Table of Contents
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-
Spinraza™ (Nusinersen)
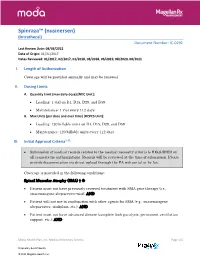
Spinraza™ (nusinersen) (Intrathecal) Document Number: IC-0291 Last Review Date: 08/03/2021 Date of Origin: 01/31/2017 Dates Reviewed: 01/2017, 02/2017, 01/2018, 08/2018, 06/2019, 08/2020, 08/2021 I. Length of Authorization Coverage will be provided annually and may be renewed. II. Dosing Limits A. Quantity Limit (max daily dose) [NDC Unit]: • Loading: 1 vial on D1, D15, D29, and D59 • Maintenance: 1 vial every 112 days B. Max Units (per dose and over time) [HCPCS Unit]: • Loading: 120 billable units on D1, D15, D29, and D59 • Maintenance: 120 billable units every 112 days III. Initial Approval Criteria1-12 • Submission of medical records related to the medical necessity criteria is REQUIRED on all requests for authorizations. Records will be reviewed at the time of submission. Please provide documentation via direct upload through the PA web portal or by fax. Coverage is provided in the following conditions: Spinal Muscular Atrophy (SMA) † Ф • Patient must not have previously received treatment with SMA gene therapy (i.e., onasemnogene abeparvovec-xioi); AND • Patient will not use in combination with other agents for SMA (e.g., onasemnogene abeparvovec, risdiplam, etc.); AND • Patient must not have advanced disease (complete limb paralysis, permanent ventilation support, etc.); AND Moda Health Plan, Inc. Medical Necessity Criteria Page 1/5 Proprietary & Confidential © 2021 Magellan Health, Inc. • Patient must have the following laboratory tests at baseline and prior to each administration*: platelet count, prothrombin time; activated -

Nonpharmacological Treatment of Rhinoconjunctivitis and Rhinosinusitis
Journal of Allergy Nonpharmacological Treatment of Rhinoconjunctivitis and Rhinosinusitis Guest Editors: Ralph Mösges, Carlos E. Baena-Cagnani, and Desiderio Passali Nonpharmacological Treatment of Rhinoconjunctivitis and Rhinosinusitis Journal of Allergy Nonpharmacological Treatment of Rhinoconjunctivitis and Rhinosinusitis Guest Editors: Ralph Mosges,¨ Carlos E. Baena-Cagnani, and Desiderio Passali Copyright © 2014 Hindawi Publishing Corporation. All rights reserved. This is a special issue published in “Journal of Allergy.” All articles are open access articles distributed under the Creative Commons At- tribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited. Editorial Board William E. Berger, USA Alan P. Knutsen, USA Fabienne Ranc, France Kurt Blaser, Switzerland Marek L. Kowalski, Poland Anuradha Ray, USA Eugene R. Bleecker, USA Ting Fan Leung, Hong Kong Harald Renz, Germany JandeMonchy,TheNetherlands Clare M Lloyd, UK Nima Rezaei, Iran Frank Hoebers, The Netherlands Redwan Moqbel, Canada Robert P. Schleimer, USA StephenT.Holgate,UK Desiderio Passali, Italy Massimo Triggiani, Italy Sebastian L. Johnston, UK Stephen P. Peters, USA Hugo Van Bever, Singapore Young J. Juhn, USA David G. Proud, Canada Garry Walsh, United Kingdom Contents Nonpharmacological Treatment of Rhinoconjunctivitis and Rhinosinusitis,RalphMosges,¨ Carlos E. Baena-Cagnani, and Desiderio Passali Volume 2014, Article ID 416236, 2 pages Clinical Efficacy of a Spray Containing Hyaluronic Acid and Dexpanthenol after Surgery in the Nasal Cavity (Septoplasty, Simple Ethmoid Sinus Surgery, and Turbinate Surgery), Ina Gouteva, Kija Shah-Hosseini, and Peter Meiser Volume 2014, Article ID 635490, 10 pages The Effectiveness of Acupuncture Compared to Loratadine in Patients Allergic to House Dust ,Mites Bettina Hauswald, Christina Dill, Jurgen¨ Boxberger, Eberhard Kuhlisch, Thomas Zahnert, and Yury M. -

Xolair/Omalizumab
Therapeutic/Humanized Antibodies ELISA Kits ‘Humanized antibodies” are ‘Animal Antibodies’ that have been modified by recombinant DNA-technology to reduce the overall content of the animal- portion of immunoglobulin so as to increase acceptance by humans or minimize ‘rejection’. By analogy, if the hands of a mouse is actually responsible for grabbing things then ‘humanized-mouse’ will only contain the ‘mouse hands’ and the rest of the body will be human. Since the size of the IgGs is similar in mouse and human, the size of the native mouse IgG and the ‘humanized IgG’ does not significantly change. Antigen recognition property of an antibody actually resides in small portion of the IgG molecule called the ‘antigen binding site or Fab’. Therefore, humanized antibodies contain the minimal portion from the Fab or the epitopes necessary for antigen binding. The process of "humanization of antibodies" is usually applied to animal (mouse) derived monoclonal antibodies for therapeutic use in humans (for example, antibodies developed as anti-cancer drugs). Xolair (Anti-IgE) is an example of humanized IgG. The portion of the mouse IgG that remains in the ‘humanized IgG’ may be recognized as foreign by humans and may result into the generation of “Human Anti-Drug Antibodies (HADA). The presence of anti-Drug antibody (e.g., Human Anti-Rituximab IgG) that may limit the long-term usage the humanized antibody (Rituximab). Not all monoclonal antibodies designed for human therapeutic use need be humanized since many therapies are short-term. The International Nonproprietary Names of humanized antibodies end in “-zumab”, as in “omalizumab”. Humanized antibodies are distinct from chimeric or fusion antibodies. -

2017 ANNUAL REPORT | Translating SCIENCE • Transforming LIVES OUR COMMITMENT Make Every Day Count at PTC, Patients Are at the Center of Everything We Do
20 YEARS OF COMMITMENT 2017 ANNUAL REPORT | Translating SCIENCE • Transforming LIVES OUR COMMITMENT Make every day count At PTC, patients are at the center of everything we do. We have the opportunity to support patients and families living with rare disorders through their journey. We know that every day matters and we are committed to making a difference. OUR SCIENCE Our scientists are finding new ways to regulate biology to control disease We have several scientific research platforms focused on modulating protein expression within the cell that we believe have the potential to address many rare genetic disorders. OUR PEOPLE Care for each other, our community, and for the needs of our patients At PTC, we are looking at drug discovery and development in a whole new light, bringing new technologies and approaches to developing medicines for patients living with rare disorders and cancer. We strive every day to be better than we were the day before. At PTC Therapeutics, it is our mission to provide access to best-in-class treatments for patients who have an unmet need. We are a science-led, global biopharmaceutical company focused on the discovery, development and commercialization of clinically-differentiated medicines that provide benefits to patients with rare disorders. Founded 20 years ago, PTC Therapeutics has successfully launched two rare disorder products and has a global commercial footprint. This success is the foundation that drives investment in a robust pipeline of transformative medicines and our mission to provide access to best-in-class treatments for patients who have an unmet medical need. As we celebrate our 20th year of bringing innovative therapies to patients affected by rare disorders, we reflect on our unwavering commitment to our patients, our science and our employees. -

September 11, 2018 DUR Minutes
Maine Department of Health and Human Services PAUL R. LEPAGE MaineCare Services BETHANY L. HAMM GOVERNOR Pharmacy Unit ACTING COMMISSIONER 11 State House Station Augusta, Maine 04333-0011 TO: Maine Drug Utilization Review Board DATE: 9/14/2018 RE: Maine DUR Board Meeting minutes from September 11, 2018 ATTENDANCE PRESENT ABSENT EXCUSED Linda Glass, MD X Lisa Wendler, Pharm. D., Clinical Pharmacy Specialist, X Maine Medical CTR Mike Antoniello, MD X Kathleen Polonchek, MD X Kenneth McCall, PharmD X Steve Diaz, MD X Erin Ackley, PharmD. X Corinn Martineau, PharmD. X Non –Voting Mike Ouellette, R.Ph., Change Healthcare X Jeffery Barkin, MD, Change Healthcare X Christopher Pezzullo, State Health Officer DHHS, DO X Jill Kingsbury, MaineCare Pharmacy Director X Guests of the Board: Ed Bosshart, PharmD, Jeff Caulfield, Lead Epidemiologist for Viral Infections from CDC: Discussed HCV treatment. CALL TO ORDER: 5:30PM Jill Kingsbury called the meeting to order at 5:30 PM. PUBLIC COMMENTS Robert Mead from Pfizer: Highlighted the attributes of Retacrit. Jane Guo from Otsuka: Highlighted the attributes of Jynarque. OLD BUSINESS DUR MINUTES The June DUR meeting minutes were accepted as written. MAINECARE UPDATE No update at this time. NEW BUSINESS INTRODUCTION: USE OF CHRONIC TRIPTANS The use of triptans has become standard of care for the treatment of acute migraine headaches, given their effectiveness, safety and tolerability. However, like many medications used to treat migraine, overuse renders them less effective. Additionally, rebound headaches from triptan overuse is common. For patients who experience frequent headaches, or whose headaches are long lasting or chronic, use of headache prophylactic medications are recommended by several medical associations, including the American Headache Society and the American Academy of Neurology. -

(CD-P-PH/PHO) Report Classification/Justifica
COMMITTEE OF EXPERTS ON THE CLASSIFICATION OF MEDICINES AS REGARDS THEIR SUPPLY (CD-P-PH/PHO) Report classification/justification of medicines belonging to the ATC group R01 (Nasal preparations) Table of Contents Page INTRODUCTION 5 DISCLAIMER 7 GLOSSARY OF TERMS USED IN THIS DOCUMENT 8 ACTIVE SUBSTANCES Cyclopentamine (ATC: R01AA02) 10 Ephedrine (ATC: R01AA03) 11 Phenylephrine (ATC: R01AA04) 14 Oxymetazoline (ATC: R01AA05) 16 Tetryzoline (ATC: R01AA06) 19 Xylometazoline (ATC: R01AA07) 20 Naphazoline (ATC: R01AA08) 23 Tramazoline (ATC: R01AA09) 26 Metizoline (ATC: R01AA10) 29 Tuaminoheptane (ATC: R01AA11) 30 Fenoxazoline (ATC: R01AA12) 31 Tymazoline (ATC: R01AA13) 32 Epinephrine (ATC: R01AA14) 33 Indanazoline (ATC: R01AA15) 34 Phenylephrine (ATC: R01AB01) 35 Naphazoline (ATC: R01AB02) 37 Tetryzoline (ATC: R01AB03) 39 Ephedrine (ATC: R01AB05) 40 Xylometazoline (ATC: R01AB06) 41 Oxymetazoline (ATC: R01AB07) 45 Tuaminoheptane (ATC: R01AB08) 46 Cromoglicic Acid (ATC: R01AC01) 49 2 Levocabastine (ATC: R01AC02) 51 Azelastine (ATC: R01AC03) 53 Antazoline (ATC: R01AC04) 56 Spaglumic Acid (ATC: R01AC05) 57 Thonzylamine (ATC: R01AC06) 58 Nedocromil (ATC: R01AC07) 59 Olopatadine (ATC: R01AC08) 60 Cromoglicic Acid, Combinations (ATC: R01AC51) 61 Beclometasone (ATC: R01AD01) 62 Prednisolone (ATC: R01AD02) 66 Dexamethasone (ATC: R01AD03) 67 Flunisolide (ATC: R01AD04) 68 Budesonide (ATC: R01AD05) 69 Betamethasone (ATC: R01AD06) 72 Tixocortol (ATC: R01AD07) 73 Fluticasone (ATC: R01AD08) 74 Mometasone (ATC: R01AD09) 78 Triamcinolone (ATC: R01AD11) 82 -

DRUGS REQUIRING PRIOR AUTHORIZATION in the MEDICAL BENEFIT Page 1
Effective Date: 08/01/2021 DRUGS REQUIRING PRIOR AUTHORIZATION IN THE MEDICAL BENEFIT Page 1 Therapeutic Category Drug Class Trade Name Generic Name HCPCS Procedure Code HCPCS Procedure Code Description Anti-infectives Antiretrovirals, HIV CABENUVA cabotegravir-rilpivirine C9077 Injection, cabotegravir and rilpivirine, 2mg/3mg Antithrombotic Agents von Willebrand Factor-Directed Antibody CABLIVI caplacizumab-yhdp C9047 Injection, caplacizumab-yhdp, 1 mg Cardiology Antilipemic EVKEEZA evinacumab-dgnb C9079 Injection, evinacumab-dgnb, 5 mg Cardiology Hemostatic Agent BERINERT c1 esterase J0597 Injection, C1 esterase inhibitor (human), Berinert, 10 units Cardiology Hemostatic Agent CINRYZE c1 esterase J0598 Injection, C1 esterase inhibitor (human), Cinryze, 10 units Cardiology Hemostatic Agent FIRAZYR icatibant J1744 Injection, icatibant, 1 mg Cardiology Hemostatic Agent HAEGARDA c1 esterase J0599 Injection, C1 esterase inhibitor (human), (Haegarda), 10 units Cardiology Hemostatic Agent ICATIBANT (generic) icatibant J1744 Injection, icatibant, 1 mg Cardiology Hemostatic Agent KALBITOR ecallantide J1290 Injection, ecallantide, 1 mg Cardiology Hemostatic Agent RUCONEST c1 esterase J0596 Injection, C1 esterase inhibitor (recombinant), Ruconest, 10 units Injection, lanadelumab-flyo, 1 mg (code may be used for Medicare when drug administered under Cardiology Hemostatic Agent TAKHZYRO lanadelumab-flyo J0593 direct supervision of a physician, not for use when drug is self-administered) Cardiology Pulmonary Arterial Hypertension EPOPROSTENOL (generic) -

RECENT MAJOR CHANGES------ Age
HIGHLIGHTS OF PRESCRIBING INFORMATION These highlights do not include all the information needed to use ---------------------DOSAGE FORMS AND STRENGTHS--------------------- CRYSVITA safely and effectively. See full prescribing information Injection: 10 mg/mL, 20 mg/mL, or 30 mg/mL in a single-dose vial (3) for CRYSVITA. -------------------------------CONTRAINDICATIONS----------------------------- ® CRYSVITA (burosumab-twza) injection, for subcutaneous use • With oral phosphate and/or active vitamin D analogs. (4) Initial U.S. Approval: 2018 • When serum phosphorus is within or above the normal range for -------------------------RECENT MAJOR CHANGES----------------- age. (4) Indications and Usage (1) 6/2020 • In patients with severe renal impairment or end stage renal Dosage and Administration, disease. (4) Tumor-induced Osteomalacia (2.4) 6/2020 ------------------------WARNINGS AND PRECAUTIONS---------------------- Dosage and Administration, 25-Hydroxy Vitamin D • Hypersensitivity: Discontinue CRYSVITA if serious hypersensitivity Supplementation (2.7) 9/2019 reactions occur and initiate appropriate medical treatment. (5.1) • Hyperphosphatemia and Risk of Nephrocalcinosis: For patients -----------------------------INDICATIONS AND USAGE------------------------- already taking CRYSVITA, dose interruption and/or dose reduction CRYSIVTA is a fibroblast growth factor 23 (FGF23) blocking antibody may be required based on a patient’s serum phosphorus levels. indicated for: (5.2, 6.1) • The treatment of X-linked hypophosphatemia (XLH) in adult and • Injection Site Reactions: Administration of CRYSVITA may result in pediatric patients 6 months of age and older. (1.1) local injection site reactions. Discontinue CRYSVITA if severe • The treatment of FGF23-related hypophosphatemia in tumor- injection site reactions occur and administer appropriate medical induced osteomalacia (TIO) associated with phosphaturic treatment. (5.3, 6.1) mesenchymal tumors that cannot be curatively resected or localized in adult and pediatric patients 2 years of age and older. -

Duchenne Muscular Dystrophy (DMD) Agents
Therapeutic Class Overview Duchenne muscular dystrophy (DMD) Agents INTRODUCTION • Duchenne muscular dystrophy (DMD) is 1 of 4 conditions known as dystrophinopathies, which are inherited, X-linked myopathic disorders due to a defect in the dystrophin gene that results in the primary pathologic process of muscle fiber degradation. The hallmark symptom is progressive weakness (Darras 2018[a], Darras 2018[b], Muscular Dystrophy Association [MDA] 2019). The other 3 conditions include: Becker muscular dystrophy (BMD), which is a mild form of DMD; an intermediate presentation between BMD and DMD; and DMD-associated dilated cardiomyopathy, which has little or no clinical ○ skeletal or muscle disease (MDA 2019). • DMD symptom onset is in early childhood, usually between the ages of 2 and 3 years old. The proximal muscles are affected first, followed by the distal limb muscles. Generally, the lower external muscles will be affected before the upper. The affected child may have difficulties jumping, walking, and running (MDA 2019). • The prevalence of DMD ranges from 1 to 2 per 10,000 live male births; female-manifesting carriers are rarer, but can present with a range of symptoms that vary in their severities (Birnkrant et al 2018, Darras 2018[a], Emflaza Food and Drug Administration [FDA] Medical Review 2017). • The clinical course and lifespan of patients with DMD is relatively short. Individuals are usually confined to a wheelchair by age 13, and many die in their late teens or twenties from respiratory insufficiency or cardiomyopathy. Although survival until adulthood is more common now, very few patients survive past the 3rd decade (Darras 2018[a]). -

(Human) ELISA Kit Rev 06/20 (Catalog # E 4381 - 100, 100 Assays, Store at 4°C) I
FOR RESEARCH USE ONLY! TM BioSim Omalizumab (Human) ELISA Kit rev 06/20 (Catalog # E4381-100, 100 assays, Store at 4°C) I. Introduction: Omalizumab is a recombinant DNA-derived humanized IgG1k monoclonal antibody that selectively binds to human immunoglobulin E (IgE). Omalizumab inhibits the binding of IgE to the high-affinity IgE receptor (FceRI) on the surface of mast cells and basophils. Reduction in surface-bound IgE on FceRI-bearing cells limits the degree of release of mediators of the allergic response. Omalizumab is used to treat severe, persistent asthma. BioSimTM Omalizumab ELISA kit has been developed for specific quantification of Omalizumab concentration in human serum or plasma with high sensitivity and reproducibility. II. Application: This ELISA kit is used for in vitro quantitative determination of Omalizumab Detection Range: 10 - 1000 ng/ml Sensitivity: 10 ng/ml Assay Precision: Intra-Assay: CV < 15%; Inter-Assay: CV < 15% (CV (%) = SD/mean X 100) Recovery rate: 85 – 115% with normal human serum samples with known concentrations Cross Reactivity: There is no cross reaction with native serum immunoglobulins and tested monoclonal antibodies such as infliximab (Remicade®), adalimumab (Humira®), etanercept (Enbrel®), bevacizumab, trastuzumab III. Sample Type: Human serum and plasma IV. Kit Contents: Components E4381-100 Part No. Micro ELISA Plate 1 plate E4381-100-1 Omalizumab Standards (S1 – S7) 1 ml X 7 E4381-100-2.x Assay Buffer 50 ml E4381-100-3 HRP-conjugate Probe 12 ml E4381-100-4 TMB substrate (Avoid light) 12 ml E4381-100-5 Stop Solution 12 ml E4381-100-6 Wash buffer (20X) 50 ml E4381-100-7 Plate sealers 2 E4381-100-8 V. -

Vyondys 53™ (Golodirsen)
UnitedHealthcare® Commercial Medical Benefit Drug Policy Vyondys 53™ (Golodirsen) Policy Number: 2021D0088C Effective Date: April 1, 2021 Instructions for Use Table of Contents Page Related Commercial Policy Coverage Rationale ....................................................................... 1 • Provider Administered Drugs – Site of Care Applicable Codes .......................................................................... 2 Background.................................................................................... 2 Community Plan Policy Benefit Considerations .................................................................. 3 • Vyondys 53™ (Golodirsen) Clinical Evidence ........................................................................... 3 U.S. Food and Drug Administration ............................................. 3 References ..................................................................................... 4 Policy History/Revision Information ............................................. 4 Instructions for Use ....................................................................... 4 Coverage Rationale See Benefit Considerations Vyondys 53 (golodirsen) may be covered for the treatment of Duchenne muscular dystrophy (DMD) in patients who meet all of the following criteria: For initial therapy, all of the following: o Diagnosis of Duchenne muscular dystrophy by, or in consultation with, a neurologist with expertise in the diagnosis of DMD; and o Submission of medical records (e.g., chart notes, laboratory -

Keeping up with FDA Drug Approvals: 60 New Drugs in 60 Minutes Elizabeth A
Keeping Up with FDA Drug Approvals: 60 New Drugs in 60 Minutes Elizabeth A. Shlom, PharmD, BCPS Senior Vice President & Director Clinical Pharmacy Program | Acurity, Inc. Privileged and Confidential April 10, 2019 Privileged and Confidential Program Objectives By the end of the presentation, the pharmacist or pharmacy technician participant will be able to: ▪ Identify orphan drugs and first-in-class medications approved by the FDA in 2018. ▪ List five new drugs and their indications. ▪ Identify the place in therapy for three novel monoclonal antibodies. ▪ Discuss at least two new medications that address public health concerns. Dr. Shlom does not have any conflicts of interest in regard to this presentation. Both trade names and generic names will be discussed throughout the presentation Privileged and Confidential 2018 NDA Approvals (NMEs/BLAs) ▪ Lutathera (lutetium Lu 177 dotatate) ▪ Braftovi (encorafenib) ▪ Vizimpro (dacomitinib) ▪ Biktarvy (bictegravir, emtricitabine, ▪ TPOXX (tecovirimat) ▪ Libtayo (cemiplimab-rwic) tenofovir, ▪ Tibsovo (ivosidenib) ▪ Seysara (sarecycline) alafenamide) ▪ Krintafel (tafenoquine) ▪ Nuzyra (omadacycline) ▪ Symdeko (tezacaftor, ivacaftor) ▪ Orilissa (elagolix sodium) ▪ Revcovi (elapegademase-lvir) ▪ Erleada (apalutamide) ▪ Omegaven (fish oil triglycerides) ▪ Tegsedi (inotersen) ▪ Trogarzo (ibalizumab-uiyk) ▪ Mulpleta (lusutrombopag) ▪ Talzenna (talazoparib) ▪ Ilumya (tildrakizumab-asmn) ▪ Poteligeo (mogamulizumab-kpkc) ▪ Xofluza (baloxavir marboxil) ▪ Tavalisse (fostamatinib disodium) ▪ Onpattro (patisiran)