Amifampridine Phosphate (Firdapse®)
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Minutes of the CHMP Meeting 14-17 September 2020
13 January 2021 EMA/CHMP/625456/2020 Corr.1 Human Medicines Division Committee for medicinal products for human use (CHMP) Minutes for the meeting on 14-17 September 2020 Chair: Harald Enzmann – Vice-Chair: Bruno Sepodes Disclaimers Some of the information contained in these minutes is considered commercially confidential or sensitive and therefore not disclosed. With regard to intended therapeutic indications or procedure scopes listed against products, it must be noted that these may not reflect the full wording proposed by applicants and may also vary during the course of the review. Additional details on some of these procedures will be published in the CHMP meeting highlights once the procedures are finalised and start of referrals will also be available. Of note, these minutes are a working document primarily designed for CHMP members and the work the Committee undertakes. Note on access to documents Some documents mentioned in the minutes cannot be released at present following a request for access to documents within the framework of Regulation (EC) No 1049/2001 as they are subject to on- going procedures for which a final decision has not yet been adopted. They will become public when adopted or considered public according to the principles stated in the Agency policy on access to documents (EMA/127362/2006). 1 Addition of the list of participants Official address Domenico Scarlattilaan 6 ● 1083 HS Amsterdam ● The Netherlands Address for visits and deliveries Refer to www.ema.europa.eu/how-to-find-us Send us a question Go to www.ema.europa.eu/contact Telephone +31 (0)88 781 6000 An agency of the European Union © European Medicines Agency, 2020. -

Biomarin Pharmaceutical Inc
BIOMARIN PHARMACEUTICAL INC FORM 10-K (Annual Report) Filed 03/02/15 for the Period Ending 12/31/14 Address 105 DIGITAL DRIVE NOVATO, CA 94949 Telephone 4155066700 CIK 0001048477 Symbol BMRN SIC Code 2834 - Pharmaceutical Preparations Industry Biotechnology & Drugs Sector Healthcare Fiscal Year 12/31 http://www.edgar-online.com © Copyright 2015, EDGAR Online, Inc. All Rights Reserved. Distribution and use of this document restricted under EDGAR Online, Inc. Terms of Use. f UNITED STATES SECURITIES AND EXCHANGE COMMISSION Washington, D.C. 20549 Form 10-K (Mark One) ANNUAL REPORT PURSUANT TO SECTION 13 OR 15(d) OF THE SECURITIES EXCHANGE ACT OF 1934 For the fiscal year ended December 31, 2014 Or TRANSITION REPORT PURSUANT TO SECTION 13 OR 15(d) OF THE SECURITIES EXCHANGE ACT OF 1934 For the transition period from to . Commission file number: 000-26727 BioMarin Pharmaceutical Inc. (Exact name of registrant as specified in its charter) Delaware 68 -0397820 (State of other jurisdiction of (I.R.S. Employer incorporation or organization) Identification No.) 770 Lindaro Street San Rafael, California 94901 (Address of principal executive offices) (Zip Code) Registrant’s telephone number, including area code: (415) 506-6700 Securities registered pursuant to Section 12(b) of the Act: Title of Each Class Name of Each Exchange on Which Registered Common Stock, $.001 par value The NASDAQ Global Select Market Securities registered under Section 12(g) of the Act: None Indicate by check mark if the registrant is a well-known seasoned issuer, as defined in Rule 405 of the Securities Act. Yes No Indicate by check mark if the registrant is not required to file reports pursuant to Section 13 or Section 15(d) of the Act. -

AHFS Pharmacologic-Therapeutic Classification System
AHFS Pharmacologic-Therapeutic Classification System Abacavir 48:24 - Mucolytic Agents - 382638 8:18.08.20 - HIV Nucleoside and Nucleotide Reverse Acitretin 84:92 - Skin and Mucous Membrane Agents, Abaloparatide 68:24.08 - Parathyroid Agents - 317036 Aclidinium Abatacept 12:08.08 - Antimuscarinics/Antispasmodics - 313022 92:36 - Disease-modifying Antirheumatic Drugs - Acrivastine 92:20 - Immunomodulatory Agents - 306003 4:08 - Second Generation Antihistamines - 394040 Abciximab 48:04.08 - Second Generation Antihistamines - 394040 20:12.18 - Platelet-aggregation Inhibitors - 395014 Acyclovir Abemaciclib 8:18.32 - Nucleosides and Nucleotides - 381045 10:00 - Antineoplastic Agents - 317058 84:04.06 - Antivirals - 381036 Abiraterone Adalimumab; -adaz 10:00 - Antineoplastic Agents - 311027 92:36 - Disease-modifying Antirheumatic Drugs - AbobotulinumtoxinA 56:92 - GI Drugs, Miscellaneous - 302046 92:20 - Immunomodulatory Agents - 302046 92:92 - Other Miscellaneous Therapeutic Agents - 12:20.92 - Skeletal Muscle Relaxants, Miscellaneous - Adapalene 84:92 - Skin and Mucous Membrane Agents, Acalabrutinib 10:00 - Antineoplastic Agents - 317059 Adefovir Acamprosate 8:18.32 - Nucleosides and Nucleotides - 302036 28:92 - Central Nervous System Agents, Adenosine 24:04.04.24 - Class IV Antiarrhythmics - 304010 Acarbose Adenovirus Vaccine Live Oral 68:20.02 - alpha-Glucosidase Inhibitors - 396015 80:12 - Vaccines - 315016 Acebutolol Ado-Trastuzumab 24:24 - beta-Adrenergic Blocking Agents - 387003 10:00 - Antineoplastic Agents - 313041 12:16.08.08 - Selective -

Reducing Prescription Drug Costs in Colorado Cost Drivers and Strategies to Address Them
2nd Edition Reducing Prescription Drug Costs in Colorado Cost Drivers and Strategies to Address Them January 2021 Contents Forward to Reducing Prescription Drug Costs in Colorado, 2nd Edition ........... 4 2020 Updates to This Report .................................................................. 4 Executive Summary ............................................................................ 6 Introduction and Purpose ...................................................................... 6 Cost Drivers ...................................................................................... 7 Prioritized Solutions ............................................................................ 8 Learning from Medicaid Policy ............................................................... 12 The Department Invites Your Collaborative Partnership .................................. 12 Industry Trends and Background Information ............................................. 13 Prescription Drug Cost, Utilization, and Trends ........................................... 13 The U.S. Pays the Highest Prices for Pharmaceutical Drugs in the World .............. 16 Many Coloradans Aren’t Taking Their Drugs Appropriately Because They Can’t Afford Them, Often Leading to Worse Health Outcomes That Are More Costly ....... 16 Major Drivers of Prescription Drug Prices .................................................. 18 Patent Protections .............................................................................. 18 Anti-Competitive Practices and Price Fixing -

208078Orig1s000
CENTER FOR DRUG EVALUATION AND RESEARCH APPLICATION NUMBER: 208078Orig1s000 ADMINISTRATIVE and CORRESPONDENCE DOCUMENTS DEPARTMENT OF HEALTH AND HUMAN SERVICES Food and Drug Administration Silver Spring MD 20993 IND 106263 MEETING MINUTES Catalyst Pharmaceutical, Inc. Attention: Gary Ingenito, MD, PhD Chief Medical Officer and Head of Regulatory Affairs 355 Alhambra Circle, Suite 1250 Coral Gables, FL 33134 Dear Dr. Ingenito: Please refer to your Investigational New Drug Application (IND) submitted under section 505(i) of the Federal Food, Drug, and Cosmetic Act for amifampridine phosphate. We also refer to the meeting between representatives of your firm and the FDA on January 30, 2018. The purpose of the meeting was to review and discuss the planned contents of an NDA for amifampridine phosphate for the indication of Lambert-Eaton myasthenic syndrome and (b) (4) congenital myasthenic syndromes. A copy of the official minutes of the meeting is enclosed for your information. Please notify us of any significant differences in understanding regarding the meeting outcomes. If you have any questions, contact Laurie Kelley, Senior Regulatory Project Manager at [email protected]. Sincerely, {See appended electronic signature page} Billy Dunn, M.D. Director Division of Neurology Products Office of Drug Evaluation I Center for Drug Evaluation and Research Enclosure: Meeting Minutes Reference ID: 4216624 Reference ID: 4355913 FOOD AND DRUG ADMINISTRATION CENTER FOR DRUG EVALUATION AND RESEARCH MEMORANDUM OF MEETING MINUTES Meeting Type: C Meeting Category: Guidance Meeting Date and Time: January 30, 2018 11:00am – 12:00pm EST Meeting Location: FDA White Oak, Building 22 Application Number: IND 106263 Product Name: amifampridine phosphate Indication: Lambert-Eaton myasthenic syndrome and congenital myasthenic syndromes Sponsor/Applicant Name: Catalyst Pharmaceutical, Inc. -

Amifampridine Prior Authorization with Quantity Limit Program
Amifampridine Prior Authorization with Quantity Limit Program Summary FDA APPROVED INDICATIONS AND DOSAGE1-2 Agent(s) Indication(s) Dosage Firdapse® ● Treatment of Lambert- LEMS: (amifampridine) oral tablet Eaton myasthenic syndrome - The recommended (LEMS) in adults starting dosage is 15 mg to 30 mg daily, taken orally in divided doses (3 to 4 times daily) - The dosage can be increased by 5 mg daily every 3 to 4 days - The maximum single dose is 20 mg and the maximum total daily dosage is 80 mg Ruzurgi® ● Treatment of Lambert- Pediatric patients 6 to (amifampridine) oral tablet Eaton myasthenic syndrome less than 17 years of age (LEMS) in patients 6 to less weighing 45 kg or more: than 17 years of age - Initial dosage 15 mg to 30 mg daily, in divided doses (2 to 3 times per day) - Increase daily in 5 mg to 10 mg increments, divided in up to 5 doses per day - The maximum single dose is 30 mg and the maximum total daily maintenance dose is 100 mg Pediatric patients 6 to less than 17 years of age weighing less than 45 kg: - Initial dosage 7.5 mg to 15 mg daily, in divided doses (2 to 3 times per day) - Increase daily in 2.5 mg to 5 mg increments, divided in up to 5 doses per day KS_PS_Amifampridine_PAQL_ProgSum_AR1220 Page 1 of 6 © Copyright Prime Therapeutics LLC. 12/2020 All Rights Reserved Effective 03/01/2021 - The maximum single dose is 15 mg and the maximum total daily maintenance dose is 50 mg CLINICAL RATIONALE Lambert-Eaton myasthenic syndrome Lambert-Eaton myasthenic syndrome (LEMS) is a rare autoimmune disorder characterized by the gradual onset of muscle weakness, especially of the pelvic and thigh muscles. -

Wednesday, June 12, 2019 4:00Pm
Wednesday, June 12, 2019 4:00pm Oklahoma Health Care Authority 4345 N. Lincoln Blvd. Oklahoma City, OK 73105 The University of Oklahoma Health Sciences Center COLLEGE OF PHARMACY PHARMACY MANAGEMENT CONSULTANTS MEMORANDUM TO: Drug Utilization Review (DUR) Board Members FROM: Melissa Abbott, Pharm.D. SUBJECT: Packet Contents for DUR Board Meeting – June 12, 2019 DATE: June 5, 2019 Note: The DUR Board will meet at 4:00pm. The meeting will be held at 4345 N. Lincoln Blvd. Enclosed are the following items related to the June meeting. Material is arranged in order of the agenda. Call to Order Public Comment Forum Action Item – Approval of DUR Board Meeting Minutes – Appendix A Update on Medication Coverage Authorization Unit/Use of Angiotensin Converting Enzyme Inhibitor (ACEI)/ Angiotensin Receptor Blocker (ARB) Therapy in Patients with Diabetes and Hypertension (HTN) Mailing Update – Appendix B Action Item – Vote to Prior Authorize Aldurazyme® (Laronidase) and Naglazyme® (Galsulfase) – Appendix C Action Item – Vote to Prior Authorize Plenvu® [Polyethylene Glycol (PEG)-3350/Sodium Ascorbate/Sodium Sulfate/Ascorbic Acid/Sodium Chloride/Potassium Chloride] – Appendix D Action Item – Vote to Prior Authorize Consensi® (Amlodipine/Celecoxib) and Kapspargo™ Sprinkle [Metoprolol Succinate Extended-Release (ER)] – Appendix E Action Item – Vote to Update the Prior Authorization Criteria For H.P. Acthar® Gel (Repository Corticotropin Injection) – Appendix F Action Item – Vote to Prior Authorize Fulphila® (Pegfilgrastim-jmdb), Nivestym™ (Filgrastim-aafi), -

Blue Cross and Blue Shield Enhanced July 2021 Dispensing Limits
Enhanced Dispensing Limits (DL) Drug dispensing limits help encourage medication use as intended by the FDA. Coverage limits are placed on medications in certain drug categories. Limits may include: • Quantity of covered medication per prescription • Quantity of covered medication in a given time period If your doctor prescribes a greater quantity of medication than what the dispensing limit allows, you can still get the medication. However, you will be responsible for the full cost of the prescription beyond what your coverage allows. The following brand drugs, and their generic equivalents, if available, have dispensing limits. Some of these dispensing limits may not apply to all members or may vary based on state regulations. Some dispensing limits listed below may apply across multiple medications within a drug class. Some plans may exclude coverage for certain agents or drug categories, like those used for erectile dysfunction (example: Viagra). Some drugs may not be available through mail service. Coverage for some drug categories, such as specialty or other select non-specialty medications, may be limited to a 30‑day supply at a time depending on your particular benefit plan. Please see your plan materials or call the number on the back of your ID card to verify if you are uncertain of any plan limitations or exclusions. This list is subject to change. Generic and Brand (BG), Brand Only (B), Drug (generic) strength Dispensing Limit Generic only (G) abacavir 20 mg/mL oral solution (Ziagen) 960 mL per 30 days BG abacavir 300 mg tablet -
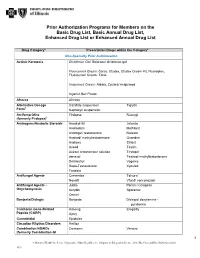
Prior Authorization Programs for Members on the Basic Drug List, Basic Annual Drug List, Enhanced Drug List Or Enhanced Annual Drug List
Prior Authorization Programs for Members on the Basic Drug List, Basic Annual Drug List, Enhanced Drug List or Enhanced Annual Drug List Drug Category* Prescription Drugs within the Category* Non-Specialty Prior Authorization Actinic Keratosis Diclofenac Gel: Solaraze/ diclofenac gel Fluorouracil Cream: Carac, Efudex, Efudex Cream Kit, Fluoroplex, Fluorouracil Cream, Tolak Imiquimod Cream: Aldara, Zyclara/ imiquimod Ingenol Gel: Picato Afrezza Afrezza Alternative Dosage Carafate suspension Tiglutik † Form Naprosyn suspension Amifampridine Firdapse Ruzurgi (formerly Firdapse)† Androgens/Anabolic Steroids Anadrol-50 Jatenzo Androderm Methitest Androgel/ testosterone Natesto Android/ methyltestosterone Oxandrin Androxy Striant Aveed Testim Axiron/ testosterone solution Testopel danazol Testred/ methyltestosterone Delatestryl Vogelxo Depo-Testosterone Xyosted Fortesta Antifungal Agents Cresemba Tolsura† Noxafil Vfend/ voriconazole Antifungal Agents – Jublia Penlac/ ciclopirox Onychomycosis Kerydin Sporanox Onmel Bonjesta/Diclegis Bonjesta Diclegis/ doxylamine - pyridoxine Calcitonin Gene-Related Aimovig Emgality Peptide (CGRP) Ajovy Cannabidiol Epidiolex Circadian Rhythm Disorders Hetlioz Combination NSAIDs Consensi Vimovo (formerly Combination GI 1 A Division of Health Care Service Corporation, a Mutual Legal Reserve Company, an Independent Licensee of the Blue Cross and Blue Shield Association 1019 Protectants) Duexis Yosprala Erectile Dysfunction Caverject Muse (ED) Cialis/ tadalafil Staxyn Edex Stendra Levitra/ vardenafil Viagra/sildenafil -

Effects of Food Intake on the Relative Bioavailability of Amifampridine Phosphate Salt in Healthy Adults
Clinical Therapeutics/Volume 37, Number 7, 2015 Effects of Food Intake on the Relative Bioavailability of Amifampridine Phosphate Salt in Healthy Adults Peter E. Haroldsen, PhD; Donald G. Musson, PhD; Boyd Hanson, PhD; Adrian Quartel, MD; and Charles A. O’Neill, PhD BioMarin Pharmaceutical Inc, Novato, California ABSTRACT in the fed state. The extent of exposure and plasma Purpose: Amifampridine (3,4-diaminopyridine) has elimination half-life of the major metabolite was been approved in the European Union for the treatment greater than those of amifampridine in the fed and of Lambert-Eaton myasthenic syndrome. Amifampridine fasted conditions. Mean AUCs in the fed and fasted has a narrow therapeutic index, and supratherapeutic states were slightly greater in women than men, with exposure has been associated with dose-dependent ad- no difference in mean Cmax. Orally administered verse events, including an increased risk for seizure. This amifampridine was renally eliminated (493%) as study assessed the effect of food on the relative bioavail- the parent compound and metabolite within 24 hours. ability of amifampridine in healthy subjects and informed Single oral doses of 20 mg of amifampridine phos- on conditions that can alter exposure. phate salt were considered well tolerated in both the Methods: This randomized, open-labeled, 2-treat- fed and fasted conditions. High intersubject variability ment, 2-period crossover study enrolled 47 healthy (%CVs, 430%) in amifampridine pharmacokinetic male and female subjects. Subjects were randomly parameter values was observed. assigned to receive 2 single oral doses of amifampri- Implications: At the intended dose under fasting dine phosphate salt (20 mg base equivalents per dose) conditions, amifampridine exposure may be increased. -

Catalyst Pharmaceutical Partners Provides Update on Research and Development Pipeline
February 11, 2013 Catalyst Pharmaceutical Partners Provides Update on Research and Development Pipeline CORAL GABLES, Fla., Feb. 11, 2013 (GLOBE NEWSWIRE) -- Catalyst Pharmaceutical Partners, Inc. (Nasdaq:CPRX), a specialty pharmaceutical company focused on the development and commercialization of novel prescription drugs targeting rare (orphan) neurological diseases and disorders, today provided an update on its research and development pipeline. "We are providing this information today to update our shareholders, patients, physicians, key opinion leaders and the financial community on our drug development activities. We are primarily focused on rapidly advancing the development of FirdapseTM for the treatment of Lambert-Eaton Myasthenic Syndrome (LEMS), which is our lead product candidate," said Patrick J. McEnany, Chief Executive Officer of Catalyst. Portfolio update Firdapse In October 2012, Catalyst acquired the North American rights to Firdapse, a proprietary form of amifampridine phosphate (3-4 diaminopyridine or 3-4 DAP), from BioMarin Pharmaceutical Inc. ("BioMarin"). Firdapse was approved in December 2009 by the European Medicines Agency for the treatment of Lambert-Eaton Myasthenic Syndrome (LEMS), a rare and sometimes fatal autoimmune disease characterized by muscle weakness. Firdapse has been granted orphan drug designation by the U.S. Food & Drug Administration, (FDA) for the treatment of LEMS, making the product eligible to obtain seven-year marketing exclusivity, if Catalyst is the first pharmaceutical company to obtain -

Clinical Outcome Assessment (Coa) Compendium
CENTER FOR DRUG EVALUATION AND RESEARCH CLINICAL OUTCOME ASSESSMENT (COA) COMPENDIUM June 2021 www.fda.gov 1 Table of Contents COA COMPENDIUM DESCRIPTION ............................................................................ 3 DIVISION OF NEUROLOGY I AND II (DN I AND II) ..........................................37 OFFICE OF CARDIOLOGY, HEMATOLOGY, ENDOCRINOLOGY, DIVISION OF PSYCHIATRIC (DP) ...........................................................................46 AND NEPHROLOGY (OCHEN) ...................................................................................... 5 DIVISION OF ANESTHESIOLOGY, ADDICTION MEDICINE AND PAIN MEDICINE DIVISION OF CARDIOLOGY AND NEPHROLOGY (DCN) ................................ 5 (DAAP)..............................................................................................................................50 DIVISION OF DIABETES, LIPID DISORDERS AND OBESITY (DDLO) .......... 9 OFFICE OF ONCOLOGIC DISEASES (OOD) ............................................................51 DIVISION OF GENERAL ENDOCRINOLOGY (DGE) ........................................... 9 DIVISION OF ONCOLOGY I (DO I).........................................................................51 DIVISION OF NON-MALIGNANT HEMATOLOGY (DNH) ..............................10 DIVISION OF ONCOLOGY II (DO II) ......................................................................51 OFFICE OF IMMUNOLOGY AND INFLAMMATION (OII) ...................................13 DIVISION OF HEMATOLOGIC MALIGNANCIES I (DHM I).............................53