fever. -

Curriculum Vitae
CURRICULUM VITAE David Randal Hessl, Ph.D. Department of Psychiatry and Behavioral Sciences and MIND Institute University of California Davis Medical Center 2825 50th Street Sacramento, CA 95817 (916) 703-0249 [email protected] EDUCATION Ph.D. University of Washington. Seattle, WA (1997) Major Area: Child Clinical Psychology Minor Area: Developmental Psychology Advisor: Geraldine Dawson, Ph.D. M.S. University of Washington. Seattle, WA (1995) Major Area: Child Clinical Psychology B.A. University of California, Los Angeles. Los Angeles, CA (1989) Major: Psychology ADDITIONAL TRAINING 1996 – 1997 APA Accredited Internship. Lucile Salter Packard Children’s Hospital at Stanford and The Children’s Health Council Consortium, Stanford and Palo Alto, CA. 1997 - 1998 MacArthur Foundation Post-Doctoral Fellowship. Institute of Human Development, University of California, Berkeley, CA. ACADEMIC POSITIONS 2014 – present Professor of Clinical Psychiatry. Department of Psychiatry and Behavioral Sciences and MIND Institute, University of California Davis School of Medicine, Sacramento, CA. 2008 – 2014 Associate Professor of Clinical Psychiatry. Department of Psychiatry and Behavioral Sciences and MIND Institute, University of California Davis School of Medicine, Sacramento, CA. David R. Hessl, PhD, 2 2006 – 2008 Assistant Professor of Clinical Psychiatry. Department of Psychiatry and Behavioral Sciences and MIND Institute, University of California Davis School of Medicine, Sacramento, CA. 2003 – 2006 Assistant Clinical Professor. Department of Psychiatry and Behavioral Sciences and MIND Institute, University of California Davis School of Medicine, Sacramento, CA. 2002 – 2003 Psychologist II. MIND Institute, University of California Davis School of Medicine, Sacramento, CA. 1998 - 2001 Research and Clinical Psychologist. Behavioral Neurogenetics Research Center, Division of Child Psychiatry, Stanford University School of Medicine, Stanford, CA. -

Genetic Evaluation of Inpatient Neonatal and Infantile Congenital Heart Defects: New Findings and Review of the Literature
G C A T T A C G G C A T genes Article Genetic Evaluation of Inpatient Neonatal and Infantile Congenital Heart Defects: New Findings and Review of the Literature Benjamin M. Helm 1,2,*, Benjamin J. Landis 3 and Stephanie M. Ware 1,3 1 Department of Medical and Molecular Genetics, Indiana University School of Medicine, Indianapolis, IN 46202, USA; [email protected] 2 Department of Epidemiology, Indiana University Fairbanks School of Public Health, Indianapolis, IN 46202, USA 3 Department of Pediatrics, Indiana University School of Medicine, Indianapolis, IN 46202, USA; [email protected] * Correspondence: [email protected]; Tel.: +1-317-944-3966 Abstract: The use of clinical genetics evaluations and testing for infants with congenital heart defects (CHDs) is subject to practice variation. This single-institution cross-sectional study of all inpatient infants with severe CHDs evaluated 440 patients using a cardiovascular genetics service (2014–2019). In total, 376 (85.5%) had chromosome microarray (CMA), of which 55 (14.6%) were diagnostic in syndromic (N = 35) or isolated (N = 20) presentations. Genetic diagnoses were made in all CHD classes. Diagnostic yield was higher in syndromic appearing infants, but geneticists’ dysmorphology exams lacked complete sensitivity and 6.5% of isolated CHD cases had diagnostic CMA. Interestingly, diagnostic results (15.8%) in left ventricular outflow tract obstruction (LVOTO) defects occurred most Citation: Helm, B.M.; Landis, B.J.; often in patients with isolated CHD. Geneticists’ evaluations were particularly important for second- Ware, S.M. Genetic Evaluation of Inpatient Neonatal and Infantile tier molecular testing (10.5% test-specific yield), bringing the overall genetic testing yield to 17%.