Impact on Microbiology Laboratory Turnaround Times Following Process Improvements and Total Laboratory Automation
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

DUKE UNIVERSITY School of Medicine Pathologists' Assistant
DUKE UNIVERSITY School of Medicine Pathologists’ Assistant Program Department of Pathology Academic Programs The Department of Pathology at Duke University offers a wide array of training programs to fit individual requirements and goals. The Residency Training program is an ACGME approved program and is available as an Anatomic Pathology/Clinical Pathology combined program, a shorter Anatomic Pathology only program, or an Anatomic Pathology/Neuropathology program. Subspecialty fellowships in Cytopathology, Dermatopathology, Hematopathology, Medical Microbiology, and Neuropathology are also ACGME approved. These programs provide the highest quality of graduate medical education by drawing on the depth and breadth of faculty expertise in the Department in all aspects of anatomic and clinical pathology and the availability of a wide variety of often complex clinical cases seen at Duke University Health System. For medical students interested in a career in Pathology pre-doctoral fellowships, internships and externships are available. Research Training in Experimental pathology can be obtained through Pre- and postdoctoral fellowships of one to five years. All pre-doctoral fellows are candidates for the Ph.D. degree in pathology. The Ph.D. is optional in postdoctoral programs, which provide didactic and research training in various aspects of modern experimental pathology. A two year NAACLS accredited Pathologists’ Assistant Program leads to a Master of Health Science degree, certifies graduates to sit for the ASCP Board of Certification examination, and leads to exciting career opportunities in a variety of anatomic pathology laboratory settings. Pathologists’ assistants are analogous to physician assistants, but with highly specialized training in autopsy and surgical pathology. This profession was pioneered in the Duke Department of Pathology 50 years ago, and is one of only twelve such programs in existence today. -

Department of Experimental Pathology, Immunology and Microbiology 531
Department of Experimental Pathology, Immunology and Microbiology 531 Department of Experimental Pathology, Immunology and Microbiology Interim Chairperson: Zaatari, Ghazi Vice Chairperson: Matar, Ghassan Professors: Abdelnoor, Alexander; Khouri, Samia; Matar, Ghassan; Sayegh, Mohamed; Zaatari, Ghazi Associate Professor: Rahal, Elias Assistant Professors: Al-Awar, Ghassan; El Hajj, Hiba; Shirinian, Margret; Zaraket, Hassan The Department of Experimental Pathology, Immunology and Microbiology offers courses to medical laboratory sciences (MLSP) students as well as nursing, medical, and graduate students. It offers a graduate program (discipline of Microbiology and Immunology) leading to a master’s degree (MS) or doctoral degree (PhD) in Biomedical sciences. The requirements for admission to the graduate program are stated on page 33 of this catalogue. IDTH 203 The immune System in Health and Disease 37.28; 3 cr. See Interdepartmental Courses. IDTH 205 Microbiology and Infectious Diseases 37.28; 5 cr. See Interdepartmental Courses. MBIM 223 Parasitology for MLSP Students 39.39; 4 cr. Second semester. MBIM 237 Microbiology and Immunology for Nursing Degree Students 32.64; 3 cr. A course on the fundamental aspects of medical microbiology and immunology for nursing students. Second semester. MBIM 260 Elective in Infectious Diseases for Medicine III and IV 0.180 A course on basic evaluation, diagnosis, and management of infectious diseases. One month. MBIM 261 Elective in Immunology for Medicine III and IV 0.180 A course that is an introduction to immunological research and its application to clinical practice. One month. MBIM 310 Basic Immunology 32.32; 3 cr. A course on innate and adaptive immune mechanisms, infection and immunity, vaccination, immune mechanisms in tissue injury and therapeutic immunology. -
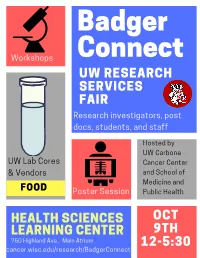
Badgerconnect 2019 Program
Badger Connect Workshops UW RESEARCH SERVICES FAIR Research investigators, post docs, students, and staff Hosted by UW Carbone UW Lab Cores Cancer Center & Vendors and School of Medicine and FOOD Poster Session Public Health HEALTH SCIENCES OCT LEARNING CENTER 9TH 750 Highland Ave., Main Atrium 12-5:30 cancer.wisc.edu/research/BadgerConnect BadgerConnect Research Services Fair October 9th, 2019 12:00 – 5:30 PM, HSLC Atrium AGENDA 12:00 – 12:30pm Registration / Networking Registration table and networking at booths open at 12pm 12:30 – 2:00pm Flash Talks Lunch (Rm 1306 HSLC) ~4 minute flash talks by research services throughout lunch 15’ Break/Networking 2:15 – 2:45pm Workshop Session I Rm 1220 HSLC Rm 1222 HSLC Rm 1244 HSLC Reference Grade De Novo Assemblies and Whole Team Science 101: How to How to create a tissue Topic Transcriptomes: See the Big build, lead, and manage a microarray (TMA) Picture With Pacbio SMRT team that does great science Sequencing UW Translational Research Biotechnology Center DNA Team Science - ICTR and Service Initiatives in Pathology Lab Sequencing Facility UWCCC Vendor n/a Pacific Biosciences n/a 15’ Break/Networking 3:00 – 3:30pm Workshop Session II Rm 1220 HSLC Rm 1222 HSLC Rm 1244 HSLC LabArchives: The Electronic Hyperfinder: Computational Creating Novel Disease Models Topic Lab Notebook Service for Sorting for High-Dimensional with CRISPR Campus Flow Cytometry Data UW Genome Editing and Animal Electronic Lab Notebook Flow Cytometry Lab Service Models Core Service Integrated DNA Technologies, Vendor LabArchives -

Overview of Pathology and Its Related Disciplines - Soheir Mahmoud Mahfouz
MEDICAL SCIENCES – Vol.I -Overview of Pathology and its Related Disciplines - Soheir Mahmoud Mahfouz OVERVIEW OF PATHOLOGY AND ITS RELATED DISCIPLINES Soheir Mahmoud Mahfouz Cairo University, Kasr El Ainy Hospital, Egypt Keywords: Pathology, Pathology disciplines, Pathology techniques, Ancillary diagnostic methods, General Pathology, Special Pathology Contents 1. Introduction 1.1 Pathology coverage 1.1.1 Etiology and Pathogenesis of a Disease 1.1.2 Manifestations of Disease (Lesions) 1.1.3 Phases Of A Disease Process (Course) 1.2 Physician’s approach to patient 1.3 Types of pathologists and affiliated specialties 1.4 Role of pathologist 2. Pathology and its related disciplines 2.1 Cytology 2.1.1 Cytology Samples 2.1.2 Technical Aspects 2.1.3 Examination of Sample and Diagnosis 3. Pathology techniques and ancillary diagnostic methods 3.1 Macroscopic pathology 3.2 Light Microscopy 3.3 Polarizing light microscopy 3.4 Electron microscopy (EM) 3.5 Confocal Microscopy 3.6 Frozen section 3.7 Cyto/histochemistry 3.8 Immunocyto/histochemical methods 3.9 Molecular and genetic methods of diagnosis 3.10 Quantitative methods 4. Types of tests used in pathology 4.1 DiagnosticUNESCO tests – EOLSS 4.2 Quantitative tests 4.3 Prognostic tests 5. The scope of SAMPLEpathology & its main divisions CHAPTERS 6. Conclusions Glossary Bibliography Biographical sketch Summary Pathology is the science of disease. It deals with deviations from normal body function and ©Encyclopedia of Life Support Systems (EOLSS) MEDICAL SCIENCES – Vol.I -Overview of Pathology and its Related Disciplines - Soheir Mahmoud Mahfouz structure. Many disciplines are involved in the study of disease, as it is necessary to understand the complex causes and effects of various disorders that affect the organs and body as a whole. -

MEDICAL UNIVERSITY of SOUTH CAROLINA Charleston, SC
MEDICAL UNIVERSITY OF SOUTH CAROLINA Charleston, SC PROGRAMS OFFERED The Department of Pathology and Laboratory Medicine of the Medical University of South Carolina offers a fully accredited training program in anatomic and clinical pathology (AP/CP). The AP/CP program consists of a 39 month core curriculum with 9 months of elective. Anatomic Pathology core rotations include autopsy pathology/forensic pathology, surgical pathology, cytopathology, dermatopathology and VA pathology. Clinical Pathology core rotations include hematopathology, immunopathology, clinical chemistry, microbiology, tranfusion medicine, apheresis, histocompatibility laboratory, molecular pathology, cytogenetics, VA pathology, laboratory management and informatics. Nine months elective time is available for more in-depth studies in areas of special interest and/or research. A graduate (PhD) program in experimental pathology is available and may be coordinated with the residency training program. Fellowships are offered at the discretion of the Chair in forensic pathology, dermatopathology, cytopathology, surgical pathology, gastrointestinal pathology, hematopathology and clinical chemistry. TYPES AND NUMBERS OF APPOINTMENTS The institution is accredited for twenty-two residency positions in anatomic pathology and clinical pathology, with an even distribution of residents at all levels. Persons seeking the PhD degree in experimental pathology must meet the requirements of the College of Graduate Studies, Medical University of South Carolina. The department participates -
Pathology: a Career in Medicine the Study of the Nature of Disease, Its Causes, Processes, Development, and Consequences
PATHOLOGY A Career in Medicine The Intersociety Council for Pathology Information (ICPI) www.pathologytraining.org 2015 Pathology: A Career in Medicine The study of the nature of disease, its causes, processes, development, and consequences. Pathology is the medical specialty that provides a scientific foundation for medical practice The pathologist is a physician who specializes in the diagnosis and management of human disease by laboratory methods. Pathologists function in three broad areas: as diagnosticians, as teachers, and as investigators. Fundamental to the discipline of pathology is the need to integrate clinical information with physiological, biochemical and molecular laboratory studies, together with observations of tissue alterations. Pathologists in hospital and clinical laboratories practice as consultant physicians, developing and applying knowledge of tissue and laboratory analyses to assist in the diagnosis and treatment of individual patients. As teachers, they impart this knowledge of disease to their medical colleagues, to medical students, and to trainees at all levels. As scientists, they use the tools of laboratory science in clinical studies, disease models, and other experimental systems, to advance the understanding and treatment of disease. Pathology has a special appeal to those who enjoy solving disease-related problems, using technologies based upon fundamental sciences ranging from biophysics to molecular genetics, as well as tools from the more traditional disciplines of anatomy, biochemistry, pharmacology, physiology and microbiology. The Pathologist in Patient Care The pathologist uses diagnostic and screening tests to identify and interpret the changes that characterize different diseases in the cells, tissues, and fluids of the body. Anatomic pathology involves the analysis of the A biosample robot prepares specimens for gross and microscopic structural changes caused by testing disease in tissues and cells removed during biopsy procedures, in surgery, or at autopsy. -

Editorial Note on Medical Microbiology & Diagnosis – Clinical
Manuscript no.- JMMD-2021-5 Article type- Editorial Received date- 20-01-2021 Accepted- 20-01-2021 Publish date-23-01-2021 Editorial Note on Medical Microbiology & Diagnosis – Clinical Microbial Pathology Tirpude RJ Defence Institute of Physiology and Allied Sciences Address for Correspondence: Tirpude RJ, Defence Institute of Physiology and Allied Sciences, Delhi - 110054, India. Tel-9869217101, E-mail: [email protected] Editorial Clinical pathology is concerned with the diagnosis of disease based on laboratory analysis of body fluids like urine and blood. It deals with the tools of microbiology like macroscopic, microscopic, analyzers and cultures. It covers microbiology, host-pathogen interaction and immunology related to infectious agents, including bacteria, fungi, viruses and protozoa. It also accepts papers in the field of clinical microbiology, with the exception of case reports. The pathogenesis of a disease is the biological mechanism that leads to the diseased state. It also describes the origin and development of the disease, and whether it is acute, chronic, or recurrent. Medical microbiology involves the identification of microorganisms for the diagnosis of infectious diseases and the assessment of likely response to specific therapeutic interventions. Major categories of organisms include bacteria, mycobacteria, fungi, viruses, and parasites. Microbiological methods combined with clinical symptoms, additional laboratory tests, and imaging techniques are used in combination to distinguish a true disease- associated infection from colonization with normal flora or other conditions, such as malignancies, inflammatory disorders, or autoimmune disorders, all of which have unique therapies and prognoses for the patient. Laboratories combine the use of traditional microscopy and culture methods, with a rapidly evolving set of molecular and proteomic techniques. -

Msk Pathology Initiatives Innovations Review Accomplishments
MSK PATHOLOGY INITIATIVES INNOVATIONS REVIEW ACCOMPLISHMENTS MSKCC Pathology Fellowship Directors 3RD QUARTER 2018 Research Spotlight HANNAH WEN, MD, PhD Hannah Wen, MD, PhD, first came to Memorial Sloan Kettering They compared the genomic landscape of MBCs with triple- Cancer Center as a fellow in 2008 before joining the Breast team in negative invasive ductal carcinomas and assessed WNT and PI3K/ 2010. When she talks about her work, especiatlly her research, she AKT/mTOR pathway activity. Among their findings, MBCs were sounds as enthusiastic as if it were her first day of fellowship. genetically complex and tended to have a high frequency of PI3 kinase “I love research! My clinical work is mostly breast cancer and WNT signaling pathways alterations. That’s unusual for a triple- diagnosis, so I’ll do research late in the day or come in on weekends,” negative disease and good news from a treatment perspective, since she says. “When you have such a rich environment, so many cases, they’re targetable alterations. and good technology, it’s satisfying and fun.” Dr. Wen’s projects include studies on triple negative breast Tumor Infiltrating Lymphocytes cancer, tumor infiltrating lymphocytes, and more. Dr. Wen’s work on tumor infiltrating lymphocytes, which are usually seen in triple negative breast cancer and HER2-positive Triple Negative Breast Cancer cancer, shows promise for near-term clinical applications. “We Dr. Wen’s research interest is in triple negative breast cancer believe those lymphocytes play an important role in the immune (TNBC), defined as breast cancer that does not express estrogen system, helping our body to defend against tumor cells,” Dr. -

UNIVERSITY of TEXAS MEDICAL BRANCH Galveston, TX
UNIVERSITY OF TEXAS MEDICAL BRANCH Galveston, TX PROGRAMS OFFERED The University of Texas Medical Branch offers fully accredited training programs in both anatomic and clinical pathology, and offers advanced fellowship training in surgical pathology, cytopathology, and dermatopathology, leading to subspecialty certification by the American Board of Pathology. Fellowship training is also offered in clinical microbiology and clinical chemistry leading to certification by the American Society for Microbiology and the American Assocation for Clinical Chemistry respectively. Residents may elect three years of anatomic pathology or three years of clinical pathology, each leading to certification, or a four year program in anatomic and clinical pathology leading to certification in both areas. The advanced fellowships described above lead to eligibility for special competence certification if such is available from the Board. All reasonable attempts are made to fit the program to the career objectives of the individual. In the anatomic pathology program, residents assume increasing diagnostic responsibility under staff supervision in surgical pathology, cytopathology, autopsy, dermatopathology, forensic pathology, pediatric pathology, neuropathology, liver pathology, transplantation pathology, and renal immunopathology. Clinical pathology offers a basic background in all disciplines of laboratory medicine, including clinical chemistry, hematopathology, coagulation, microbiology, transfusion medicine, cytogenetics, molecular diagnostics, laboratory administration and informatics. Diagnostic Management Teams (DMT) provide comprehensive diagnostic interpretation of anatomic and clinical pathology data to our clinicians. Information comes from our diagnostic experts as a personalized, expert driven narrative about the differential diagnosis for a patient evaluation. In addition, we have developed personalized interpretations that are disease-specific and have input not only from the pathologist, but also from investigators studying that particular disease. -

Cell Injury David S
91731_ch01 12/1/06 10:10 AM Page 1 1 Cell Injury David S. Strayer Emanuel Rubin Reactions to Persistent Stress and Cell Injury Ionizing Radiation Proteasomes Viral Cytotoxicity Atrophy as Adaptation Chemicals Atrophy as an Active Process Abnormal G Protein Activity Hypertrophy Cell Death Hyperplasia Morphology of Necrosis Metaplasia Necrosis from Exogenous Stress Dysplasia Necrosis from Intracellular Insults Calcification Apoptosis (Programmed Cell Death) Hyaline Initiators of Apoptosis Mechanisms and Morphology of Cell Injury Biological Aging Hydropic Swelling Maximal Life Span Subcellular Changes Functional and Structural Changes Ischemic Cell Injury The Cellular Basis of Aging Oxidative Stress Genetic Factors Nonlethal Mutations that Impair Cell Function Somatic Damage Intracellular Storage Summary Hypothesis of Aging Ischemia/Reperfusion Injury athology is basically the study of structural and functional ab- between its internal milieu and a hostile environment. The normalities that are expressed as diseases of organs and systems. plasma membrane serves this purpose in several ways: PClassic theories of disease attributed disease to imbalances • It maintains a constant internal ionic composition against or noxious effects of humors on specific organs. In the 19th cen- very large chemical gradients between the interior and exte- tury, Rudolf Virchow, often referred to as the father of modern rior compartments. pathology, proposed that injury to the smallest living unit of the body, the cell, is the basis of all disease. To this day, clinical and • It selectively admits some molecules while excluding or ex- experimental pathology remain rooted in this concept. truding others. Teleology—the study of design or purpose in nature—has • It provides a structural envelope to contain the informa- long since been discredited as part of scientific investigation. -

Breast Epithelium Procurement from Stereotactic Core Biopsy Washings: Flow Cytometry-Sorted Cell Count Analysis1
428 Vol. 8, 428–432, February 2002 Clinical Cancer Research Breast Epithelium Procurement from Stereotactic Core Biopsy Washings: Flow Cytometry-sorted Cell Count Analysis1 Daniel L. Stoler,2 Carleton C. Stewart, and INTRODUCTION Paul C. Stomper Identification and characterization of breast tumor markers Departments of Experimental Pathology [D. L. S.], Flow Cytometry has important implications for breast cancer screening and di- [C. C. S.], and Diagnostic Imaging [P. C. S.], Roswell Park Cancer agnosis, for assessing prognosis, and for predicting response to Institute, Buffalo, New York 14263 individual therapies. In addition, determination of the molecular and/or genetic changes that precede or accompany the cancer can have significant effects on patient management and out- ABSTRACT come. The greatest impact may be through defining these Purpose: Molecular studies of breast lesions have been changes in early lesions that have been implicated in breast constrained by difficulties in procuring adequate tissues for tumorigenesis, such as atypia, DCIS,3 and minimally invasive analyses. Standard procedures are restricted to larger, pal- disease. However, a majority of these lesions are clinically pable masses or the use of paraffin-embedded materials, occult and detected during screening mammography. Standard precluding facile procurement of fresh specimens of early procedures for fresh tissue procurement are limited to larger, lesions. We describe a study to determine the yield and palpable masses, and the use of paraffin-embedded materials characteristics of sorted cell populations retrieved in core precludes the use of fresh tissues. Procurement of fresh epithe- needle biopsy specimen rinses from a spectrum of breast lial cell specimens from earlier lesions poses unique challenges. -

Biochemical Challenge of Microbial Pathogenicity
BACTERIOLOGICAL REVIEWS, Sept., 1968, p. 164-184 Vol. 32, No. 3 Copyright c 1968 American Society for Microbiology Priiited in U.S.A. Biochemical Challenge of Microbial Pathogenicity H. SMITH Depcartmenit of Microbiology, The Uuiiversity, of Birminiglhamii, Bir-iniglhami1, Eniglantd INTRODUCTION.. ..... 164 STUDIES OF BACTERIAL PATHOGENICITY ..... .... 165 Difficulty of'Inivestigati,ig Biochenmicail Mechanlisms of PathogenlicitY. 165 Studies of Bacterial Behavior In Vivo.... 165 ASPECTS OF BACTERIAL PATHOGENICITY REQUIRING ATTENTION- 166 Intitiationl of Inlfectioni 166 Growth and Multiplication In Vivo. 166 Aggressive Activity........... 167 Inhihitors of blood atnd tissie hbactericidins............ 167 Inihibitors of' the actioni of plipagocvtes............................ 168 (i) Iihibitors of conltact. ..... 168 (ii) l liihi tor-s of intgestionl . 168 (iii) Inihibitors of initralcellutlair hactericidins: prom2otioni of intracellular growvth. 169 (iv) Repercussionu of ietertogeiueity of pliagocytic finIuctiOni Oni microbial requiire- ments for caggressitis. 170 Toxic Activity....................... 171 Toxi,is of overridling importalnce in disease 171 Toxi,Is which aire siglnificanlt bhlt niot the o;uly factors respoursible.for dlisecase. 171 Toxilns produced ini vitro hblt of ioiknown importance ill disea.se. 171 Toxic effe(cts in vivo ofhacteria which aippear to produice lo rolevait to-viii ifi vitro 171 (i) Toxilns revealedbl vsticlyinig hbacteria in more iiactuiral enviro.iciltsWi 172 (ii) Rolev of hypersensitiviity ili toxic maniJe*stations of disesn.A. 173 Relcatioli o' Protective Anitigens to Virule,ice Factors... 174 Biochenicall Bases of Host anid Tissuce Specificity,.... 174 Role ofucireaise ili kidney, localizations ofCoryniehacteriuon rena(ile and(i Proteuis mirabilis. 175 Role of ervthritol in the tissute specificity of the brlucellae 175 UNANSWERED QUESTIONS RELATING TO THE PATHOGENICITN' OF VIRUSES, FUNGI, PROTOZOA, AND MALIGNANT CELLS.