Oregon Medicaid Pharmaceutical Services Prior Authorization Criteria
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Minutes of the CHMP Meeting 14-17 September 2020
13 January 2021 EMA/CHMP/625456/2020 Corr.1 Human Medicines Division Committee for medicinal products for human use (CHMP) Minutes for the meeting on 14-17 September 2020 Chair: Harald Enzmann – Vice-Chair: Bruno Sepodes Disclaimers Some of the information contained in these minutes is considered commercially confidential or sensitive and therefore not disclosed. With regard to intended therapeutic indications or procedure scopes listed against products, it must be noted that these may not reflect the full wording proposed by applicants and may also vary during the course of the review. Additional details on some of these procedures will be published in the CHMP meeting highlights once the procedures are finalised and start of referrals will also be available. Of note, these minutes are a working document primarily designed for CHMP members and the work the Committee undertakes. Note on access to documents Some documents mentioned in the minutes cannot be released at present following a request for access to documents within the framework of Regulation (EC) No 1049/2001 as they are subject to on- going procedures for which a final decision has not yet been adopted. They will become public when adopted or considered public according to the principles stated in the Agency policy on access to documents (EMA/127362/2006). 1 Addition of the list of participants Official address Domenico Scarlattilaan 6 ● 1083 HS Amsterdam ● The Netherlands Address for visits and deliveries Refer to www.ema.europa.eu/how-to-find-us Send us a question Go to www.ema.europa.eu/contact Telephone +31 (0)88 781 6000 An agency of the European Union © European Medicines Agency, 2020. -

AHFS Pharmacologic-Therapeutic Classification System
AHFS Pharmacologic-Therapeutic Classification System Abacavir 48:24 - Mucolytic Agents - 382638 8:18.08.20 - HIV Nucleoside and Nucleotide Reverse Acitretin 84:92 - Skin and Mucous Membrane Agents, Abaloparatide 68:24.08 - Parathyroid Agents - 317036 Aclidinium Abatacept 12:08.08 - Antimuscarinics/Antispasmodics - 313022 92:36 - Disease-modifying Antirheumatic Drugs - Acrivastine 92:20 - Immunomodulatory Agents - 306003 4:08 - Second Generation Antihistamines - 394040 Abciximab 48:04.08 - Second Generation Antihistamines - 394040 20:12.18 - Platelet-aggregation Inhibitors - 395014 Acyclovir Abemaciclib 8:18.32 - Nucleosides and Nucleotides - 381045 10:00 - Antineoplastic Agents - 317058 84:04.06 - Antivirals - 381036 Abiraterone Adalimumab; -adaz 10:00 - Antineoplastic Agents - 311027 92:36 - Disease-modifying Antirheumatic Drugs - AbobotulinumtoxinA 56:92 - GI Drugs, Miscellaneous - 302046 92:20 - Immunomodulatory Agents - 302046 92:92 - Other Miscellaneous Therapeutic Agents - 12:20.92 - Skeletal Muscle Relaxants, Miscellaneous - Adapalene 84:92 - Skin and Mucous Membrane Agents, Acalabrutinib 10:00 - Antineoplastic Agents - 317059 Adefovir Acamprosate 8:18.32 - Nucleosides and Nucleotides - 302036 28:92 - Central Nervous System Agents, Adenosine 24:04.04.24 - Class IV Antiarrhythmics - 304010 Acarbose Adenovirus Vaccine Live Oral 68:20.02 - alpha-Glucosidase Inhibitors - 396015 80:12 - Vaccines - 315016 Acebutolol Ado-Trastuzumab 24:24 - beta-Adrenergic Blocking Agents - 387003 10:00 - Antineoplastic Agents - 313041 12:16.08.08 - Selective -

Horizon Scanning Status Report June 2019
Statement of Funding and Purpose This report incorporates data collected during implementation of the Patient-Centered Outcomes Research Institute (PCORI) Health Care Horizon Scanning System, operated by ECRI Institute under contract to PCORI, Washington, DC (Contract No. MSA-HORIZSCAN-ECRI-ENG- 2018.7.12). The findings and conclusions in this document are those of the authors, who are responsible for its content. No statement in this report should be construed as an official position of PCORI. An intervention that potentially meets inclusion criteria might not appear in this report simply because the horizon scanning system has not yet detected it or it does not yet meet inclusion criteria outlined in the PCORI Health Care Horizon Scanning System: Horizon Scanning Protocol and Operations Manual. Inclusion or absence of interventions in the horizon scanning reports will change over time as new information is collected; therefore, inclusion or absence should not be construed as either an endorsement or rejection of specific interventions. A representative from PCORI served as a contracting officer’s technical representative and provided input during the implementation of the horizon scanning system. PCORI does not directly participate in horizon scanning or assessing leads or topics and did not provide opinions regarding potential impact of interventions. Financial Disclosure Statement None of the individuals compiling this information have any affiliations or financial involvement that conflicts with the material presented in this report. Public Domain Notice This document is in the public domain and may be used and reprinted without special permission. Citation of the source is appreciated. All statements, findings, and conclusions in this publication are solely those of the authors and do not necessarily represent the views of the Patient-Centered Outcomes Research Institute (PCORI) or its Board of Governors. -

211172Orig1s000
CENTER FOR DRUG EVALUATION AND RESEARCH APPLICATION NUMBER: 211172Orig1s000 CLINICAL REVIEW(S) Combined Clinical/Biostatistical Review Clinical Reviewer – Breder; Statistical Reviewer – Massie NDA 211172 Tegsedi (inotersen) CLINICAL REVIEW Application Type Original NDA Application Number(s) 211172 Priority or Standard Priority Submit Date(s) 11/6/17 Received Date(s) 11/6/17 PDUFA Goal Date 10/6/18 (Extension); 7/6/18 (Original) Division/Office DNP/ODEI Reviewer Name(s) Clinical Reviewer – Christopher Breder; Statistical Reviewer – Tristan Massie Review Completion Date October 4, 2018 Established/Proper Name Inotersen (Proposed) Trade Name Tegsedi Applicant Ionis Pharmaceuticals, Inc. Dosage Form(s) 284 mg inotersen (300 mg sodium salt)/ 1.5 mL in a single- dose, prefilled syringe including a safety syringe device. Applicant Proposed (b) (4) Dosing Regimen(s) doses should be administered once every week (b) (4) Applicant Proposed For treatment of adult patients with hereditary TTR amyloidosis Indication(s)/Population(s) with polyneuropathy (hATTR-PN) (b) (4) Recommendation on Substantial evidence of effectiveness has been provided Regulatory Action Recommended For treatment of the polyneuropathy of hereditary transthyretin- Indication(s)/Population(s) mediated amyloidosis (if applicable) 1 Reference ID: 4330479 Combined Clinical/Biostatistical Review Clinical Reviewer – Breder; Statistical Reviewer – Massie NDA 211172 Tegsedi (inotersen) Table of Contents Glossary ......................................................................................................................................... -

Specialty Pharmacy Program Drug List
Specialty Pharmacy Program Drug List The Specialty Pharmacy Program covers certain drugs commonly referred to as high-cost Specialty Drugs. To receive in- network benefits/coverage for these drugs, these drugs must be dispensed through a select group of contracted specialty pharmacies or your medical provider. Please call the BCBSLA Customer Service number on the back of your member ID card for information about our contracted specialty pharmacies. All specialty drugs listed below are limited to the retail day supply listed in your benefit plan (typically a 30-day supply). As benefits may vary by group and individual plans, the inclusion of a medication on this list does not imply prescription drug coverage. Please refer to your benefit plan for a complete list of benefits, including specific exclusions, limitations and member cost-sharing amounts you are responsible for such as a deductible, copayment and coinsurance. Brand Name Generic Name Drug Classification 8-MOP methoxsalen Psoralen ACTEMRA SC tocilizumab Monoclonal Antibody/Arthritis ACTHAR corticotropin Adrenocortical Insufficiency ACTIMMUNE interferon gamma 1b Interferon ADCIRCA tadalafil Pulmonary Vasodilator ADEMPAS riociguat Pulmonary Vasodilator AFINITOR everolimus Oncology ALECENSA alectinib Oncology ALKERAN (oral) melphalan Oncology ALUNBRIG brigatinib Oncology AMPYRA ER dalfampridine Multiple Sclerosis APTIVUS tipranavir HIV/AIDS APOKYN apomorphine Parkinson's Disease ARCALYST rilonacept Interleukin Blocker/CAPS ATRIPLA efavirenz-emtricitabine-tenofovir HIV/AIDS AUBAGIO -

208078Orig1s000
CENTER FOR DRUG EVALUATION AND RESEARCH APPLICATION NUMBER: 208078Orig1s000 ADMINISTRATIVE and CORRESPONDENCE DOCUMENTS DEPARTMENT OF HEALTH AND HUMAN SERVICES Food and Drug Administration Silver Spring MD 20993 IND 106263 MEETING MINUTES Catalyst Pharmaceutical, Inc. Attention: Gary Ingenito, MD, PhD Chief Medical Officer and Head of Regulatory Affairs 355 Alhambra Circle, Suite 1250 Coral Gables, FL 33134 Dear Dr. Ingenito: Please refer to your Investigational New Drug Application (IND) submitted under section 505(i) of the Federal Food, Drug, and Cosmetic Act for amifampridine phosphate. We also refer to the meeting between representatives of your firm and the FDA on January 30, 2018. The purpose of the meeting was to review and discuss the planned contents of an NDA for amifampridine phosphate for the indication of Lambert-Eaton myasthenic syndrome and (b) (4) congenital myasthenic syndromes. A copy of the official minutes of the meeting is enclosed for your information. Please notify us of any significant differences in understanding regarding the meeting outcomes. If you have any questions, contact Laurie Kelley, Senior Regulatory Project Manager at [email protected]. Sincerely, {See appended electronic signature page} Billy Dunn, M.D. Director Division of Neurology Products Office of Drug Evaluation I Center for Drug Evaluation and Research Enclosure: Meeting Minutes Reference ID: 4216624 Reference ID: 4355913 FOOD AND DRUG ADMINISTRATION CENTER FOR DRUG EVALUATION AND RESEARCH MEMORANDUM OF MEETING MINUTES Meeting Type: C Meeting Category: Guidance Meeting Date and Time: January 30, 2018 11:00am – 12:00pm EST Meeting Location: FDA White Oak, Building 22 Application Number: IND 106263 Product Name: amifampridine phosphate Indication: Lambert-Eaton myasthenic syndrome and congenital myasthenic syndromes Sponsor/Applicant Name: Catalyst Pharmaceutical, Inc. -

The Clinical Trial Landscape in Amyotrophic Lateral Sclerosis—Past, Present, and Future
Received: 16 September 2019 | Revised: 8 December 2019 | Accepted: 27 January 2020 DOI: 10.1002/med.21661 REVIEW ARTICLE The clinical trial landscape in amyotrophic lateral sclerosis—Past, present, and future Heike J. Wobst1 | Korrie L. Mack2,3 | Dean G. Brown4 | Nicholas J. Brandon1 | James Shorter2 1Neuroscience, BioPharmaceuticals R&D, AstraZeneca, Boston, Massachusetts Abstract 2 Department of Biochemistry and Biophysics, Amyotrophic lateral sclerosis (ALS) is a fatal neurodegen- Perelman School of Medicine, University of erative disease marked by progressive loss of muscle func- Pennsylvania, Philadelphia, Pennsylvania ‐ 3Merck & Co, Inc, Kenilworth, New Jersey tion. It is the most common adult onset form of motor 4Hit Discovery, Discovery Sciences, neuron disease, affecting about 16 000 people in the United BioPharmaceuticals R&D, AstraZeneca, Boston, States alone. The average survival is about 3 years. Only two Massachusetts interventional drugs, the antiglutamatergic small‐molecule Correspondence riluzole and the more recent antioxidant edaravone, have Heike J. Wobst, Jnana Therapeutics, Northern been approved for the treatment of ALS to date. Therapeutic Avenue, Boston, MA 02210. Email: [email protected] strategies under investigation in clinical trials cover a range of different modalities and targets, and more than 70 dif- James Shorter, Department of Biochemistry and Biophysics, Perelman School of Medicine, ferent drugs have been tested in the clinic to date. Here, we University of Pennsylvania, Philadelphia, PA summarize and classify interventional therapeutic strategies 19104. Email: [email protected] based on their molecular targets and phenotypic effects. We also discuss possible reasons for the failure of clinical trials in Present address Heike J. Wobst, Dean G. -

Amifampridine Prior Authorization with Quantity Limit Program
Amifampridine Prior Authorization with Quantity Limit Program Summary FDA APPROVED INDICATIONS AND DOSAGE1-2 Agent(s) Indication(s) Dosage Firdapse® ● Treatment of Lambert- LEMS: (amifampridine) oral tablet Eaton myasthenic syndrome - The recommended (LEMS) in adults starting dosage is 15 mg to 30 mg daily, taken orally in divided doses (3 to 4 times daily) - The dosage can be increased by 5 mg daily every 3 to 4 days - The maximum single dose is 20 mg and the maximum total daily dosage is 80 mg Ruzurgi® ● Treatment of Lambert- Pediatric patients 6 to (amifampridine) oral tablet Eaton myasthenic syndrome less than 17 years of age (LEMS) in patients 6 to less weighing 45 kg or more: than 17 years of age - Initial dosage 15 mg to 30 mg daily, in divided doses (2 to 3 times per day) - Increase daily in 5 mg to 10 mg increments, divided in up to 5 doses per day - The maximum single dose is 30 mg and the maximum total daily maintenance dose is 100 mg Pediatric patients 6 to less than 17 years of age weighing less than 45 kg: - Initial dosage 7.5 mg to 15 mg daily, in divided doses (2 to 3 times per day) - Increase daily in 2.5 mg to 5 mg increments, divided in up to 5 doses per day KS_PS_Amifampridine_PAQL_ProgSum_AR1220 Page 1 of 6 © Copyright Prime Therapeutics LLC. 12/2020 All Rights Reserved Effective 03/01/2021 - The maximum single dose is 15 mg and the maximum total daily maintenance dose is 50 mg CLINICAL RATIONALE Lambert-Eaton myasthenic syndrome Lambert-Eaton myasthenic syndrome (LEMS) is a rare autoimmune disorder characterized by the gradual onset of muscle weakness, especially of the pelvic and thigh muscles. -

Wednesday, June 12, 2019 4:00Pm
Wednesday, June 12, 2019 4:00pm Oklahoma Health Care Authority 4345 N. Lincoln Blvd. Oklahoma City, OK 73105 The University of Oklahoma Health Sciences Center COLLEGE OF PHARMACY PHARMACY MANAGEMENT CONSULTANTS MEMORANDUM TO: Drug Utilization Review (DUR) Board Members FROM: Melissa Abbott, Pharm.D. SUBJECT: Packet Contents for DUR Board Meeting – June 12, 2019 DATE: June 5, 2019 Note: The DUR Board will meet at 4:00pm. The meeting will be held at 4345 N. Lincoln Blvd. Enclosed are the following items related to the June meeting. Material is arranged in order of the agenda. Call to Order Public Comment Forum Action Item – Approval of DUR Board Meeting Minutes – Appendix A Update on Medication Coverage Authorization Unit/Use of Angiotensin Converting Enzyme Inhibitor (ACEI)/ Angiotensin Receptor Blocker (ARB) Therapy in Patients with Diabetes and Hypertension (HTN) Mailing Update – Appendix B Action Item – Vote to Prior Authorize Aldurazyme® (Laronidase) and Naglazyme® (Galsulfase) – Appendix C Action Item – Vote to Prior Authorize Plenvu® [Polyethylene Glycol (PEG)-3350/Sodium Ascorbate/Sodium Sulfate/Ascorbic Acid/Sodium Chloride/Potassium Chloride] – Appendix D Action Item – Vote to Prior Authorize Consensi® (Amlodipine/Celecoxib) and Kapspargo™ Sprinkle [Metoprolol Succinate Extended-Release (ER)] – Appendix E Action Item – Vote to Update the Prior Authorization Criteria For H.P. Acthar® Gel (Repository Corticotropin Injection) – Appendix F Action Item – Vote to Prior Authorize Fulphila® (Pegfilgrastim-jmdb), Nivestym™ (Filgrastim-aafi), -

Blue Cross and Blue Shield Enhanced July 2021 Dispensing Limits
Enhanced Dispensing Limits (DL) Drug dispensing limits help encourage medication use as intended by the FDA. Coverage limits are placed on medications in certain drug categories. Limits may include: • Quantity of covered medication per prescription • Quantity of covered medication in a given time period If your doctor prescribes a greater quantity of medication than what the dispensing limit allows, you can still get the medication. However, you will be responsible for the full cost of the prescription beyond what your coverage allows. The following brand drugs, and their generic equivalents, if available, have dispensing limits. Some of these dispensing limits may not apply to all members or may vary based on state regulations. Some dispensing limits listed below may apply across multiple medications within a drug class. Some plans may exclude coverage for certain agents or drug categories, like those used for erectile dysfunction (example: Viagra). Some drugs may not be available through mail service. Coverage for some drug categories, such as specialty or other select non-specialty medications, may be limited to a 30‑day supply at a time depending on your particular benefit plan. Please see your plan materials or call the number on the back of your ID card to verify if you are uncertain of any plan limitations or exclusions. This list is subject to change. Generic and Brand (BG), Brand Only (B), Drug (generic) strength Dispensing Limit Generic only (G) abacavir 20 mg/mL oral solution (Ziagen) 960 mL per 30 days BG abacavir 300 mg tablet -
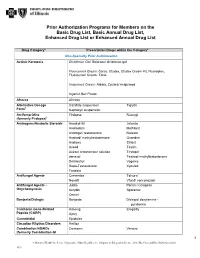
Prior Authorization Programs for Members on the Basic Drug List, Basic Annual Drug List, Enhanced Drug List Or Enhanced Annual Drug List
Prior Authorization Programs for Members on the Basic Drug List, Basic Annual Drug List, Enhanced Drug List or Enhanced Annual Drug List Drug Category* Prescription Drugs within the Category* Non-Specialty Prior Authorization Actinic Keratosis Diclofenac Gel: Solaraze/ diclofenac gel Fluorouracil Cream: Carac, Efudex, Efudex Cream Kit, Fluoroplex, Fluorouracil Cream, Tolak Imiquimod Cream: Aldara, Zyclara/ imiquimod Ingenol Gel: Picato Afrezza Afrezza Alternative Dosage Carafate suspension Tiglutik † Form Naprosyn suspension Amifampridine Firdapse Ruzurgi (formerly Firdapse)† Androgens/Anabolic Steroids Anadrol-50 Jatenzo Androderm Methitest Androgel/ testosterone Natesto Android/ methyltestosterone Oxandrin Androxy Striant Aveed Testim Axiron/ testosterone solution Testopel danazol Testred/ methyltestosterone Delatestryl Vogelxo Depo-Testosterone Xyosted Fortesta Antifungal Agents Cresemba Tolsura† Noxafil Vfend/ voriconazole Antifungal Agents – Jublia Penlac/ ciclopirox Onychomycosis Kerydin Sporanox Onmel Bonjesta/Diclegis Bonjesta Diclegis/ doxylamine - pyridoxine Calcitonin Gene-Related Aimovig Emgality Peptide (CGRP) Ajovy Cannabidiol Epidiolex Circadian Rhythm Disorders Hetlioz Combination NSAIDs Consensi Vimovo (formerly Combination GI 1 A Division of Health Care Service Corporation, a Mutual Legal Reserve Company, an Independent Licensee of the Blue Cross and Blue Shield Association 1019 Protectants) Duexis Yosprala Erectile Dysfunction Caverject Muse (ED) Cialis/ tadalafil Staxyn Edex Stendra Levitra/ vardenafil Viagra/sildenafil -

Amifampridine Phosphate (Firdapse®)
AMIFAMPRIDINE PHOSPHATE (FIRDAPSEVR ) IS EFFECTIVE AND SAFE IN A PHASE 3 CLINICAL TRIAL IN LEMS SHIN J OH, MD,1 NATALYA SHCHERBAKOVA, MD,2 ANNA KOSTERA-PRUSZCZYK, MD, PhD,3 MOHAMMAD ALSHARABATI, MD,1 MAZEN DIMACHKIE, MD,4 JOSE MUNOZ BLANCO, MD,5 THOMAS BRANNAGAN, MD,6 DRAGANA LAVRNIC´ , MD, PhD,7 PERRY B SHIEH, MD, PhD,8 CHRISTOPHE VIAL, MD,9 ANDREAS MEISEL, MD,10 SAMUEL KOMOLY, MD, PhD, DSc,11 BENEDIKT SCHOSER, MD,12 KUMARASWAMY SIVAKUMAR, MD,13 YUEN SO, MD, PhD,14 and LEMS STUDY GROUP 1 Department of Neurology, University of Alabama at Birmingham, Birmingham, Alabama, USA 2 Russian Academy of Medical Sciences, Scientific Center of Neurology, Moscow, Russia 3 Department of Neurology, Medical University of Warsaw, Poland 4 University of Kansas Medical Center, Kansas City, Kansas, USA 5 Gregorio Maranon Hospital, Madrid, Spain 6 Columbia University Medical Center, New York, New York, USA 7 Clinical Center of Serbia, Clinic of Neurology, Belgrade, Serbia 8 Department of Neurology, University of California, Los Angeles, California, USA 9 Hospital of Lyon, ENMG Service and Neuromuscular Pathology Hospital, Lyon, France 10 Charite Universitatsmedizin Berlin-NeuroCure Clinical Research Center, Berlin, Germany 11 University of Pecs, Department of Neurology, Pecs, Hungary 12 Ludwig-Maximilians-University Munich Friedrich-Baur-Institute, Munich, Germany 13 Neuromuscular Research Center, Phoenix, Arizona, USA [email protected] 14 Stanford University, Stanford, California, USA Accepted 4 February 2016 ABSTRACT: Objective: We evaluated the efficacy and safety ated; the most common adverse events were oral and digital of amifampridine phosphate (FirdapseVR ) for symptomatic treat- paresthesias, nausea, and headache. Conclusions: This study ment in Lambert-Eaton myasthenic syndrome (LEMS).