Bats in Ecosystems and Their Wide Spectrum of Viral Infectious Threats: SARS-Cov-2 and Other Emerging Viruses
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Pacific Flying Foxes (Mammalia, Chiroptera) : Two New Species of Pteropus from Samoa, Probably Extinct
A tamerican museum Novitates PUBLISHED BY THE AMERICAN MUSEUM OF NATURAL HISTORY CENTRAL PARK WEST AT 79TH STREET, NEW YORK, NY 10024 Number 3646, 37 pp., 14 figures, 5 tables June 25, 2009 Pacific Flying Foxes (Mammalia: Chiroptera): Two New Species of Pteropus from Samoa, Probably Extinct KRISTOFER M. HELGEN,1 LAUREN E. HELGEN,2 AND DON E. WILSON3 ABSTRACT Two new species of flying foxes (genus Pteropus) from the Samoan archipelago are described on the basis of modern museum specimens collected in the mid-19th century. A medium-sized species (P. allenorum, n. sp.) is introduced from the island of Upolu (Independent Samoa), based on a specimen collected in 1856 and deposited in the Academy of Natural Sciences of Philadelphia. It has not been collected again, and we regard it as almost certainly extinct. This species is smaller bodied and has much smaller teeth than both extant congeners recorded in the contemporary fauna of Samoa (Pteropus samoensis and P. tonganus). The closest relative of this new species may be Pteropus fundatus of northern Vanuatu. The disjunct historical distribution of these two small¬ toothed flying foxes (in Vanuatu and Samoa) suggests that similar species may have been more extensively distributed in the remote Pacific in the recent past. Another species, a very large flying fox with large teeth (P. coxi, n. sp.), is described from two skulls collected in Samoa in 1839-1841 during the U.S. Exploring Expedition; it too has not been collected since. This robust species resembles Pteropus samoensis and Pteropus anetianus of Vanuatu in craniodental conformation but is larger than other Polynesian Pteropus, and in some features it is ecomorphologically convergent on the Pacific monkey-faced bats (the pteropodid genera Pteralopex and Mirimiri). -

Checklist of the Mammals of Indonesia
CHECKLIST OF THE MAMMALS OF INDONESIA Scientific, English, Indonesia Name and Distribution Area Table in Indonesia Including CITES, IUCN and Indonesian Category for Conservation i ii CHECKLIST OF THE MAMMALS OF INDONESIA Scientific, English, Indonesia Name and Distribution Area Table in Indonesia Including CITES, IUCN and Indonesian Category for Conservation By Ibnu Maryanto Maharadatunkamsi Anang Setiawan Achmadi Sigit Wiantoro Eko Sulistyadi Masaaki Yoneda Agustinus Suyanto Jito Sugardjito RESEARCH CENTER FOR BIOLOGY INDONESIAN INSTITUTE OF SCIENCES (LIPI) iii © 2019 RESEARCH CENTER FOR BIOLOGY, INDONESIAN INSTITUTE OF SCIENCES (LIPI) Cataloging in Publication Data. CHECKLIST OF THE MAMMALS OF INDONESIA: Scientific, English, Indonesia Name and Distribution Area Table in Indonesia Including CITES, IUCN and Indonesian Category for Conservation/ Ibnu Maryanto, Maharadatunkamsi, Anang Setiawan Achmadi, Sigit Wiantoro, Eko Sulistyadi, Masaaki Yoneda, Agustinus Suyanto, & Jito Sugardjito. ix+ 66 pp; 21 x 29,7 cm ISBN: 978-979-579-108-9 1. Checklist of mammals 2. Indonesia Cover Desain : Eko Harsono Photo : I. Maryanto Third Edition : December 2019 Published by: RESEARCH CENTER FOR BIOLOGY, INDONESIAN INSTITUTE OF SCIENCES (LIPI). Jl Raya Jakarta-Bogor, Km 46, Cibinong, Bogor, Jawa Barat 16911 Telp: 021-87907604/87907636; Fax: 021-87907612 Email: [email protected] . iv PREFACE TO THIRD EDITION This book is a third edition of checklist of the Mammals of Indonesia. The new edition provides remarkable information in several ways compare to the first and second editions, the remarks column contain the abbreviation of the specific island distributions, synonym and specific location. Thus, in this edition we are also corrected the distribution of some species including some new additional species in accordance with the discovery of new species in Indonesia. -

Lancaster County, PA Archives
Fictitious Names in Business Index 1917-1983 Derived from original indexes within the Lancaster County Archives collection 1001 Hobbies & Crafts, Inc. Corp 1 656 1059 Columbia Avenue Associates 15 420 120 Antiquities 8 47 121 Studio Gallery 16 261 1226 Gallery Gifts 16 278 1722 Motor Lodge Corp 1 648 1810 Associates 15 444 20th Century Card Co 4 138 20thLancaster Century Housing County,6 PA332 Archives 20th Century Television Service 9 180 222 Service Center 14 130 25th Hour 14 43 28th Division Highway Motor Court 9 225 3rd Regular Infantry Corp 1 568 4 R's Associates 16 227 4 Star Linen Supply 12 321 501 Diner 11 611 57 South George Street Associates 16 302 611 Shop & Gallery 16 192 7 Cousins Park City Corp 1 335 78-80 West Main, Inc. Corp 1 605 840 Realty 16 414 A & A Aluminum 15 211 A & A Credit Exchange 4 449 A & B Associates 13 342 A & B Automotive Warehouse Company Corp 1 486 A & B Electronic Products Leasing 15 169 A & B Manufacturing Company 12 162 A & E Advertising 15 54 A & H Collectors Center 12 557 A & H Disposal 15 56 A & H Drywall Finishers 12 588 A & L Marketing 15 426 A & L Trucking 16 358 A & M Enterprises 15 148 A & M New Car Brokers 15 128 A & M Rentals 12 104 A & P Roofing Company 14 211 A & R Flooring Service 15 216 A & R Nissley, Inc. Corp 1 512 A & R Nissley, Inc. Corp 1 720 A & R Nissley, Inc. Corp 2 95 A & R Tour Services Co. -

The Australasian Bat Society Newsletter, Number 31, Nov 2008
The Australasian Bat Society Newsletter, Number 31, Nov 2008 The Australasian Bat Society Newsletter Number 39 November 2012 ABS Website: http://abs.ausbats.org.au ABS Discussion list - email: [email protected] ISSN 1448-5877 © Copyright The Australasian Bat Society, Inc. (2012) The Australasian Bat Society Newsletter, Number 31, Nov 2008 The Australasian Bat Society Newsletter, Number 39, November 2012 – Instructions for Contributors – The Australasian Bat Society Newsletter will accept contributions under one of the following two sections: Research Papers, and all other articles or notes. There are two deadlines each year: 10th March for the April issue, and 10th October for the November issue. The Editor reserves the right to hold over contributions for subsequent issues of the Newsletter, and meeting the deadline is not a guarantee of immediate publication. Opinions expressed in contributions to the Newsletter are the responsibility of the author, and do not necessarily reflect the views of the Australasian Bat Society, its Executive or members. For consistency, the following guidelines should be followed: Emailed electronic copy of manuscripts or articles, sent as an attachment, is the preferred method of submission. Faxed and hard copy manuscripts will be accepted but reluctantly! Please send all submissions to the Newsletter Editor at the email or postal address below. Electronic copy should be in 11 point Arial font, left and right justified with 16 mm left and right margins. Please use Microsoft Word; any version is acceptable. Manuscripts should be submitted in clear, concise English and free from typographical and spelling errors. Please leave two spaces after each sentence. -

Tdn Europe • Page 2 of 8 • Thetdn.Com Saturday • 17 April 2021
SATURDAY, 17 APRIL 2021 GREENLANDS GOAL FOR GLEN SHIEL MENUISIER FOCUSED Glen Shiel (GB) (Pivotal {GB}), who claimed a first Group 1 win ON ARC WITH at age six last season when upsetting the G1 British Champions Sprint S. at 16-1, could make his seasonal debut in the G3 WONDERFUL TONIGHT Greenlands S. at The Curragh on May 22. The Archie Watson- trained gelding also has an option in the G2 Duke Of York S. at York on May 12. Cosmo Charlton, Head Racing Manager for owner Hambleton Racing, said, AGlen Shiel is in fantastic form. Everyone is very happy with him. He=s stepped up into faster work now, and Archie is really pleased. AWe=re weighing up possible starting point options, but it might be the Greenlands S. over in Ireland, a Group 2 at the end of May. The Duke of York is still under consideration as well, but I think the likelihood is he=ll go to the Greenlands and then on to Royal Ascot for the [G1] Diamond Jubilee.@ Cont. p2 Wonderful Tonight | Scoop Dyga IN TDN AMERICA TODAY ALL IN THE FAMILY WITH STONESTREET’S OAKS FILLIES Three of the leading contender’s for the GI Kentucky Oaks were Christopher Wright=s dual Group 1-winning mare Wonderful born and raised at Stonestreet Farm. Click or tap here to go Tonight (Fr) (Le Havre {Ire}) is likely to have a later start to her straight to TDN America. 4-year-old campaign, with all roads leading to the G1 Prix de l=Arc de Triomphe, according to trainer David Menuisier. -

Species-Edition-Melanesian-Geo.Pdf
Nature Melanesian www.melanesiangeo.com Geo Tranquility 6 14 18 24 34 66 72 74 82 6 Herping the final frontier 42 Seahabitats and dugongs in the Lau Lagoon 10 Community-based response to protecting biodiversity in East 46 Herping the sunset islands Kwaio, Solomon Islands 50 Freshwater secrets Ocean 14 Leatherback turtle community monitoring 54 Freshwater hidden treasures 18 Monkey-faced bats and flying foxes 58 Choiseul Island: A biogeographic in the Western Solomon Islands stepping-stone for reptiles and amphibians of the Solomon Islands 22 The diversity and resilience of flying foxes to logging 64 Conservation Development 24 Feasibility studies for conserving 66 Chasing clouds Santa Cruz Ground-dove 72 Tetepare’s turtle rodeo and their 26 Network Building: Building a conservation effort network to meet local and national development aspirations in 74 Secrets of Tetepare Culture Western Province 76 Understanding plant & kastom 28 Local rangers undergo legal knowledge on Tetepare training 78 Grassroots approach to Marine 30 Propagation techniques for Tubi Management 34 Phantoms of the forest 82 Conservation in Solomon Islands: acts without actions 38 Choiseul Island: Protecting Mt Cover page The newly discovered Vangunu Maetambe to Kolombangara River Island endemic rat, Uromys vika. Image watershed credit: Velizar Simeonovski, Field Museum. wildernesssolomons.com WWW.MELANESIANGEO.COM | 3 Melanesian EDITORS NOTE Geo PRODUCTION TEAM Government Of Founder/Editor: Patrick Pikacha of the priority species listed in the Critical Ecosystem [email protected] Solomon Islands Hails Partnership Fund’s investment strategy for the East Assistant editor: Tamara Osborne Melanesian Islands. [email protected] Barana Community The Critical Ecosystem Partnership Fund (CEPF) Contributing editor: David Boseto [email protected] is designed to safeguard Earth’s most biologically rich Prepress layout: Patrick Pikacha Nature Park Initiative and threatened regions, known as biodiversity hotspots. -
Status and Red List of Pakistan's Mammals
SSttaattuuss aanndd RReedd LLiisstt ooff PPaakkiissttaann’’ss MMaammmmaallss based on the Pakistan Mammal Conservation Assessment & Management Plan Workshop 18-22 August 2003 Authors, Participants of the C.A.M.P. Workshop Edited and Compiled by, Kashif M. Sheikh PhD and Sanjay Molur 1 Published by: IUCN- Pakistan Copyright: © IUCN Pakistan’s Biodiversity Programme This publication can be reproduced for educational and non-commercial purposes without prior permission from the copyright holder, provided the source is fully acknowledged. Reproduction of this publication for resale or other commercial purposes is prohibited without prior permission (in writing) of the copyright holder. Citation: Sheikh, K. M. & Molur, S. 2004. (Eds.) Status and Red List of Pakistan’s Mammals. Based on the Conservation Assessment and Management Plan. 312pp. IUCN Pakistan Photo Credits: Z.B. Mirza, Kashif M. Sheikh, Arnab Roy, IUCN-MACP, WWF-Pakistan and www.wildlife.com Illustrations: Arnab Roy Official Correspondence Address: Biodiversity Programme IUCN- The World Conservation Union Pakistan 38, Street 86, G-6⁄3, Islamabad Pakistan Tel: 0092-51-2270686 Fax: 0092-51-2270688 Email: [email protected] URL: www.biodiversity.iucnp.org or http://202.38.53.58/biodiversity/redlist/mammals/index.htm 2 Status and Red List of Pakistan Mammals CONTENTS Contributors 05 Host, Organizers, Collaborators and Sponsors 06 List of Pakistan Mammals CAMP Participants 07 List of Contributors (with inputs on Biological Information Sheets only) 09 Participating Institutions -

The Horse-Breeder's Guide and Hand Book
LIBRAKT UNIVERSITY^' PENNSYLVANIA FAIRMAN ROGERS COLLECTION ON HORSEMANSHIP (fop^ U Digitized by the Internet Archive in 2009 with funding from Lyrasis IVIembers and Sloan Foundation http://www.archive.org/details/horsebreedersguiOObruc TSIE HORSE-BREEDER'S GUIDE HAND BOOK. EMBRACING ONE HUNDRED TABULATED PEDIGREES OF THE PRIN- CIPAL SIRES, WITH FULL PERFORMANCES OF EACH AND BEST OF THEIR GET, COVERING THE SEASON OF 1883, WITH A FEW OF THE DISTINGUISHED DEAD ONES. By S. D. BRUCE, A.i3.th.or of tlie Ainerican. Stud Boole. PUBLISHED AT Office op TURF, FIELD AND FARM, o9 & 41 Park Row. 1883. NEW BOLTON CSNT&R Co 2, Entered, according to Act of Congress, in the year 1883, By S. D. Bruce, In the Office of the Librarian of Congress, at Washington, D. C. INDEX c^ Stallions Covering in 1SS3, ^.^ WHOSE PEDIGREES AND PERFORMANCES, &c., ARE GIVEN IN THIS WORK, ALPHABETICALLY ARRANGED, PAGES 1 TO 181, INCLUSIVE. PART SECOISTD. DEAD SIRES WHOSE PEDIGREES AND PERFORMANCES, &c., ARE GIVEN IN THIS WORK, PAGES 184 TO 205, INCLUSIVE, ALPHA- BETICALLY ARRANGED. Index to Sires of Stallions described and tabulated in tliis volume. PAGE. Abd-el-Kader Sire of Algerine 5 Adventurer Blythwood 23 Alarm Himvar 75 Artillery Kyrle Daly 97 Australian Baden Baden 11 Fellowcraft 47 Han-v O'Fallon 71 Spendthrift 147 Springbok 149 Wilful 177 Wildidle 179 Beadsman Saxon 143 Bel Demonio. Fechter 45 Billet Elias Lawrence ' 37 Volturno 171 Blair Athol. Glen Athol 53 Highlander 73 Stonehege 151 Bonnie Scotland Bramble 25 Luke Blackburn 109 Plenipo 129 Boston Lexington 199 Breadalbane. Ill-Used 85 Citadel Gleuelg... -

Chapter 3 Figure 7
Cover Page The handle http://hdl.handle.net/1887/138409 holds various files of this Leiden University dissertation. Author: Darmanto Title: Good to produce, good to share: Food, hunger, and social values in a contemporary Mentawaian community, Indonesia Issue date: 2020-11-26 3 Plenty of Kat, Lack of Iba: The Availability of and Access to Edible Resources This chapter will describe and present a variety of ecological and quantitative data to demonstrate the availability and the access to food resources around the settlement. This chapter starts with the emic category of ecosystem. Understanding how people use the natural environment and create specific zones will enable us to examine the complex relations between Muntei residents and the environment, the pattern of resources’ exploitation, and in particular, food availability and the access to food resources. The following sections will describe the availability of and the access to a wide range of food resources from plants and animals as well as imported food. 3.1 Manipulated Ecosystem and Productive Zones People see the environment around their settlement as a vast resource containing edible and non-edible animals and plants, which can be exploited. They have established a tenure arrangement in which empty territory and unclaimed objects on it did not exist. All the land, rivers, caves, waterfalls, small lakes, mangroves, and other specific ecosystems have been occupied, named, claimed, and exploited. Each ecosystem and the resources on it are far from uniform, for reasons of their physical and natural character. The variations within those ecosystems are quite considerable, determining the ways people make use of them and the breadth of choice available in the selection of edible resources. -
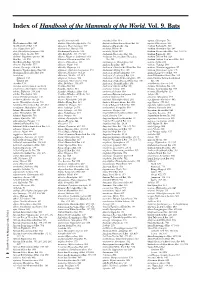
Index of Handbook of the Mammals of the World. Vol. 9. Bats
Index of Handbook of the Mammals of the World. Vol. 9. Bats A agnella, Kerivoula 901 Anchieta’s Bat 814 aquilus, Glischropus 763 Aba Leaf-nosed Bat 247 aladdin, Pipistrellus pipistrellus 771 Anchieta’s Broad-faced Fruit Bat 94 aquilus, Platyrrhinus 567 Aba Roundleaf Bat 247 alascensis, Myotis lucifugus 927 Anchieta’s Pipistrelle 814 Arabian Barbastelle 861 abae, Hipposideros 247 alaschanicus, Hypsugo 810 anchietae, Plerotes 94 Arabian Horseshoe Bat 296 abae, Rhinolophus fumigatus 290 Alashanian Pipistrelle 810 ancricola, Myotis 957 Arabian Mouse-tailed Bat 164, 170, 176 abbotti, Myotis hasseltii 970 alba, Ectophylla 466, 480, 569 Andaman Horseshoe Bat 314 Arabian Pipistrelle 810 abditum, Megaderma spasma 191 albatus, Myopterus daubentonii 663 Andaman Intermediate Horseshoe Arabian Trident Bat 229 Abo Bat 725, 832 Alberico’s Broad-nosed Bat 565 Bat 321 Arabian Trident Leaf-nosed Bat 229 Abo Butterfly Bat 725, 832 albericoi, Platyrrhinus 565 andamanensis, Rhinolophus 321 arabica, Asellia 229 abramus, Pipistrellus 777 albescens, Myotis 940 Andean Fruit Bat 547 arabicus, Hypsugo 810 abrasus, Cynomops 604, 640 albicollis, Megaerops 64 Andersen’s Bare-backed Fruit Bat 109 arabicus, Rousettus aegyptiacus 87 Abruzzi’s Wrinkle-lipped Bat 645 albipinnis, Taphozous longimanus 353 Andersen’s Flying Fox 158 arabium, Rhinopoma cystops 176 Abyssinian Horseshoe Bat 290 albiventer, Nyctimene 36, 118 Andersen’s Fruit-eating Bat 578 Arafura Large-footed Bat 969 Acerodon albiventris, Noctilio 405, 411 Andersen’s Leaf-nosed Bat 254 Arata Yellow-shouldered Bat 543 Sulawesi 134 albofuscus, Scotoecus 762 Andersen’s Little Fruit-eating Bat 578 Arata-Thomas Yellow-shouldered Talaud 134 alboguttata, Glauconycteris 833 Andersen’s Naked-backed Fruit Bat 109 Bat 543 Acerodon 134 albus, Diclidurus 339, 367 Andersen’s Roundleaf Bat 254 aratathomasi, Sturnira 543 Acerodon mackloti (see A. -
A Re-Evaluation of Allometric Relationships for Circulating Concentrations of Glucose in Mammals
Food and Nutrition Sciences, 2016, 7, 240-251 Published Online April 2016 in SciRes. http://www.scirp.org/journal/fns http://dx.doi.org/10.4236/fns.2016.74026 A Re-Evaluation of Allometric Relationships for Circulating Concentrations of Glucose in Mammals Colin G. Scanes Department of Biological Science, University of Wisconsin Milwaukee, Milwaukee, WI, USA Received 10 August 2015; accepted 19 April 2016; published 22 April 2016 Copyright © 2016 by author and Scientific Research Publishing Inc. This work is licensed under the Creative Commons Attribution International License (CC BY). http://creativecommons.org/licenses/by/4.0/ Abstract Purpose: The present study examined the putative relationship between circulating concentra- tions of glucose and log10 body weight in a large sample size (270) of wild species but with domes- ticated animals excluded from the analyses. Methods: A data-set of plasma/serum concentration of glucose and body weight in mammalian species was developed from the literature. Allometric re- lationships were examined. Results: In contrast to previous reports, no overall relationship for circulating concentrations of glucose was observed across 270 species of mammals (for log10 glu- cose concentration adjusted R2 = −0.003; for glucose concentration adjusted R2 = −0.003). In con- trast, a strong allometric relationship was observed for circulating concentrations of glucose in 2 Primates (for log10 glucose concentration adjusted R = 0.511; for glucose concentration adjusted R2 = 0.480). Conclusion: The absence of an allometric relationship for circulating concentrations of glucose was unexpected. A strong allometric relationship was seen in Primates. Keywords Glucose, Allometric, Mammals, Primates 1. Introduction Glucose in the blood is the principal energy source for brain functioning and but glucose can be used as the energy source for multiple other tissues. -

Case 3:13-Cv-00739-AVC Document 61 Filed 08/23/13 Page 1 of 42
Case 3:13-cv-00739-AVC Document 61 Filed 08/23/13 Page 1 of 42 IN THE UNITED STATES DISTRICT COURT FOR THE DISTRICT OF CONNECTICUT JUNE SHEW, et al., : : : Plaintiffs, : Case No. 3:13-cv-00739-AVC v. : : DANNEL P. MALLOY, et al., : : Defendants. : August 23, 2013 PLAINTIFFS’ LOCAL RULE 56(a)1 STATEMENT Plaintiffs, by and through counsel and pursuant to D.Conn.L.Civ.R. 56(a)1, hereby submit this Statement of Undisputed Material Facts in support of their Motion for Summary Judgment dated August 23, 2013 (Doc. # 60) seeking declaratory judgment that Connecticut’s Act Concerning Gun Violence Prevention and Children’s Safety (“the Act”) is unconstitutional, and also an immediate and permanent injunction against the Act’s enforcement. Gun Deaths In The United States 1. The leading cause of death by firearm in the U.S. is suicide. See Pew Research Center, Gun Homicide Rate Down 49% Since 1993 Peak; Public Unaware (May 2013) (“Pew Report”), at 2. [A copy of the Pew Report is attached hereto as “Exhibit A ”]. 2. Gun suicides now account for six out of every ten firearm deaths in this country. Id. 3. The gun suicide rate has been higher than the gun homicide rate since at least 1981. Id. at 4. 4. There were 31,672 firearm deaths in the U.S. in 2010; 61% of these were caused by suicide, versus 35% being caused by homicide. Pew Report at 4. In 2010, firearm suicide was the 1 GOLDBERG SEGALLA, LLP 100 Pearl Street – Suite 1100 Hartford, CT 06103 (860) 760-3300 Case 3:13-cv-00739-AVC Document 61 Filed 08/23/13 Page 2 of 42 fourth leading cause of violent-injury death in the U.S., behind motor vehicle accidents, unintentional poisoning, and falls.