AG Jarrams. a Dermatological Survey of the Gurkha Brigade
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

5906 Supplement to the London Gazette, 13 December, 1949
5906 SUPPLEMENT TO THE LONDON GAZETTE, 13 DECEMBER, 1949 CENTRAL CHANCERY OF THE .ORDERS OF Brigadier (temporary) IN. D. RICE (5783), Buffs. KNIGHTHOOD. Brigadier (temporary) C. G. ROBINS (13950), late St. James's Palace, S.W.I. Y. & L. Brigadier (temporary) F. H. C. ROGERS, C.B.E.. December, 1949. D.S.O., M.C. (17114), late R.A. The RING has 'been graciously pleased to approve Colonel A. E. CAMPBELL (30235), late R.A.M.C. the award of the British Empire Medal (Military Division), in recognition of gallant and distinguished Employed List. services in Malaya during the period 1st January, Lieutenant-Colonel R. L. K. ALLEN, O.B.E. (6183). 1949, to 30th June, 1949, to the undermentioned:— ROYAL ARMOURED .CORPS. MYA/ 18019241 Warrant Officer Class I (acting) Royal Tank Regiment. ATTAM BIN YATIN, Royal Army Service Corps. Lieutenant-Colonel (temporary) S. P. WOOD 7662953 Staff Sergeant John Milner Buchanan (45005). BONELL, Royal Army Pay Corps. Major (temporary) S. P. M. SUTTON, M.C. (7702). 177853'! Sergeant Roy Victor CUDLIP, Corps of Royal Military (Police. 4th Queen's Own Hussars. 2814476 Sergeant Walter "Ross GRANT, The Seaforth Lieutenant-Colonel R. S. G. SMITH (44724). Highlanders ^Ross-shire IBuffs, The Duke of Captain (temporary) G. K. BIDIE (386204). Albany's). 553824 War Substantive/Sergeant J. STREET. 5334915 Staff Sergeant Joseph George HILLS, Royal 22202630 Trooper C. R. CARTER. Electrical and Mechanical Engineers. 14194104 Trooper J. H. GOODIER. 2702482 Corporal iFrank HOWARTH, Scots Guards. 19040839 Trooper K. GUY. 19042700 ^Lance-corporal Anthony Walter HURST, 21187657 Trooper R. E. PETERS. Royal Corps of Signals. -

ARMY RESERVE ARMY Group A
MINISTRY OF DEFENCE ARMY RESERVE ARMY Group A Major C. D. QUINCEY 30049957 resigns commission 11 June 2017 APPOINTMENTS INFANTRY The Reverend Father M. P. D. FAVA 547430 is appointed Honorary SCOTTISH DIVISION Chaplain to The QUEEN 5 July 2017 in succession to The Venerable P. A. EAGLES 539182 tenure expired REGULAR ARMY Intermediate Regular Commissions COMMANDS AND STAFF Captain I. K. WALKER The Royal Regiment of Scotland 30028065 REGULAR ARMY from Short Service Commission 3 November 2016 to be Captain with seniority 17 June 2014 (Belated Entry) General Sir Adrian BRADSHAW KCB OBE 508707 retires 12 August 2017 QUEEN’S DIVISION Brigadier J. I. S. STEVENSON MBE 512688 retires 12 August 2017 REGULAR ARMY Colonel A. K. ROBINSON OBE 527755 retires 29 July 2017 Intermediate Regular Commissions (Late Entry) ARMY RESERVE Warrant Officer Class 1 Neil Simon REEDER Royal Anglian Regiment 25028996 to be Captain 12 June 2017 Brigadier C. M. ABRAHAM OBE 513289 from Regular Army Reserve of Officers 19 May 2017 and is granted the substantive rank of LIGHT DIVISION Brigadier with seniority 30 June 2013 ARMY RESERVE ROYAL REGIMENT OF ARTILLERY Group A REGULAR ARMY Captain S. LONGMAN The Rifles 24811566 retires 1 April 2016 (Belated Entry) Intermediate Regular Commissions (Late Entry) Second Lieutenant A. J. BANFIELD The Rifles 30122252 to be Warrant Officer Class 1 Steven MCDONOGH 25045124 to be Captain Lieutenant 9 November 2013 (Belated Entry) 2 June 2017 THE BRIGADE OF GURKHAS CORPS OF ROYAL ENGINEERS REGULAR ARMY REGULAR ARMY Intermediate Regular Commissions (Late Entry) Intermediate Regular Commissions (Late Entry) Captain Ranjankumar BADGAMI Royal Gurkha Rifles 21168496 Warrant Officer Class 1 Mark Sean WILLIAMS 25028849 to be from Short Service Commission (Late Entry) 3 November 2016 to be Captain 12 May 2017 Captain with seniority 1 July 2013 (Belated Entry) ARMY RESERVE ARMY AIR CORPS Group A REGULAR ARMY Second Lieutenant K. -

Gurkhas: Terms and Conditions of Service
Gurkhas: Terms and Conditions of Service Standard Note: SN/IA/4671 Last updated: 12 June 2009 Author: Claire Taylor Section International Affairs and Defence Section The Terms and Conditions of Service of the British Army’s Brigade of Gurkhas were originally set down in accordance with the Tripartite Agreement of 1947 between the UK, India and Nepal. The agreement provided commonality with respect to key Service conditions such as pay and pensions, irrespective of whether Gurkhas were enlisted in the British or Indian Armies. Over the last few years various changes to Gurkha terms and conditions of service have been made in order to bring them more closely into line with their counterparts in the British Army. In September 2004 the decision to grant Gurkhas indefinite leave to remain in the UK upon completion of four years of service and the opportunity to eventually apply for British citizenship was announced by the Government. Changes to the Married Accompanied Service Allowance were also made in August 2005. In addition the MOD also announced in January 2005 that it would undertake a comprehensive review of Gurkha terms and conditions of service. The conclusions and recommendations of that review were published in March 2007. This note provides a brief history of the Gurkhas and the basic obligations for terms and conditions of service which were initially set down under the Tripartite Agreement. It examines the subsequent changes to those terms and conditions of service, including the wide-ranging recommendations of the MOD’s review. Further detailed information on the recent changes to immigration and citizenship rules and pension rights relating to Gurkhas following the March 2007 review is available in the following Library Standard Notes: SN/HA/4399, Immigration: discharged members of the Armed Forces, 11 June 2009 SN/BT/4375, Gurkha Pensions, 12 June 2009 This information is provided to Members of Parliament in support of their parliamentary duties and is not intended to address the specific circumstances of any particular individual. -

The Kukri 2008
THE KUKRI 2008 The Kukri U B I Q U E NUMBER 60 The Journal of The Brigade of Gurkhas 2008 Design: HQLF(U) Design Studio © Crown Copyright Job Reference Number DS 14982 The Kukri - The Journal of The Brigade of Gurkhas The Kukri NUMBER 60 December 2008 (All rights reserved) Headquarters Brigade of Gurkhas Airfield Camp, Netheravon SP4 9SF United Kingdom The Journal of The Brigade of Gurkhas 2008 U B I Q U E Front Cover Queen’s Gurkha Orderly Officers Capt Khusiman Gurung RGR and Capt Sovitbahadur Hamal Thakuri QOGLR 1 The Kukri - The Journal of The Brigade of Gurkhas The Kukri - The Journal of The Brigade of Gurkhas Contents Number 60 December 2008 Editorial ……………………………………………………………………………………………………… 6 Report to the Right Honourable Doctor Ram Baran Yadav, President of the Federal Democratic Republic of Nepal …………………………………………………………… 8 Honours and Awards ……………………………………………………………………………………… 11 Operations 1 RGR Commanding Officer’s Haul-Down Report ……………………………………………………………… 13 Air Operations with Regional Battle Group (South) on Op HERRICK 7 ……………………………… 18 Under the Influence? Thoughts on Influence at Platoon Level from Op HERRICK 7 …………………… 20 2 RGR Operations in Afghanistan - The First Three Months …………………………………………………… 22 Op HERRICK 9 – 2 RGR Battle Group (North West): Influence………………………………………… 31 Op KAPCHA BAZ ……………………………………………………………………………………… 37 Op GALLIPOLI STRIKE 1 ………………………………………………………………………………… 37 Raid North of Patrol Base WOQAB …………………………………………………………………… 38 QGE ……………………………………………………………………………………………………… 42 QGS Stafford-based Gurkha Signallers -

An Investigation Into the Gurkhas' Position in The
THE WAY OF THE GURKHA: AN INVESTIGATION INTO THE GURKHAS’ POSITION IN THE BRITISH ARMY Thesis submitted to Kingston University in partial fulfilment of the requirement for the degree of Doctor of Philosophy Mulibir Rai Faculty of Arts and Social Science Kingston University 2018 1 2 CONTENTS The thesis contains: Documentary: The Way of the Gurkha Script/Director/Presenter/Editor/Cinematographer: Mulibir Rai Cast: Mulibir Rai, Karan Rai, Sarbada Rai, Deshu Rai, Shanta Maya Limbu, Kesharbahadur Rai, Yamkumar Rai, Dipendra Rai, Rastrakumar Rai, Bambahadur Thapa, Tiloksing Rai, Lt Col JNB Birch, Maj R Anderson, Gajendra K.C, Sophy Rai, Chandra Subba Gurung, Lt Col (retired) J. P. Cross, Major (retired) Tikendradal Dewan, Gyanraj Rai, Padam Gurung, D.B. Rai, Recruit intake 2012. Genre: Documentary Run time: 1:33:26 Medium: High definition Synopsis – The documentary is divided into two parts. In the first part, the researcher, in 2012 returned to his village of Chautara in Eastern Nepal where he was born, raised and educated for the first time in 13 years. He found many changes in the village - mainly in transport and information technology, but no improvement in the standard of English teaching which nowadays, unlike in the past, is one of the necessities required for joining the British Army. Hence, the hillboys pay a significant amount of money to the training academies in the cities to improve their English. In the end, only a few out of thousands of candidates achieve success. They fly to the UK and receive nine months training at Catterick Garrison Training Centre before joining their respective regiments as fully-fledged Gurkha soldiers. -
Heritage Manual
A-DH-200-000/AG-000 CHAPTER 8 ALLIANCES, AFFILIATIONS AND PARTNERSHIPS CANADIAN CUSTOMS 1. Officially-sanctioned links can be established to foster continuous fraternal connections between military organizations beyond the close, professional relationships which are always encouraged. 2. Three types of official links are maintained by the Canadian Armed Forces (CAF): a. an alliance – between Canadian and Commonwealth units or branches/corps; b. an affiliation – between two Canadian units; and c. a partnership – an informal bond of friendship (partnership) between a Canadian unit and a unit from an allied country, such as a member of the North Atlantic Treaty Organization (NATO). Partnerships include "jumelages" (the twinning of Canadian and French units), "partnerschafts" (the twinning of Canadian and German units), and similar bonds. GUIDELINES 3. A Canadian branch or corps is one of the CAF personnel branches or corps described in Chapter 1. Its equivalent in the armed forces of another member of the Commonwealth may be titled as a department, corps or branch. 4. A Canadian unit is a commissioned ship, regiment, flying squadron, or equivalent. Sub-units shall not be authorized alliances, affiliations or partnerships. 5. Since official links create a social obligation to welcome members into each other's "families", they should only be requested if the organizations concerned are prepared to maintain contact over time. 6. In general, requests to forge these links may be made when: a. close ties and personal relationships have developed between units through combined participation in operations or training, regular exchange of personnel on exercises, special meets, parades, competitions, etc.; b. -

5292 Supplement to the London Gazette, 24 October, 1950
5292 SUPPLEMENT TO THE LONDON GAZETTE, 24 OCTOBER, 1950 The War Office, 24th October, 1950. Capt. (temp.) M. H. WILTON (124364). Lt. J. A. WILKINSON (384399). The KING has been graciously pleased to approve 18013278 A/W.O. I JAMIN Bin MARSON (L.E.P.). the following awards in recognition of gallant and 18013296 A/W.O. II ABASS Bin KHALID (L.E.P.). distinguished services in Malaya during the period 828958 Sjt. C. SAUNDERS. 1st January to 30th June, 1950: — 21002798 A/Sjt. B. E. HODSON. (To be dated 18th September, 1950.) 14460023 A/Bdr. D. A. TAYLOR. 19037372 Gnr. R. J. MENEAR. The Distinguished Service Order. Lieutenant-Colonel (temporary) Robert George Victor CORPS OF ROYAL ENGINEERS. FITZ-GEORGE-BALFOUR, C.B.E., M.C. (5-328'8), Cold- Lt.-Col. M. CHAMPION-JONES (30534). stream Guards. Lt.-Col. (temp.) C. R. JANVRIN, M.B.E. (100475). Lieutenant-Colonel (now Colonel (temporary)) Cyril Maj. (temp.) R. F. N. ANDERSON, M.C. (95071). Carew GRAHAM, O.B.E. (391327), 10th Gurkha Maj. (temp.) R. J. HEWITT (237317). Rifles, The Brigade of Gurkhas. Maj. (temp.) C. J. OLIN (294148). Lieutenant-Colonel John Stratford SANDERSON, O.B.E. Maj. (temp.) K. M. ROBERTSON (73061). (40179), Scots Guards. Maj. (temp.) P. V. H. SWAN (77569). Capt. R. D. H. BLIGHT (265565). Bar to The Military Cross. Capt. A. N. DANIELL (146085). Major (temporary) Angus James Donald MACDONALD, 5494950 W.O. I E. J. HARVEY. M.C. (384999), The Queen's Own Cameron 1931812 A/Sjt. P. T. MAIDMENT. Highlanders. 1872063 Cpl. P. PULFORD. -

The Gurkha Brigade Association @Gurkha Brigade
The Gurkha Brigade Association @Gurkha_Brigade Creative Media Design ADR003298 www.gurkhabde.com/publication Vol 65 No 9: Feb 2014 The magazine for Gurkha Soldiers and their Families Bde Band - MOD(UK) Defence Engagement to Nepal and India 2013-14 G200E - Update 1 RGR - JLC 2013 Vol 65 No. 9 - February 2014 Editorial Staff Contents Editor: Mrs Janette Patterson Bde Band 2 - 3 Assistant Editor: Cpl Rakam Thamshuhang GSPS G200E 4 - 5 Telephone: 01980 618012 (94344 8012) Fax: 01980 618938 (94344 8938) 1 RGR 6 - 7 Email: [email protected] GWT. 8 MOD Users: [email protected] Gurkha Museum 8 Please send your articles together with good quality Nepali Page 9 photographs (300 dpi), through your unit’s Parbate Rep, to: Photo News 10 - 11 The Editor, Parbate Office, HQBG, Trenchard Lines, Upavon, Pewsey, Wiltshire SN9 6BE* 2 RGR 12 - 15 QGE 16 Parbate is published every month by kind permission of HQBG. It is not an official publication and the views expressed, unless specifically stated otherwise, do not reflect QGS 16 - 18 MOD or Army policy and are the personal views of the author. No part of this publication may be reproduced without the permission of the Editorial Staff. No responsibility for the QOGLR 19 quality of goods or services advertised in this magazine can be accepted by the Editorial Staff or Publishers and advertisements are accepted on the express condition that they in no GSPS 20 way contravene the provisions of the Trades Descriptions Act 1968 nor any other prevailing Consumer Legislation. The Editorial Staff and Publishers cannot accept responsibility for the result of errors or omissions in articles or advertisements. -

History of the Gurkha Staff and Personnel Support
History of the Gurkha Staff and Personnel Support On the 30th June 2011 at a parade at Sir John Moore Barracks, Shorncliffe, the clerks of the Brigade of Gurkhas exchanged their Royal Gurkha Rifle’s cap badge for the badge of the newly formed Gurkha Staff and Personnel Support Company (GSPS Coy). This parade was held in the presence of the Colonel Commandant Brigade of Gurkhas, General Sir David Richards GCB CBE DSO ADC Gen. The then Director Staff and Personnel Support (Army), Brigadier Nicky Moffat Late AGC (SPS) assumed the inaugural appointment of Colonel GSPS. The formation of the GSPS Coy was the result of a major review in 2007 which sought to harmonize the terms and conditions of service of Gurkhas with the rest of The British Army. In July 2009, the Executive Committee of the Army Board (ECAB) endorsed the broad principles on the future management of Gurkha military clerks. This included a recommendation that Gurkha military clerks should be re-organised along the lines of the Combat Human Resource Specialists in the wider Army, which would give increased career opportunities for Gurkha clerks. Within each Gurkha battalion there evolved a clerical establishment, initially manned by Indian civilians known as writers and later a mix of Indian and Gurkha military clerks, the latter having been enlisted as line boys.These were the sons of Gurkhas who were born and brought up within the regimental lines in India. They were usually better educated than those Gurkhas recruited from the hills of Nepal and were enlisted as signallers, bandsmen and clerks. -

Gurkha Soldiers As an Intercultural Moment on the European Battlefields of the Great War
City University of New York (CUNY) CUNY Academic Works Publications and Research Queensborough Community College 2015 Gurkha Soldiers as an Intercultural Moment on the European Battlefields of the Great War Frank Jacob CUNY Queensborough Community College How does access to this work benefit ou?y Let us know! More information about this work at: https://academicworks.cuny.edu/qb_pubs/15 Discover additional works at: https://academicworks.cuny.edu This work is made publicly available by the City University of New York (CUNY). Contact: [email protected] Gurkha Soldiers as an Intercultural Moment on the European Battlefields of the Great War Frank JACOB ! The centennial of the First World War in 2014 created a high impact for research of the events between 1914 and 1918.i However, the perspective remained a mainly European one, as it can be seen by having a look in the Cambridge History of the First World Warii , which covers mainly the European aspects of the Great War. Despite this partially still existing Euro-centrism with regard to the events of the “seminal catastrophe of the twentieth century,“iii research on colonial spheres and the use of colonial troopsiv in the international campaigns are especially important to show the transnational impact of the events during the war years. The British Empire and its multiethnic colonial sphere had created many different colonial elite troops, whose members were recruited in Africav , the Punjabvi , and especially Nepalvii . The last named country provided countless generations of young men to fight and die for the sake of the British Empire, and military historians as well as those who served as officers in the British army know that the so-called Gurkhas have been an elite troop inside the British Indian Army for more than one and a half centuries. -
2Nd Battalion 26 Army Cadets 29 1St Battalion 34 a Concise Record of a Short Visit to Washington, U.S.A
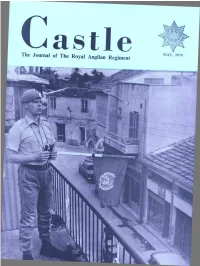
5/70-1 Printed in Great Britain SUPPLEMENT No. 1—PAGE ONE SUPPLEMENT No. 1-PAGE TWO Printed in Great Britain SUPPLEMENT N o. 1- P A G E THREE Printed in Great Britain 1850 OFFICER OF THE 11th HUSSARS The 11th ( Prince Albert s ow n) provided the escort to the Prince Consort when he landed at Dover and also took part in the famous charge of the Light Brigade. Traditionally, too, the Colchester Permanent Benefit Building Society have a fine record (also since Albert's day) of providing a safe escort for your savings-and just think of the 'charges' you can offset with the interest you make in the Colchester Permanent-write today to 11 Sir Isaacs Walk, Colchester, Essex. F. A. STONE & SONS TAILORS MAKERS OF MILITARY GARMENTS AND MUFTI OF ALL TYPES SINCE 1874 Known to military personnel o f many units throughout the country SUBSCRIPTION TERMS AVAILABLE LONDON NORWICH 2 Savile Row, W.1. PRINCE OF WALES ROAD GT. YARMOUTH Phone: REG 1464 Phone : 25296 By Appointment ii Barber-Greene Greetings and Best Wishes to all who serve with the Royal Anglian Regiment Barber-Greene England Limited Bury St. Edmunds Suffolk Tel. 3411/7 iii CONWAY WILLIAMS THE MAYFAIR TAILOR 48 BROOK STREET, MAYFAIR, LONDON, W.1 (Opposite Claridges Hotel) AND 39 LONDON ROAD, CAMBERLEY Morning and Evening Wear, Court and Military Dress for all occasions. Hunting, Sports and Lounge Kits All Cloths cut by expert West End Cutters and made exclusively by hand in our Mayfair workshops by the Best English Tailors Regimental Tailors to The Royal Anglian Regiment Telephones : Telegrams : 01-629 0945—Camberley 0276-4098. -

A Forgotten Force: the Gurkhas and the Partition of India
A Forgotten Force: the Gurkhas and the Partition of India. Dissertation History MA. Supervisor: Dr Talat Ahmed. Exam Number: B069448. Word Count: 11,884. B069448 1 ACKNOWLEDGEMENTS Firstly, I would like to thank my supervisor Dr. Talat Ahmed, for her advice and continued support over the past year. I am also extremely grateful to all those at the Gurkha Museum who assisted in locating essential documents and whose interest in the topic was very encouraging. Finally, I would like to recognise the patience and support of friends and family. B069448 2 CONTENTS A Forgotten Force: the Gurkhas and the Partition of India. ACKNOWLEDGEMENTS…………………………………………………………………………………………………2 CONTENTS……………………………………………………………………………………………………………………3 ABBREVIATIONS…………………………………………………………………………………………………………..4 INTRODUCTION……………………………………………………………………………………………………………5 METHODOLOGY………………………………………………………………………………………………………….14 (1)SILENCE AS REVEALING……………………………………………………………………………………………19 (2)IMAGINED COMMUNITIES?......................................................................................27 (3)A FORGOTTEN FORCE……………………………………………………………………………………………..37 CONCLUSION………………………………………………………………………………………………………………46 BIBLIOGRAPHY……………………………………………………………………………………………………………50 B069448 3 ABBREVIATIONS G/R – Gurkha Rifles. The Gurkhas/Brigade - The Brigade of Gurkhas. B069448 4 INTRODUCTION Upon the transfer of power from Britain, on 15th August 1947, Indian was partitioned into two new states, India and Pakistan. The two countries celebrated independence separately; Pakistan on 14th and India