Identification of a Botulinum Neurotoxin-Like Toxin in A
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

The Influence of Probiotics on the Firmicutes/Bacteroidetes Ratio In
microorganisms Review The Influence of Probiotics on the Firmicutes/Bacteroidetes Ratio in the Treatment of Obesity and Inflammatory Bowel disease Spase Stojanov 1,2, Aleš Berlec 1,2 and Borut Štrukelj 1,2,* 1 Faculty of Pharmacy, University of Ljubljana, SI-1000 Ljubljana, Slovenia; [email protected] (S.S.); [email protected] (A.B.) 2 Department of Biotechnology, Jožef Stefan Institute, SI-1000 Ljubljana, Slovenia * Correspondence: borut.strukelj@ffa.uni-lj.si Received: 16 September 2020; Accepted: 31 October 2020; Published: 1 November 2020 Abstract: The two most important bacterial phyla in the gastrointestinal tract, Firmicutes and Bacteroidetes, have gained much attention in recent years. The Firmicutes/Bacteroidetes (F/B) ratio is widely accepted to have an important influence in maintaining normal intestinal homeostasis. Increased or decreased F/B ratio is regarded as dysbiosis, whereby the former is usually observed with obesity, and the latter with inflammatory bowel disease (IBD). Probiotics as live microorganisms can confer health benefits to the host when administered in adequate amounts. There is considerable evidence of their nutritional and immunosuppressive properties including reports that elucidate the association of probiotics with the F/B ratio, obesity, and IBD. Orally administered probiotics can contribute to the restoration of dysbiotic microbiota and to the prevention of obesity or IBD. However, as the effects of different probiotics on the F/B ratio differ, selecting the appropriate species or mixture is crucial. The most commonly tested probiotics for modifying the F/B ratio and treating obesity and IBD are from the genus Lactobacillus. In this paper, we review the effects of probiotics on the F/B ratio that lead to weight loss or immunosuppression. -

Probiotic Properties of Enterococcus Faecium CE5-1 Producing A
Czech J. Anim. Sci., 57, 2012 (11): 529–539 Original Paper Probiotic properties of Enterococcus faecium CE5-1 producing a bacteriocin-like substance and its antagonistic effect against antibiotic-resistant enterococci in vitro K. Saelim1, N. Sohsomboon1, S. Kaewsuwan2, S. Maneerat1 1Department of Industrial Biotechnology, Faculty of Agro-Industry, Prince of Songkla University, Hat Yai, Thailand 2Department of Pharmacognosy and Pharmaceutical Botany, Faculty of Pharmaceutical Sciences, Prince of Songkla University, Hat Yai, Thailand ABSTRACT: A bacteriocin-like substance (BLS) producing Enterococcus faecium CE5-1 was isolated from the gastrointestinal tract (GIT) of Thai indigenous chickens. Investigations of its probiotic potential were carried out. The competition between the BLS probiotic strain and antibiotic-resistant enterococci was also studied. Ent. faecium CE5-1 exhibited a good tolerance to pH 3.0 after 2 h and in 7% fresh chicken bile after 6 h, but the viability of Ent. faecium CE5-1 decreased by about 2–3 log CFU/ml after 2 h incubation in pH 2.5. It was susceptible to the antibiotics tested (tetracycline, erythromycin, penicillin G, and vancomycin). The maximum BLS production from Ent. faecium CE5-1 was observed at 15 h of cultivation. It showed activity against Listeria monocytogenes DMST17303, Pediococcus pentosaceus 3CE27, Lactobacillus sakei subsp. sakei JCM1157, and antibiotic-resistant enterococci. The detection by polymerase chain reaction (PCR) in the enterocin structural gene determined the presence of enterocin A gene in Ent. faecium CE5-1 only. Ent. faecium CE5-1 showed the highest inhibitory activity against two antibiotic-resistant Ent. faecalis VanB (from 6.68 to 4.29 log CFU/ml) and Ent. -
![Saxitoxin Poisoning (Paralytic Shellfish Poisoning [PSP])](https://docslib.b-cdn.net/cover/6900/saxitoxin-poisoning-paralytic-shellfish-poisoning-psp-76900.webp)
Saxitoxin Poisoning (Paralytic Shellfish Poisoning [PSP])
Saxitoxin Poisoning (Paralytic Shellfish Poisoning [PSP]) PROTOCOL CHECKLIST Enter available information into Merlin upon receipt of initial report Review information on Saxitoxin and its epidemiology, case definition and exposure information Contact provider Interview patient(s) Review facts on Saxitoxin Sources of poisoning Symptoms Clinical information Ask about exposure to relevant risk factors Type of fish or shellfish Size and weight of shellfish/puffer fish or other type of fish Amount of shellfish/puffer fish or other type of fish consumed Where the shellfish/puffer fish or other type of fish was caught or purchased Where the shellfish/puffer fish or other type of fish was consumed Secure any leftover product for potential testing Restaurant meals Other Contact your Regional Environmental Epidemiologist (REE) Identify symptomatic contacts or others who ate the shellfish/puffer fish or other type of fish Enter any additional information gathered into Merlin Saxitoxin Poisoning Guide to Surveillance and Investigation Saxitoxin Poisoning 1. DISEASE REPORTING A. Purpose of reporting and surveillance 1. To gather epidemiologic and environmental data on saxitoxin shellfish, Florida puffer fish or other type of fish poisoning cases to target future public health interventions. 2. To prevent additional cases by identifying any ongoing public health threats that can be mitigated by identifying any shellfish or puffer fish available commercially and removing it from the marketplace or issuing public notices about the risks from consuming molluscan shellfish from Florida and non-Florida waters, such as from the northern Pacific and other cold water sources. 3. To identify all exposed persons with a common or shared exposure to saxitoxic shellfish or puffer fish; collect shellfish and/or puffer fish samples for testing by the Florida Fish and Wildlife Conservation Commission (FWC) and the U.S. -

Detection of ESKAPE Pathogens and Clostridioides Difficile in Simulated
bioRxiv preprint doi: https://doi.org/10.1101/2021.03.04.433847; this version posted March 4, 2021. The copyright holder for this preprint (which was not certified by peer review) is the author/funder, who has granted bioRxiv a license to display the preprint in perpetuity. It is made available under aCC-BY 4.0 International license. 1 Detection of ESKAPE pathogens and Clostridioides difficile in 2 Simulated Skin Transmission Events with Metagenomic and 3 Metatranscriptomic Sequencing 4 5 Krista L. Ternusa#, Nicolette C. Keplingera, Anthony D. Kappella, Gene D. Godboldb, Veena 6 Palsikara, Carlos A. Acevedoa, Katharina L. Webera, Danielle S. LeSassiera, Kathleen Q. 7 Schultea, Nicole M. Westfalla, and F. Curtis Hewitta 8 9 aSignature Science, LLC, 8329 North Mopac Expressway, Austin, Texas, USA 10 bSignature Science, LLC, 1670 Discovery Drive, Charlottesville, VA, USA 11 12 #Address correspondence to Krista L. Ternus, [email protected] 13 14 1 bioRxiv preprint doi: https://doi.org/10.1101/2021.03.04.433847; this version posted March 4, 2021. The copyright holder for this preprint (which was not certified by peer review) is the author/funder, who has granted bioRxiv a license to display the preprint in perpetuity. It is made available under aCC-BY 4.0 International license. 15 1 Abstract 16 Background: Antimicrobial resistance is a significant global threat, posing major public health 17 risks and economic costs to healthcare systems. Bacterial cultures are typically used to diagnose 18 healthcare-acquired infections (HAI); however, culture-dependent methods provide limited 19 presence/absence information and are not applicable to all pathogens. -

Current Trends of Enterococci in Dairy Products: a Comprehensive Review of Their Multiple Roles
foods Review Current Trends of Enterococci in Dairy Products: A Comprehensive Review of Their Multiple Roles Maria de Lurdes Enes Dapkevicius 1,2,* , Bruna Sgardioli 1,2 , Sandra P. A. Câmara 1,2, Patrícia Poeta 3,4 and Francisco Xavier Malcata 5,6,* 1 Faculty of Agricultural and Environmental Sciences, University of the Azores, 9700-042 Angra do Heroísmo, Portugal; [email protected] (B.S.); [email protected] (S.P.A.C.) 2 Institute of Agricultural and Environmental Research and Technology (IITAA), University of the Azores, 9700-042 Angra do Heroísmo, Portugal 3 Microbiology and Antibiotic Resistance Team (MicroART), Department of Veterinary Sciences, University of Trás-os-Montes and Alto Douro (UTAD), 5001-801 Vila Real, Portugal; [email protected] 4 Associated Laboratory for Green Chemistry (LAQV-REQUIMTE), University NOVA of Lisboa, 2829-516 Lisboa, Portugal 5 LEPABE—Laboratory for Process Engineering, Environment, Biotechnology and Energy, Faculty of Engineering, University of Porto, 420-465 Porto, Portugal 6 FEUP—Faculty of Engineering, University of Porto, 4200-465 Porto, Portugal * Correspondence: [email protected] (M.d.L.E.D.); [email protected] (F.X.M.) Abstract: As a genus that has evolved for resistance against adverse environmental factors and that readily exchanges genetic elements, enterococci are well adapted to the cheese environment and may reach high numbers in artisanal cheeses. Their metabolites impact cheese flavor, texture, Citation: Dapkevicius, M.d.L.E.; and rheological properties, thus contributing to the development of its typical sensorial properties. Sgardioli, B.; Câmara, S.P.A.; Poeta, P.; Due to their antimicrobial activity, enterococci modulate the cheese microbiota, stimulate autoly- Malcata, F.X. -

Cyanobacterial Toxins: Saxitoxins
WHO/SDE/WSH/xxxxx English only Cyanobacterial toxins: Saxitoxins Background document for development of WHO Guidelines for Drinking-water Quality and Guidelines for Safe Recreational Water Environments Version for Public Review Nov 2019 © World Health Organization 20XX Preface Information on cyanobacterial toxins, including saxitoxins, is comprehensively reviewed in a recent volume to be published by the World Health Organization, “Toxic Cyanobacteria in Water” (TCiW; Chorus & Welker, in press). This covers chemical properties of the toxins and information on the cyanobacteria producing them as well as guidance on assessing the risks of their occurrence, monitoring and management. In contrast, this background document focuses on reviewing the toxicological information available for guideline value derivation and the considerations for deriving the guideline values for saxitoxin in water. Sections 1-3 and 8 are largely summaries of respective chapters in TCiW and references to original studies can be found therein. To be written by WHO Secretariat Acknowledgements To be written by WHO Secretariat 5 Abbreviations used in text ARfD Acute Reference Dose bw body weight C Volume of drinking water assumed to be consumed daily by an adult GTX Gonyautoxin i.p. intraperitoneal i.v. intravenous LOAEL Lowest Observed Adverse Effect Level neoSTX Neosaxitoxin NOAEL No Observed Adverse Effect Level P Proportion of exposure assumed to be due to drinking water PSP Paralytic Shellfish Poisoning PST paralytic shellfish toxin STX saxitoxin STXOL saxitoxinol -
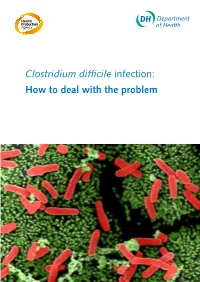
Clostridium Difficile Infection: How to Deal with the Problem DH INFORMATION RE ADER B OX
Clostridium difficile infection: How to deal with the problem DH INFORMATION RE ADER B OX Policy Estates HR / Workforce Commissioning Management IM & T Planning / Finance Clinical Social Care / Partnership Working Document Purpose Best Practice Guidance Gateway Reference 9833 Title Clostridium difficile infection: How to deal with the problem Author DH and HPA Publication Date December 2008 Target Audience PCT CEs, NHS Trust CEs, SHA CEs, Care Trust CEs, Medical Directors, Directors of PH, Directors of Nursing, PCT PEC Chairs, NHS Trust Board Chairs, Special HA CEs, Directors of Infection Prevention and Control, Infection Control Teams, Health Protection Units, Chief Pharmacists Circulation List Description This guidance outlines newer evidence and approaches to delivering good infection control and environmental hygiene. It updates the 1994 guidance and takes into account a national framework for clinical governance which did not exist in 1994. Cross Ref N/A Superseded Docs Clostridium difficile Infection Prevention and Management (1994) Action Required CEs to consider with DIPCs and other colleagues Timing N/A Contact Details Healthcare Associated Infection and Antimicrobial Resistance Department of Health Room 528, Wellington House 133-155 Waterloo Road London SE1 8UG For Recipient's Use Front cover image: Clostridium difficile attached to intestinal cells. Reproduced courtesy of Dr Jan Hobot, Cardiff University School of Medicine. Clostridium difficile infection: How to deal with the problem Contents Foreword 1 Scope and purpose 2 Introduction 3 Why did CDI increase? 4 Approach to compiling the guidance 6 What is new in this guidance? 7 Core Guidance Key recommendations 9 Grading of recommendations 11 Summary of healthcare recommendations 12 1. -
Understanding Fungal (Mold) Toxins (Mycotoxins) Michael P
® ® KFSBOPFQVLCB?O>PH>¨ FK@LIKUQBKPFLK KPQFQRQBLCDOF@RIQROB>KA>QRO>IBPLRO@BP KLTELT KLTKLT G1513 Understanding Fungal (Mold) Toxins (Mycotoxins) Michael P. Carlson, Diagnostic Toxicologist/Analytical Chemist; and Steve M. Ensley, Veterinary Toxicologist of the immune system. Common mycoses include athlete’s This NebGuide briefly discusses mycotoxins commonly foot and ringworm. encountered in grains and feeds used in Nebraska and the mycotoxicoses they cause. Myco toxin sources and clini- Diagnosis and Treatment of Mycotoxicoses cal signs, lesions, diagnostic aids and treatment for each mycotoxicosis are listed. Different mycotoxins cause different diseases. Although they all are called mycotoxicoses, they are very different from Mycotoxins are chemicals produced by fungi (molds) each other. under certain conditions. They are not essential for fungal Modern agricultural practices make acute mycotoxicoses growth or reproduction, and are toxic to animals or humans. with high death loss (mortality) rare. Chronic mycotoxicoses Scientists do not yet know how many mycotoxins may ex- are often suspected when clinical signs include poor perfor- ist, even though more than 250 have been detected. They mance, ill thrift, or increased incidence of infectious diseases. represent many different kinds of chemicals. For many, if Establishing cause and effect relationships between consump- not most, their toxicological characteristics have not been tion of mycotoxin-contaminated feed and vague chronic fully determined. conditions is very difficult. Diseases in animals caused by mycotoxins are called my- Diagnosis of mycotoxicoses is usually not very easy. cotoxicoses. There are many different kinds of mycotoxicoses Exposure cannot be established by detection of mycotoxins in because there are many different kinds of mycotoxins. -

Comparative Acute and Combinative Toxicity of Aflatoxin B1 and T-2 Toxin
JOURNAL OF APPLIED TOXICOLOGY TOXICITY OF AFLATOXIN B1 AND T-2 TOXIN 139 J. Appl. Toxicol. 2006; 26: 139–147 Published online 17 October 2005 in Wiley InterScience (www.interscience.wiley.com). DOI: 10.1002/jat.1117 Comparative acute and combinative toxicity of aflatoxin B1 and T-2 toxin in animals and immortalized human cell lines Christopher McKean, Lili Tang, Madhavi Billam, Meng Tang, Christopher W. Theodorakis, Ronald J. Kendall and Jia-Sheng Wang* The Institute of Environmental and Human Health, Department of Environmental Toxicology, Texas Tech University, Box 41163, Lubbock TX 79409-1163, USA Received 27 September 2004; Revised 14 June 2005; Accepted 8 August 2005 ABSTRACT: Aflatoxin B1 (AFB1) and T-2 toxin (T-2) are important food-borne mycotoxins that have been implicated in human health and as potential biochemical weapons threats. In this study the acute and combinative toxicity of AFB1 and T-2 were tested in F-344 rats, mosquitofish (Gambusia affinis), immortalized human hepatoma cells (HepG2) and human bronchial epithelial cells (BEAS-2B). Preliminary experiments were conducted in order to assess the acute toxicity and to obtain LD50, LC50 and IC50 values for individual toxins in each model, respectively. This was followed by testing combinations of AFB1 and T-2 to obtain LD50, LC50 and IC50 values for the combination in each model. All models demonstrated a significant dose response in the observed parameters to treatment. The potency of the mixture was gauged through the determination of the interaction index metric. The results of this study demonstrate that these two toxins interacted to produce alterations in the toxic responses generally classifiable as additive; however, a synergistic interaction was noted in the case of BEAS-2B. -

Methicillin-Resistant Staphylococcus Aureus (MRSA)
Methicillin-Resistant Staphylococcus Aureus (MRSA) Over the past several decades, the incidence of resistant gram-positive organisms has risen in the United States. MRSA strains, first identified in the 1960s in England, were first observed in the U.S. in the mid 1980s.1 Resistance quickly developed, increasing from 2.4% in 1979 to 29% in 1991.2 The current prevalence for MRSA in hospitals and other facilities ranges from <10% to 65%. In 1999, MRSA accounted for more than 50% of all Staphylococcus aureus isolates within U.S. intensive care units.3, 4 The past years, however, outbreaks of MRSA have also been seen in the community setting, particularly among preschool-age children, some of whom have attended day-care centers.5, 6, 7 MRSA does not appear to be more virulent than methicillin-sensitive Staphylococcus aureus, but certainly poses a greater treatment challenge. MRSA also has been associated with higher hospital costs and mortality.8 Within a decade of its development, methicillin resistance to Staphylococcus aureus emerged.9 MRSA strains generally are now resistant to other antimicrobial classes including aminoglycosides, beta-lactams, carbapenems, cephalosporins, fluoroquinolones and macrolides.10,11 Most of the resistance was secondary to production of beta-lactamase enzymes or intrinsic resistance with alterations in penicillin-binding proteins. Staphylococcus aureus is the most frequent cause of nosocomial pneumonia and surgical- wound infections and the second most common cause of nosocomial bloodstream infections.12 Long-term care facilities (LTCFs) have developed rates of MRSA ranging from 25%-35%. MRSA rates may be higher in LTCFs if they are associated with hospitals that have higher rates.13 Transmission of MRSA generally occurs through direct or indirect contact with a reservoir. -

A Review of Chemical Defense in Poison Frogs (Dendrobatidae): Ecology, Pharmacokinetics, and Autoresistance
Chapter 21 A Review of Chemical Defense in Poison Frogs (Dendrobatidae): Ecology, Pharmacokinetics, and Autoresistance Juan C. Santos , Rebecca D. Tarvin , and Lauren A. O’Connell 21.1 Introduction Chemical defense has evolved multiple times in nearly every major group of life, from snakes and insects to bacteria and plants (Mebs 2002 ). However, among land vertebrates, chemical defenses are restricted to a few monophyletic groups (i.e., clades). Most of these are amphibians and snakes, but a few rare origins (e.g., Pitohui birds) have stimulated research on acquired chemical defenses (Dumbacher et al. 1992 ). Selective pressures that lead to defense are usually associated with an organ- ism’s limited ability to escape predation or conspicuous behaviors and phenotypes that increase detectability by predators (e.g., diurnality or mating calls) (Speed and Ruxton 2005 ). Defended organisms frequently evolve warning signals to advertise their defense, a phenomenon known as aposematism (Mappes et al. 2005 ). Warning signals such as conspicuous coloration unambiguously inform predators that there will be a substantial cost if they proceed with attack or consumption of the defended prey (Mappes et al. 2005 ). However, aposematism is likely more complex than the simple pairing of signal and defense, encompassing a series of traits (i.e., the apose- matic syndrome) that alter morphology, physiology, and behavior (Mappes and J. C. Santos (*) Department of Zoology, Biodiversity Research Centre , University of British Columbia , #4200-6270 University Blvd , Vancouver , BC , Canada , V6T 1Z4 e-mail: [email protected] R. D. Tarvin University of Texas at Austin , 2415 Speedway Stop C0990 , Austin , TX 78712 , USA e-mail: [email protected] L. -

Botulinum Toxin Ricin Toxin Staph Enterotoxin B
Botulinum Toxin Ricin Toxin Staph Enterotoxin B Source Source Source Clostridium botulinum, a large gram- Ricinus communis . seeds commonly called .Staphylococcus aureus, a gram-positive cocci positive, spore-forming, anaerobic castor beans bacillus Characteristics Characteristics .Appears as grape-like clusters on Characteristics .Toxin can be disseminated in the form of a Gram stain or as small off-white colonies .Grows anaerobically on Blood Agar and liquid, powder or mist on Blood Agar egg yolk plates .Toxin-producing and non-toxigenic strains Pathogenesis of S. aureus will appear morphologically Pathogenesis .A-chain inactivates ribosomes, identical interrupting protein synthesis .Toxin enters nerve terminals and blocks Pathogenesis release of acetylcholine, blocking .B-chain binds to carbohydrate receptors .Staphylococcus Enterotoxin B (SEB) is a neuro-transmission and resulting in on the cell surface and allows toxin superantigen. Toxin binds to human class muscle paralysis complex to enter cell II MHC molecules causing cytokine Toxicity release and system-wide inflammation Toxicity .Highly toxic by inhalation, ingestion Toxicity .Most lethal of all toxic natural substances and injection .Toxic by inhalation or ingestion .Groups A, B, E (rarely F) cause illness in .Less toxic by ingestion due to digestive humans activity and poor absorption Symptoms .Low dermal toxicity .4-10 h post-ingestion, 3-12 h post-inhalation Symptoms .Flu-like symptoms, fever, chills, .24-36 h (up to 3 d for wound botulism) Symptoms headache, myalgia .Progressive skeletal muscle weakness .18-24 h post exposure .Nausea, vomiting, and diarrhea .Symmetrical descending flaccid paralysis .Fever, cough, chest tightness, dyspnea, .Nonproductive cough, chest pain, .Can be confused with stroke, Guillain- cyanosis, gastroenteritis and necrosis; and dyspnea Barre syndrome or myasthenia gravis death in ~72 h .SEB can cause toxic shock syndrome + + + Gram stain Lipase on Ricin plant Castor beans S.