Cmv-Infection in Gay Men with Aids
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-
With Gerry Conway & Dan Jurgens
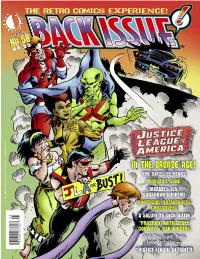
Justice League of America TM & © DC Comics. All Rights Reserved. 0 7 No.58 August 2012 $ 8 . 9 5 1 82658 27762 8 THE RETRO COMICS EXPERIENCE! IN THE BRONZE AGE! “JUSTICE LEAGUE DETROIT”! UNOFFICIAL JLA/AVENGERS CONWAY & DAN JURGENS A SALUTE TO DICK DILLIN “PRO2PRO” WITH GERRY THE SATELLITE YEARS SQUADRON SUPREME And the team fans love to hate — INJUSTICE GANG MARVEL’s JLA, CROSSOVERS ® The Retro Comics Experience! Volume 1, Number 58 August 2012 Celebrating the Best Comics of the '70s, '80s, '90s, and Beyond! EDITOR Michael “Superman”Eury PUBLISHER John “T.O.” Morrow GUEST DESIGNER Michael “Batman” Kronenberg COVER ARTIST ISSUE! Luke McDonnell and Bill Wray COVER COLORIST BACK SEAT DRIVER: Editorial by Michael Eury.........................................................2 Glenn “Green Lantern” Whitmore PROOFREADER Whoever was stuck on Monitor Duty FLASHBACK: 22,300 Miles Above the Earth .............................................................3 A look back at the JLA’s “Satellite Years,” with an all-star squadron of creators SPECIAL THANKS Jerry Boyd Rob Kelly Michael Browning Elliot S! Maggin GREATEST STORIES NEVER TOLD: Unofficial JLA/Avengers Crossovers................29 Rich Buckler Luke McDonnell Never heard of these? Most folks haven’t, even though you might’ve read the stories… Russ Burlingame Brad Meltzer Snapper Carr Mike’s Amazing Dewey Cassell World of DC INTERVIEW: More Than Marvel’s JLA: Squadron Supreme....................................33 ComicBook.com Comics SS editor Ralph Macchio discusses Mark Gruenwald’s dictatorial do-gooders Gerry Conway Eric Nolen- DC Comics Weathington J. M. DeMatteis Martin Pasko BRING ON THE BAD GUYS: The Injustice Gang.....................................................43 Rich Fowlks Chuck Patton These baddies banded together in the Bronze Age to bedevil the League Mike Friedrich Shannon E. -

Hotel Executive
HotelExecutive.com - Newswire - Liberty Group of Companies Acquires Assets in Florida 1/17/11 4:08 PM Login Subscribe to Business Review Receive Daily Digest Advertise About us Receive the free Daily Digest Sign up! Home Hotel Business Review Hotel Newswire Hotel Newswire Free daily news distribution for hotels. Online Hotel Merchandising Insights. Only on VTV Channel. Share | Acquisitions & Hotel Openings Liberty Group of Companies Acquires Assets in Florida January 6, 2011 - Liberty Group of Companies is proud to announce that it has acquired over $70,000,000 in distressed real estate assets and non-performing loans secured by hospitality assets since January 2010. The Liberty Group of Companies, founded in 1980 by hotelier Raxit N. Shah and led by his son Punit R. Shah, has been actively pursuing undervalued off-market acquisitions that present attractive investment opportunities as part of its conservative but aggressive growth strategy within the hospitality sector. Key acquisitions in 2010 have included seven upper-midscale limited service hotels Guest Sourcing: The Art of Turning Your Guests into Content Producers (through a combination of direct asset acquisition and senior debt purchase) and a senior- living facility all located throughout Florida. Click here to learn more "Our opportunistic approach to our investments, primarily in the Southeastern United States, demonstrates our confidence in the hospitality sector and specifically in our core markets. Hotel Business Review Suggested Reading Each of our investments presents a value-add approach where we focus on the asset The Real Cost of Online Travel Agencies repositioning thereby creating a long-term capital enhancement," says Punit R. -

2014 European Hotel Transactions
MARCH 2015 | PRICE £500 2014 EUROPEAN HOTEL TRANSACTIONS Jill Barthel – HVS London ConsulƟ ng & ValuaƟ on Analyst Adrian Ruch – HVS Hodges Ward EllioƩ Analyst www.hvs.com HVS London and HVS Hodges Ward Elliott www.hvshwe.com 7-10 Chandos St, London W1G 9DQ, UK This license lets others remix, tweak, and build upon your work non-commercially, as long as they credit you and license their new creations under the identical terms. Others can download and redistribute your work just like the by-nc-nd license, but they can also translate, make remixes, and produce new stories based on your work. All new work based on yours will carry the same license, so any derivatives will also be non-commercial in nature. Highlights PARIS MARRIOTT HOTEL CHAMPS-ELYSÉES European hotel transaction volume totalled €14.4 billion in 2014, an increase of 86% on 2013. This igure represents a new record since the onset of the global inancial crisis and marks a continuation of the market recovery seen in 2013. Not only was 2014 the highest year since the €20.3 billion recorded in 2006, it was also the fourth highest year on record;¹ Transactions were evenly spread over the year, with slightly higher volumes in the second quarter, owing to the sales of the Paris Marriott Hotel Champs-Elysées (€345 million, €1.8 million per room) and Le Méridien Etoile (€280 million, €237,000 per room), and in the fourth quarter, the sale of Louvre Hotels Group (€1.2 billion); With regard to single asset transactions, 2014 witnessed the highest level of single both Ireland and Spain experienced a asset hotel transaction volume on record, strong year, marking a recovery in their while portfolio sales achieved the ifth struggling economies; highest volume on record, behind 2001, 2005, 2006 and 2007; While Middle Eastern investment decreased after an extremely strong Total portfolio transaction volume 2013, investment by North American and (€6.9 billion) doubled compared to Asian entities increased substantially 2013. -

The Starman Omnibus Vol. 2 PDF Book
THE STARMAN OMNIBUS VOL. 2 PDF, EPUB, EBOOK James Robinson | 416 pages | 11 Sep 2012 | DC Comics | 9781401221959 | English | New York, NY, United States The Starman Omnibus Vol. 2 PDF Book Martin Luther King Jr. Collects Starman 2nd Series and 1,,, Stars and S. It's stuck somewhere between a character-driven indie comic like Strangers In Paradise and a classic DC superhero comic. Fate, the Shade, and the Golden Age Sandman. In the pages of Starman we get a looser, more cartoony style from Harris, but with hint at the refined style he currently draws in. This made me realize that I am not a huge fan of Tony Harris's art. All rights reserved. Zero Hour: Crisis in Time 25th Anniversary. However, he got stranded on Earth, the Kingdom Come universe, thus witnessing the dramatic events on that Earth and receiving added damage to his frail mind, worsened by the lack of the advanced medication to which he had had access in his own time. Of course there is his wise mentor in his father, Ted. Books by James Robinson. Help Learn to edit Community portal Recent changes Upload file. Creepy Eerie. From Wikipedia, the free encyclopedia. Much like Opal City itself, Robinson crafts a fantastic blend of old and new in his story. He pickpocketed a pistol and fired on the group. An old guy now, but his thought process is shown here, and his arc striked curiosity inside of me: now I want to know more about the character, and how he was when younger This book gave me a bunch of mixed feelings. -

Heroclix Campaign
HeroClix Campaign DC Teams and Members Core Members Unlock Level A Unlock Level B Unlock Level C Unless otherwise noted, team abilities are be purchased according to the Core Rules. For unlock levels listing a Team Build (TB) requisite, this can be new members or figure upgrades. VPS points are not used for team unlocks, only TB points. Arkham Inmates Villain TA Batman Enemy Team Ability (from the PAC). SR Criminals are Mooks. A 450 TB points of Arkham Inmates on the team. B 600 TB points of Arkham Inmates on the team. Anarky, Bane, Black Mask, Blockbuster, Clayface, Clayface III, Deadshot, Dr Destiny, Firefly, Cheetah, Criminals, Ambush Bug. Jean Floronic Man, Harlequin, Hush, Joker, Killer Croc, Mad Hatter, Mr Freeze, Penguin, Poison Ivy, Dr Arkham, The Key, Loring, Kobra, Professor Ivo, Ra’s Al Ghul, Riddler, Scarecrow, Solomon Grundy, Two‐Face, Ventriloquist. Man‐Bat. Psycho‐Pirate. Batman Enemy See Arkham Inmates, Gotham Underground Villain Batman Family Hero TA The Batman Ally Team Ability (from the PAC). SR Bat Sentry may purchased in Multiples, but it is not a Mook. SR For Batgirl to upgrade to Oracle, she must be KOd by an opposing figure. Environment or pushing do not count. If any version of Joker for KOs Level 1 Batgirl, the player controlling Joker receives 5 extra points. A 500 TB points of Batman members on the team. B 650 TB points of Batman members on the team. Azrael, Batgirl (Gordon), Batgirl (Cain), Batman, Batwoman, Black Catwoman, Commissioner Gordon, Alfred, Anarky, Batman Canary, Catgirl, Green Arrow (Queen), Huntress, Nightwing, Question, Katana, Man‐Bat, Red Hood, Lady Beyond, Lucius Fox, Robin (Tim), Spoiler, Talia. -

LGBTQ+ GUIDE to COMIC-CON@HOME 2021 Compiled by Andy Mangels Edited by Ted Abenheim Collage Created by Sean (PXLFORGE) Brennan
LGBTQ+ GUIDE TO COMIC-CON@HOME 2021 Compiled by Andy Mangels Edited by Ted Abenheim Collage created by Sean (PXLFORGE) Brennan Character Key on pages 3 and 4 Images © Respective Publishers, Creators and Artists Prism logo designed by Chip Kidd PRISM COMICS is an all-volunteer, nonprofit 501c3 organization championing LGBTQ+ diversity and inclusion in comics and popular media. Founded in 2003, Prism supports queer and LGBTQ-friendly comics professionals, readers, educators and librarians through its website, social networking, booths and panel presentations at conventions. Prism Comics also presents the annual Prism Awards for excellence in queer comics in collaboration with the Queer Comics Expo and The Cartoon Art Museum. Visit us at prismcomics.org or on Facebook - facebook.com/prismcomics WELCOME We miss conventions! We miss seeing comics fans, creators, pros, panelists, exhibitors, cosplayers and the wonderful Comic-Con staff. You’re all family, and we hope everyone had a safe and productive 2020 and first half of 2021. In the past year and a half we’ve seen queer, BIPOC, AAPI and other marginalized communities come forth with strength, power and pride like we have not seen in a long time. In the face of hate and discrimination we at Prism stand even more strongly for the principles of diversity and equality on which the organization was founded. We stand with the Black, Asian American and Pacific Islander, Indigenous, Latinx, Transgender communities and People of Color - LGBTQ+ and allies - in advocating for inclusion and social justice. Comics, graphic novels and arts are very powerful mediums for marginalized voices to be heard. -

X-Men, Dragon Age, and Religion: Representations of Religion and the Religious in Comic Books, Video Games, and Their Related Media Lyndsey E
Georgia Southern University Digital Commons@Georgia Southern University Honors Program Theses 2015 X-Men, Dragon Age, and Religion: Representations of Religion and the Religious in Comic Books, Video Games, and Their Related Media Lyndsey E. Shelton Georgia Southern University Follow this and additional works at: https://digitalcommons.georgiasouthern.edu/honors-theses Part of the American Popular Culture Commons, International and Area Studies Commons, and the Religion Commons Recommended Citation Shelton, Lyndsey E., "X-Men, Dragon Age, and Religion: Representations of Religion and the Religious in Comic Books, Video Games, and Their Related Media" (2015). University Honors Program Theses. 146. https://digitalcommons.georgiasouthern.edu/honors-theses/146 This thesis (open access) is brought to you for free and open access by Digital Commons@Georgia Southern. It has been accepted for inclusion in University Honors Program Theses by an authorized administrator of Digital Commons@Georgia Southern. For more information, please contact [email protected]. X-Men, Dragon Age, and Religion: Representations of Religion and the Religious in Comic Books, Video Games, and Their Related Media An Honors Thesis submitted in partial fulfillment of the requirements for Honors in International Studies. By Lyndsey Erin Shelton Under the mentorship of Dr. Darin H. Van Tassell ABSTRACT It is a widely accepted notion that a child can only be called stupid for so long before they believe it, can only be treated in a particular way for so long before that is the only way that they know. Why is that notion never applied to how we treat, address, and present religion and the religious to children and young adults? In recent years, questions have been continuously brought up about how we portray violence, sexuality, gender, race, and many other issues in popular media directed towards young people, particularly video games. -

Justice League of America the Silver Age: Vol 1 Free
FREE JUSTICE LEAGUE OF AMERICA THE SILVER AGE: VOL 1 PDF Various,Gardner F Fox | 144 pages | 23 Feb 2016 | DC Comics | 9781401261115 | English | United States Justice League of America: The Silver Age Vol. 1 by Gardner F. Fox Goodreads helps you keep track of books you want to read. Want to Read saving…. Want to Read Currently Reading Read. Other editions. Enlarge cover. Error rating book. Refresh and try again. Open Preview See a Problem? Details if other :. Thanks for telling us about the problem. Return to Book Page. Fox. Mike Sekowsky Illustrator. Bernard Sachs Illustrator. Wonder Woman. The Flash. Green Lantern. The Martian Manhunter. Green Arrow. As individuals, their names are legend. Together, they are even greater than the sum of their parts. They are the Justice League of America, and they stand for truth, justice and the American way! Since they were first commissioned by renowned DC Comics editor Julius Schwartz inthe Justice League has thrilled audiences across the globe in tales that span time and space. Get A Copy. Paperbackpages. More Details Other Editions 1. Friend Reviews. To see what your friends thought of this book, please sign up. To ask other readers questions about Justice League of Americaplease sign up. Be the first to ask a question about Justice League of America. Lists with This Book. This book is not yet featured on Listopia. Community Reviews. Showing Average rating 3. Rating details. More filters. Sort order. Jun 18, Matt rated it it was amazing. Awesome artwork and good, solid writing with classic storylines and adventures are captured in this collection. -

American Comic Books & the Aids Crisis
FATAL ATTRACTIONS: AMERICAN COMIC BOOKS & THE AIDS CRISIS A MASTER’S FINAL PROJECT FOR THE DEPARTMENT OF AMERICAN STUDIES Sean A. Guynes FATAL ATTRACTIONS: AMERICAN COMIC BOOKS AND THE AIDS CRISIS A Master’s Final Project Presented by SEAN A. GUYNES Submitted to the Department of American Studies, University of Massachusetts Boston, in partial fulfillment of the requirements for the degree of MASTER OF ARTS June 2015 American Studies Program © 2015 by Sean A. Guynes All rights reserved Cover design after Alaniz (2014). Cover art by Richard Bennett, Uncanny X-Men #303 (August 1993), © Marvel Worldwide, Inc. Art below from 7 Miles A Second, story by David Wojnarowicz, art by James Romberger and Marguerite Van Cook (1996). ABSTRACT FATAL ATTRACTIONS: AMERICAN COMIC BOOKS AND THE AIDS CRISIS June 2015 Sean A. Guynes, B.A., Western Washington University M.A., University of Massachusetts Boston Advisor: Aaron Lecklider, Ph.D. Second Reader: Rachel Rubin, Ph.D. Between 1988 and 1994 American comic books engaged the politics, problematics, and crises of the AIDS epidemic by inserting the virus and its social, cultural, and epidemiological effects on gay men into the four-color fantasies of the superhero genre. As the comic-book industry was undergoing major internal changes that allowed for more mature, adult storylines, creators challenged the Comics Code Authority’s 1954 sanction against the representation of homosexuality to create, for the first time, openly gay characters. Creators’ efforts were driven by a desire to recognize the reality of gay men’s lived experiences, especially crucial in the epidemic time of the AIDS crisis. -

The Starman Companion
THE STARMAN SAGA Volume 4 THE STARMAN COMPANION 2 The cover illustrates a scene on page 101 of Volume 2, The Search for the Benefactors. This book is available in four versions: in color (expensive) and black & white (less expensive), and in both casewrap and dust jacket. Visit lulu.com and search by title. 3 THE STARMAN SAGA Volume Four THE STARMAN COMPANION by Michael D. Cooper (assembled by David Baumann) © 2017 by David Baumann, Jon Cooper, and Mike Dodd all rights reserved ABCDE “A Baumann-Cooper-Dodd Enterprise” www.starmanseries.com 4 About the Author Michael D. Cooper is the pseudonym for Jon Cooper, Mike Dodd, and David Baumann, each of whom played a vital role in creating the Starman series. Jon Cooper plotted the stories, Mike Dodd suggested creative plot elements and supervised the stories’ scientific accuracy and plausibility, and David Baumann wrote the text, fine tuning details and developing the characters. Cooper is a computer programmer, Dodd is a social worker and zeppelin builder, and Baumann is an Episcopal priest and martial arts master. TAKE NOTE There are many spoilers in this volume. Anyone who has not yet read the Starman saga in its entirety should not read this book. 5 THE STARMAN SAGA Volume 1: The Dawn of the Starmen Mutiny On Mars (May 19-July 22, 2151) The Runaway Asteroid (July 24-September 10, 2151) “The City of Dust” (July 30, 2049-August 2051) “The Flight of the Olympia” (2110) “The Caves of Mercury” (2112-2113) “The Orphans of Titan” (August 2, 2130) “A Matter of Time” (October 12, 2150) Journey to -

New Comics & Tpbs for the Week of 1/5/10
Thanos Imperative Devestation New Comics & TPBs Ultimate Comics Captain America #1 Weird Worlds #1 for the Week of 1/5/10 Wolverine Best There Is #2 X-Factor #213 Action/Adventure Comics 27 #2 Anita Blake Circus of Damned Ingenue #1 Alternative/Vertigo Comics Billy the Kid Ghastly Fiend London #4 Eric Powell Cvr Alan Moore Writing for Comics GN Bring the Thunder #2 House of Mystery #33 Dracula Company of Monsters #5 Izombie #9 Earp Saints for Sinners #1 Madame Xanadu TP Vol 03 Broken House of Cards Jonah Hex #63 Sweet Tooth #17 Ozma of Oz #3 Ryder on the Storm #2 Horror Comics Terry Moores Echo #27 Choker #5 Torchwood #6 Doc Macabre #2 Transformers Ongoing #15 Edge of Doom #3 Transformers Prime #1 Hack Slash My First Maniac TP Vol 01 Lady Death #1 Lady Death #1 Wrap Cvr Superhero Comics Raise the Dead II #2 Adventure Comics #522 Vampirella #2 Ant-Man & Wasp #3 Walking Dead #80 Avengers Childrens Crusade #4 Avengers Prime #5 Avengers Prime #5 A Adams Var Manga Azrael #16 Gantz TP Vol 15 Batman Beyond #1 Batman Beyond #1 Var Ed Batman Confidential #52 Magazines Brightest Day #17 Clint #4 Brightest Day #17 Var Ed Shonen Jump February 2011 Captain America Hail Hydra #1 DC Comics Presents Lobo #1 Deadpool Corps Prelude TP Kid's Doom Patrol #18 Avengers Earths Mightiest Heroes #3 Essential Iron Man TP Vol 02 New Ed Betty & Veronica Double Digest #187 Freedom Fighters #5 Chip N Dale Rescue Rangers #2 Generation Hope #3 Chip N Dale Rescue Rangers #2 10 Copy Incv Green Hornet #12 Looney Tunes #194 Green Hornet #12 15-Copy Ross Neg Incv Scooby -

American Superhero Comics: Fractal Narrative and the New Deal a Dissertation Presented to the Faculty of the College of Arts
American Superhero Comics: Fractal Narrative and The New Deal A dissertation presented to the faculty of the College of Arts and Sciences of Ohio University In partial fulfillment of the requirements for the degree Doctor of Philosophy Lawrence W. Beemer June 2011 © 2011 Lawrence W. Beemer. All Rights Reserved. 2 This dissertation titled American Superhero Comics: Fractal Narrative and The New Deal by LAWRENCE W. BEEMER has been approved for the English Department of Ohio University and the College of Arts and Sciences by ______________________________ Robert Miklitsch Professor of English ______________________________ Benjamin M. Ogles Dean, College of Arts and Sciences 3 ABSTRACT BEEMER, LAWRENCE W., Ph.D., June 2011, English American Superhero Comics: Fractal Narrative and The New Deal (204 pp.) Director of Dissertation: Robert Miklitsch Coining the term "fractal narrative," this dissertation examines the complex storytelling structure that is particular to contemporary American superhero comics. Whereas other mediums most often require narrative to function as self-contained and linear, individual superhero comics exist within a vast and intricate continuity that is composed of an indeterminate number of intersecting threads. Identical to fractals, the complex geometry of the narrative structure found in superhero comics when taken as a whole is constructed by the perpetual iteration of a single motif that was established at the genre's point of origin in Action Comics #1. The first appearance of Superman institutes all of the features and rhetorical elements that define the genre, but it also encodes it with the specific ideology of The New Deal era. In order to examine this fractal narrative structure, this dissertation traces historical developments over the last seven decades and offers a close reading Marvel Comics' 2006 cross-over event, Civil War.