Arthus Reaction As an Adverse Event Following Tdap Vaccination
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Differentiating Between Anxiety, Syncope & Anaphylaxis
Differentiating between anxiety, syncope & anaphylaxis Dr. Réka Gustafson Medical Health Officer Vancouver Coastal Health Introduction Anaphylaxis is a rare but much feared side-effect of vaccination. Most vaccine providers will never see a case of true anaphylaxis due to vaccination, but need to be prepared to diagnose and respond to this medical emergency. Since anaphylaxis is so rare, most of us rely on guidelines to assist us in assessment and response. Due to the highly variable presentation, and absence of clinical trials, guidelines are by necessity often vague and very conservative. Guidelines are no substitute for good clinical judgment. Anaphylaxis Guidelines • “Anaphylaxis is a potentially life-threatening IgE mediated allergic reaction” – How many people die or have died from anaphylaxis after immunization? Can we predict who is likely to die from anaphylaxis? • “Anaphylaxis is one of the rarer events reported in the post-marketing surveillance” – How rare? Will I or my colleagues ever see a case? • “Changes develop over several minutes” – What is “several”? 1, 2, 10, 20 minutes? • “Even when there are mild symptoms initially, there is a potential for progression to a severe and even irreversible outcome” – Do I park my clinical judgment at the door? What do I look for in my clinical assessment? • “Fatalities during anaphylaxis usually result from delayed administration of epinephrine and from severe cardiac and respiratory complications. “ – What is delayed? How much time do I have? What is anaphylaxis? •an acute, potentially -

Early-Phase GVHD Gene Expression Profile in Target Versus Non
Bone Marrow Transplantation (2013) 48, 284–293 & 2013 Macmillan Publishers Limited All rights reserved 0268-3369/13 www.nature.com/bmt ORIGINAL ARTICLE Early-phase GVHD gene expression profile in target versus non-target tissues: kidney, a possible target? B Sadeghi1, H Al-Chaqmaqchi1, S Al-Hashmi1, D Brodin2, Z Hassan1,3, M Abedi-Valugerdi4, A Moshfegh5 and M Hassan1,3 GVHD is a major complication after allo-SCT. In GVHD, some tissues like liver, intestine and skin are infiltrated by donor T cells while others like muscle are not. The mechanism underlying targeted tropism of donor T cells is not fully understood. In the present study, we aim to explore differences in gene expression profile among target versus non-target tissues in a mouse model of GVHD based on chemotherapy conditioning. Expression levels of JAK–signal transducers and activators of transcription (STAT), CXCL1, ICAM1 and STAT3 were increased in the liver and remained unchanged (or decreased) in the muscle and kidney after conditioning. At the start of GVHD the expression levels of CXCL9, ITGb2, SAA3, MARCO, TLR and VCAM1 were significantly higher in the liver or kidney compared with the muscle of GVHD animals. Moreover, biological processes of inflammatory reactions, leukocyte migration, response to bacterium and chemotaxis followed the same pattern. Our data show that both chemotherapy and allogenicity exclusively induce expression of inflammatory genes in target tissues. Moreover, gene expression profile and histopathological findings in the kidney are similar to those observed in the liver of GVHD mice. Bone Marrow Transplantation (2013) 48, 284–293; doi:10.1038/bmt.2012.120; published online 23 July 2012 Keywords: gene expression; GVHD; kidney; target tissues; mouse model INTRODUCTION none of these reports describe any changes in gene expression Allo-SCT is the treatment of choice for a variety of malignant and profile of non-target tissues like muscle. -

Allergic Reactions After Vaccination: Translating Guidelines Into Clinical Practice
R E V I E W EUR ANN ALLERGY CLIN IMMUNOL VOL 51, N 2, 51-61, 2019 A. RADICE1, G. CARLI2, D. MACCHIA1, A. FARSI2 Allergic reactions after vaccination: translating guidelines into clinical practice 1SOS Allergologia e Immunologia, Firenze, Azienda USL Toscana Centro, Italy 2SOS Allergologia e Immunologia, Prato, Azienda USL Toscana Centro, Italy KEYWORDS Summary vaccine; vaccination; allergic reactions; Vaccination represents one of the most powerful medical interventions on global health. anaphylaxis; vaccine hesitancy; vaccine Despite being safe, sustainable, and effective against infectious and in some cases also components; desensitization non-infectious diseases, it’s nowadays facing general opinion’s hesitancy because of a false perceived risk of adverse events. Adverse reactions to vaccines are relatively rare, instead, and those recognizing a hypersensitivity mechanism are even rarer. Corresponding author The purpose of this review is to offer a practical approach to adverse events after vaccina- Anna Radice Ospedale San Giovanni di Dio tion, focusing on immune-mediated reactions with particular regard to their recognition, Via Torregalli 3, 50143 Firenze diagnosis and management. Phone: +39 055 6932304 According to clinical features, we propose an algorythm for allergologic work-up, which E-mail: [email protected] helps in confirming hypersensitivity to vaccine, nonetheless ensuring access to vaccination. Finally, a screening questionnaire is included, providing criteria for immunisation in spe- Doi cialized care settings. 10.23822/EurAnnACI.1764-1489.86 Introduction The gain from vaccination is not just about human health, but it is also a matter of financial resources for health systems. “Smallpox is dead” stated the magazine of the World Health It has been calculated that for every dollar spent in vaccines, Organisation (WHO) in 1980. -
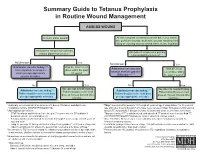
Summary Guide to Tetanus Prophylaxis in Routine Wound Management
Summary Guide to Tetanus Prophylaxis in Routine Wound Management ASSESS WOUND A clean, minor wound All other wounds (contaminated with dirt, feces, saliva, soil; puncture wounds; avulsions; wounds resulting from flying or crushing objects, animal bites, burns, frostbite) Has patient completed a primary Has patient completed a primary tetanus diphtheria series?1, 7 tetanus diphtheria series?1, 7 No/Unknown Yes No/Unknown Yes Administer vaccine today.2,3,4 Was the most recent Administer vaccine and Was the most Instruct patient to complete dose within the past tetanus immune gobulin recent dose within series per age-appropriate 10 years? (TIG) now.2,4,5,6,7 the past 5 years?7 vaccine schedule. No Yes No Yes Vaccine not needed today. Vaccine not needed today. Administer vaccine today.2,4 2,4 Patient should receive next Administer vaccine today. Patient should receive next Patient should receive next dose Patient should receive next dose dose at 10-year interval after dose at 10-year interval after per age-appropriate schedule. per age-appropriate schedule. last dose. last dose. 1 A primary series consists of a minimum of 3 doses of tetanus- and diphtheria- 4 Tdap* is preferred for persons 11 through 64 years of age if using Adacel* or 10 years of containing vaccine (DTaP/DTP/Tdap/DT/Td). age and older if using Boostrix* who have never received Tdap. Td is preferred to tetanus 2 Age-appropriate vaccine: toxoid (TT) for persons 7 through 9 years, 65 years and older, or who have received a • DTaP for infants and children 6 weeks up to 7 years of age (or DT pediatric if Tdap previously. -

Vaccines 101 the Very Last Day That I Was a Pediatric Resident. Um, Many
Vaccines 101 The very last day that I was a pediatric resident. Um, many years ago, a toddler walked into the emergency room and uh, and progressively got sicker and sicker. That's Dr. Katherine Edwards, a world expert in pediatric infectious disease in vaccinology. She's also a professor of pediatrics at Vanderbilt university and she's been working on vaccines for 40 years. I did a spinal tap on her and realized that she had Haemophilus influenza, typ e B meningitis, Haemophilus influenza, type B or HIB is it bacteria normally found in our nose and throat that can lead to very serious life threatening infections and no matter what I did in that day and into the night in terms of prompt antibiotics and she'd just been sick a few hours and, and fluids and all the, you know, ventilators and all the best things that modern medicine, she died, the vaccine for hip was not available until the 1990s. And until it did become available, hip disease affected approximately 25,000 children each year with things like meningitis, pneumonia, and bloodstream infections. And at that time in the hospital that I was practicing at any one time, there were generally five or six patients that had Haemophilus meningitis or invasive disease or some complication of this particular infection. And we knew that from the basic science that if you had antibody to the capsule or to the coat of the organism, that you were protected from disease. But we really didn't know how to make little kids make antibody. -
Difference Between Hypersensitivity and Autoimmunity Key Difference – Hypersensitivity Vs Autoimmunity
Difference Between Hypersensitivity and Autoimmunity www.differencebetwee.com Key Difference – Hypersensitivity vs Autoimmunity Autoimmunity is an adaptive immune response mounted against self-antigens. In simple terms, when your body is acting against its own cells and tissues, this is called an autoimmune reaction. An exaggerated and inappropriate immune response to an antigenic stimulus is defined as a hypersensitivity reaction. Unlike autoimmune reactions that are triggered only by the endogenous antigens, hypersensitivity reactions are triggered by both endogenous and exogenous antigens. This is the key difference between hypersensitivity and autoimmunity. What is Hypersensitivity? An exaggerated and inappropriate immune response to an antigenic stimulus is defined as a hypersensitivity reaction. The first exposure to a particular antigen activates the immune system and, antibodies are produced as a result. This is called sensitization. Subsequent exposures to the same antigen give rise to hypersensitivity. Few important facts regarding the hypersensitivity reactions are given below They can be elicited by both exogenous and endogenous agents. They are a result of an imbalance between the effector mechanisms and the countermeasures that are there to control any inappropriate execution of an immune response. The presence of a genetic susceptibility increases the likelihood of hypersensitivity reactions. The manner in which hypersensitivity reactions harm our body is similar to the way that the pathogens are destroyed by immune reactions. Figure 01: Allergy According to the Coombs and Gell classification, there are four main types of hypersensitivity reactions. Type I- Immediate Type/ Anaphylactic Mechanism Vasodilation, edema, and contraction of smooth muscles are the pathological changes that take place during the immediate phase of the reaction. -

Vaccine Hesitancy
Vaccine Hesitancy Dr Brenda Corcoran National Immunisation Office Presentation Outline An understanding of the following principles: • Overview of immunity • Different types of vaccines and vaccine contents • Vaccine failures • Time intervals between vaccine doses • Vaccine overload • Adverse reactions • Herd immunity Immunity Immunity • The ability of the human body to protect itself from infectious disease The immune system • Cells with a protective function in the – bone marrow – thymus – lymphatic system of ducts and nodes – spleen –blood Types of immunity Source: http://en.wikipedia.org/wiki/Immunological_memory Natural (innate) immunity Non-specific mechanisms – Physical barriers • skin and mucous membranes – Chemical barriers • gastric and digestive enzymes – Cellular and protein secretions • phagocytes, macrophages, complement system ** No “memory” of protection exists afterwards ** Passive immunity – adaptive mechanisms Natural • maternal transfer of antibodies to infant via placenta Artificial • administration of pre- formed substance to provide immediate but short-term protection (antitoxin, antibodies) Protection is temporary and wanes with time (usually few months) Active immunity – adaptive mechanisms Natural • following contact with organism Artificial • administration of agent to stimulate immune response (immunisation) Acquired through contact with an micro-organism Protection produced by individual’s own immune system Protection often life-long but may need boosting How vaccines work • Induce active immunity – Immunity and immunologic memory similar to natural infection but without risk of disease • Immunological memory allows – Rapid recognition and response to pathogen – Prevent or modify effect of disease Live attenuated vaccines Weakened viruses /bacteria – Achieved by growing numerous generations in laboratory – Produces long lasting immune response after one or two doses – Stimulates immune system to react as it does to natural infection – Can cause mild form of the disease (e.g. -

The Challenge of Achieving Universal Access to Vaccines
Keynote Address: The Challenge of Achieving Universal Access to Vaccines WIPO & AMF Seth Berkley M.D, CEO 8 November 2017 www.gavi.org 1 Vaccine landscape WIPO 8 November 2017 The world before vaccines Examples of major disease outbreaks Polio Cholera New York pandemic 1916 Europe 6,000 deaths 1829-1851 >200,000 deaths Yellow fever Philadelphia Smallpox 1793 epidemic >5,000 India deaths 1974 15,000 deaths Flu pandemic 1918-1920 > 50-100 million deaths worldwide WIPO 8 November 2017 History of vaccine development Source: Delaney et.al. 2014 WIPO 8 November 2017 Cumulative number of vaccines developed licensed 50+ vaccines Lyme OspA, protein (1998) Tuberculosis (Bacille Calmette-Guérin) Pneumococcal conjugate, heptavalent* (2000) 1927 Typhus Varicella (1995) Meningococcal quadrivalent conjugates* (2005) Japanese encephalitis (Vera-cell) (2009) 1938 Cholera (recombinant Toxin B) # (1993) Cholera (WC only) (2009) Tetanus toxoid Cholera (WC-rBC) (1991) Human papillomavirus recombinant bivalent (2009) Influenza H. influenzaeconjugate* (1987) Quadrivalent influenza vaccines (2012) Typhoid Cholera Pertussis 1936 Meningococcal C and Y and 1886 1896 1926 H. influenza type B polysaccharide (1985) Haemophilusinfluenza type b (2012) Adenovirus (1980) Meningococcal B (2013) Smallpox Diphtheria Yellow Rabies, cell culture (1980) Influenza vaccine (baculovirus) (2013) 1798 toxoid Fever Typhoid conjugate vaccine (2013) Rabies Plague Meningococcal polysaccharides (1974) 1923 1935 Human papillomavirus, 9-valent (2014) 1885 Rubella, live (1969) 1897 vaccines -

Package Inserts
Individuals using assistive technology may not be able to fully access the information contained in this file. For assistance, please send an e-mail to: [email protected] and include 508 Accommodation and the title of the document in the subject line of your e-mail. HIGHLIGHTS OF PRESCRIBING INFORMATION -----------------------WARNINGS AND PRECAUTIONS------------------------ These highlights do not include all the information needed to use • Carefully consider benefits and risks before administering VAXELIS to VAXELIS safely and effectively. See full prescribing information for persons with a history of: VAXELIS. - fever ≥40.5°C (≥105°F), hypotonic-hyporesponsive episode (HHE) or VAXELISTM (Diphtheria and Tetanus Toxoids and Acellular Pertussis, persistent, inconsolable crying lasting ≥3 hours within 48 hours after a Inactivated Poliovirus, Haemophilus b Conjugate and Hepatitis B previous pertussis-containing vaccine. (5.2) Vaccine) - seizures within 3 days after a previous pertussis-containing vaccine. (5.2) Suspension for Intramuscular Injection Initial U.S. Approval: 2018 • If Guillain-Barré syndrome occurred within 6 weeks of receipt of a prior vaccine containing tetanus toxoid, the risk for Guillain-Barré syndrome ----------------------------RECENT MAJOR CHANGES ------------------------ may be increased following VAXELIS. (5.3) Dosage and Administration (2.2) 09/2020 • Apnea following intramuscular vaccination has been observed in some ----------------------------INDICATIONS AND USAGE--------------------------- infants born prematurely. The decision about when to administer an VAXELIS is a vaccine indicated for active immunization to prevent intramuscular vaccine, including VAXELIS, to an infant born prematurely diphtheria, tetanus, pertussis, poliomyelitis, hepatitis B, and invasive disease should be based on consideration of the individual infant’s medical status due to Haemophilus influenzae type b. -
An Avoidable Cause of Thymoglobulin Anaphylaxis S
Brabant et al. Allergy Asthma Clin Immunol (2017) 13:13 Allergy, Asthma & Clinical Immunology DOI 10.1186/s13223-017-0186-9 CASE REPORT Open Access An avoidable cause of thymoglobulin anaphylaxis S. Brabant1*, A. Facon2, F. Provôt3, M. Labalette1, B. Wallaert4 and C. Chenivesse4 Abstract Background: Thymoglobulin® (anti-thymocyte globulin [rabbit]) is a purified pasteurised, gamma immune globulin obtained by immunisation of rabbits with human thymocytes. Anaphylactic allergic reactions to a first injection of thymoglobulin are rare. Case presentation: We report a case of serious anaphylactic reaction occurring after a first intraoperative injection of thymoglobulin during renal transplantation in a patient with undiagnosed respiratory allergy to rabbit allergens. Conclusions: This case report reinforces the importance of identifying rabbit allergy by a simple combination of clini- cal interview followed by confirmatory skin testing or blood tests of all patients prior to injection of thymoglobulin, which is formally contraindicated in patients with a history of hypersensitivity to rabbit proteins. Keywords: Thymoglobulin, Anaphylactic allergic reaction, Rabbit proteins Background [7]. Cases of serious anaphylactic reactions to thymo- Thymoglobulin is an IgG fraction purified from the globulin due to rabbit protein allergy are very rare, and serum of rabbits immunised against human thymocytes. consequently, specific tests for rabbit allergy are not The preparation consists of polyclonal antilymphocyte usually performed as part of the pre-transplant assess- IgG directed against T lymphocyte surface antigens, and ment. We report a case of serious anaphylactic reaction induction of profound lymphocyte depletion is though due to rabbit protein allergy following a first injection of to be the main mechanism of thymoglobulin-mediated thymoglobulin. -

Food Fact Sheet: Food Allergy and Food Intolerance
Food Fact Sheet: Food Allergy and Food Intolerance Having to avoid certain foods in your diet can be difficult. But there are a few simple things you can do to help you manage your food allergies - allowing you to stay safe, continue to participate in fun activities and enjoy your food. What is the difference between food allergy and food intolerance? For some people, eating certain foods can lead to an unpleasant and sometimes dangerous physical reaction. The term used to describe all types of reactions to foods is ‘food hypersensitivity’. A 'food allergy' is a reaction involving the immune system (the body’s defence against foreign bodies). Those that do not involve the immune system are often called a ‘food intolerance’. It is important to identify and manage foods that trigger any symptoms in an appropriate way. Food allergy Proteins within foods can trigger immediate (within two hours) or delayed symptoms (up to several days later). Immediate food allergy (IgE mediated food allergy) Immediate reactions to foods occur when your immune system reacts to a normally harmless protein in food, due to the creation of Immunoglobulin E (IgE). This results in the release of chemicals (e.g. histamine) which trigger allergic symptoms. These symptoms are usually in the skin (itching/swelling), or gut (vomiting, diarrhoea). Other symptoms can include breathing problems and in rare cases an extreme allergic reaction called anaphylaxis. Delayed food allergy (non IgE mediated food allergy) Delayed reactions to foods still involve your immune system, but there is a different type of immune reaction involved. Symptoms typically occur in the gut (vomiting, diarrhoea, constipation) and/or the skin (atopic eczema). -

Allergy, Hypersensitivity, Angioedema, and Anaphylaxis Episode Overview
CrackCast Show Notes –Allergy and Anaphylaxis – October 2017 www.canadiem.org/crackcast Chapter 109 – Allergy, Hypersensitivity, Angioedema, and Anaphylaxis Episode Overview Key Points: 1. A history of sudden urticarial rash accompanied by respiratory difficulty, abdominal pain, or hypotension, strongly favors the diagnosis of anaphylaxis. 2. Epinephrine is the first-line treatment in patients with anaphylaxis: give it immediately. 3. There are no absolute contraindications to the use of epinephrine in the setting of anaphylaxis. 4. Antihistamines and corticosteroids are second- and third-line agents in the management of anaphylaxis and should not replace or precede epinephrine. 5. Consider prolonged observation or admission for patients who: a. Experience protracted anaphylaxis, hypotension, or airway involvement; b. Receive IV epinephrine or more than two doses of IM epinephrine; c. Or have poor outpatient social support. 6. Patients discharged after an anaphylactic event should be prescribed an EpiPen and instructed on its use. 7. Patients with refractory hypotension may require glucagon (receiving beta-blockage) or a continuous IV epinephrine infusion. 8. Non-histaminergic angioedema (non-allergic angioedema) does not typically respond to epinephrine and antihistamines. New drugs, including berinert, icatibant, ecallantide, and Ruconest have been approved for use in HAE. FFP has been used with varying success in HAE, ACID, and ACE inhibitor–induced angioedema. NOTE: ACID: acquired C1 esterase deficiency (ACED) Core Questions: 1. List the four types of Gell and Coombs classifications of immune reaction and give examples of each 2. List four etiologic agents causing anaphylaxis by immunologic mechanisms 3. List six mediators of anaphylaxis and their physiologic actions and clinical manifestations 4.