Nitric Oxide Regulates Vascular Cell Adhesion Molecule 1 Gene
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Genome-Wide Association Study Identifies Seven Novel Loci
Complex traits J Med Genet: first published as 10.1136/jmedgenet-2018-105965 on 19 June 2019. Downloaded from ORIGINAL ARTICLE Genome-wide association study identifies seven novel loci associating with circulating cytokines and cell adhesion molecules in Finns Eeva Sliz, 1,2,3 Marita Kalaoja,1,2,3 Ari Ahola-Olli,4,5 Olli Raitakari,5,6 Markus Perola,7,8,9 Veikko Salomaa,7 Terho Lehtimäki,10 Toni Karhu,3,11 Heimo Viinamäki,12 Marko Salmi,13 Kristiina Santalahti,13 Sirpa Jalkanen,13 Jari Jokelainen,2,14 Sirkka Keinänen-Kiukaanniemi,2,14,15 Minna Männikkö,16 Karl-Heinz Herzig,3,11,17,18 Marjo-Riitta Järvelin,2,3,19,20 Sylvain Sebert,2,3,21 Johannes Kettunen1,2,3 4 ► Additional material is ABSTRact The risk for these diseases increases with age, and published online only. To view Background Inflammatory processes contribute to the due to the world’s ageing population5 their preva- please visit the journal online lence is likely to expand. Moreover, these diseases (http:// dx. doi. org/ 10. 1136/ pathophysiology of multiple chronic conditions. Genetic jmedgenet- 2018- 105965). factors play a crucial role in modulating the inflammatory often co-occur, which is likely due to shared inflam- load, but the exact mechanisms are incompletely mation-related pathophysiology.6 For numbered affiliations see understood. Inflammation is the body’s physiological response end of article. Objective To assess genetic determinants of 16 to harmful stimuli involving multiple molecular and circulating cytokines and cell adhesion molecules cellular interactions attempting to restore distur- Correspondence to bances in tissue or systemic homeostasis. -

Somamer Reagents Generated to Human Proteins Number Somamer Seqid Analyte Name Uniprot ID 1 5227-60
SOMAmer Reagents Generated to Human Proteins The exact content of any pre-specified menu offered by SomaLogic may be altered on an ongoing basis, including the addition of SOMAmer reagents as they are created, and the removal of others if deemed necessary, as we continue to improve the performance of the SOMAscan assay. However, the client will know the exact content at the time of study contracting. SomaLogic reserves the right to alter the menu at any time in its sole discretion. Number SOMAmer SeqID Analyte Name UniProt ID 1 5227-60 [Pyruvate dehydrogenase (acetyl-transferring)] kinase isozyme 1, mitochondrial Q15118 2 14156-33 14-3-3 protein beta/alpha P31946 3 14157-21 14-3-3 protein epsilon P62258 P31946, P62258, P61981, Q04917, 4 4179-57 14-3-3 protein family P27348, P63104, P31947 5 4829-43 14-3-3 protein sigma P31947 6 7625-27 14-3-3 protein theta P27348 7 5858-6 14-3-3 protein zeta/delta P63104 8 4995-16 15-hydroxyprostaglandin dehydrogenase [NAD(+)] P15428 9 4563-61 1-phosphatidylinositol 4,5-bisphosphate phosphodiesterase gamma-1 P19174 10 10361-25 2'-5'-oligoadenylate synthase 1 P00973 11 3898-5 26S proteasome non-ATPase regulatory subunit 7 P51665 12 5230-99 3-hydroxy-3-methylglutaryl-coenzyme A reductase P04035 13 4217-49 3-hydroxyacyl-CoA dehydrogenase type-2 Q99714 14 5861-78 3-hydroxyanthranilate 3,4-dioxygenase P46952 15 4693-72 3-hydroxyisobutyrate dehydrogenase, mitochondrial P31937 16 4460-8 3-phosphoinositide-dependent protein kinase 1 O15530 17 5026-66 40S ribosomal protein S3 P23396 18 5484-63 40S ribosomal protein -

Inflammation-Related Risk Loci in Genome-Wide Association Studies
cells Review Inflammation-Related Risk Loci in Genome-Wide Association Studies of Coronary Artery Disease Carina Mauersberger 1,2 , Heribert Schunkert 1,2 and Hendrik B. Sager 1,2,* 1 Klinik für Kardiologie, Deutsches Herzzentrum München, Technische Universität München, 80636 Munich, Germany; [email protected] (C.M.); [email protected] (H.S.) 2 DZHK (German Centre for Cardiovascular Research), Partner Site Munich Heart Alliance, 80636 Munich, Germany * Correspondence: [email protected] Abstract: Although the importance of inflammation in atherosclerosis is now well established, the exact molecular processes linking inflammation to the development and course of the disease are not sufficiently understood. In this context, modern genetics—as applied by genome-wide association studies (GWAS)—can serve as a comprehensive and unbiased tool for the screening of potentially involved pathways. Indeed, a considerable proportion of loci discovered by GWAS is assumed to affect inflammatory processes. Despite many well-replicated association findings, however, translating genomic hits to specific molecular mechanisms remains challenging. This review provides an overview of the currently most relevant inflammation-related GWAS findings in coronary artery disease and explores their potential clinical perspectives. Keywords: atherosclerosis; coronary artery disease; inflammation; genetics; genome-wide associa- tion studies Citation: Mauersberger, C.; Schunkert, H.; Sager, H.B. Inflammation-Related Risk Loci in Genome-Wide Association Studies of 1. Introduction Coronary Artery Disease. Cells 2021, Atherosclerosis is a complex disorder that evolves over time into clinically manifest- 10, 440. https://doi.org/10.3390/ ing vascular diseases such as carotid or coronary artery disease (CAD), which can lead cells10020440 to potentially lethal complications including stroke and myocardial infarction. -

The Proteomic Analysis of Breast Cell Line Exosomes Reveals Disease Patterns and Potential Biomarkers Yousef Risha1, Zoran Minic2, Shahrokh M
www.nature.com/scientificreports OPEN The proteomic analysis of breast cell line exosomes reveals disease patterns and potential biomarkers Yousef Risha1, Zoran Minic2, Shahrokh M. Ghobadloo3 & Maxim V. Berezovski 1,2,3* Cancer cells release small extracellular vesicles, exosomes, that have been shown to contribute to various aspects of cancer development and progression. Diferential analysis of exosomal proteomes from cancerous and non-tumorigenic breast cell lines can provide valuable information related to breast cancer progression and metastasis. Moreover, such a comparison can be explored to fnd potentially new protein biomarkers for early disease detection. In this study, exosomal proteomes of MDA-MB-231, a metastatic breast cancer cell line, and MCF-10A, a non-cancerous epithelial breast cell line, were identifed by nano-liquid chromatography coupled to tandem mass spectrometry. We also tested three exosomes isolation methods (ExoQuick, Ultracentrifugation (UC), and Ultrafltration– Ultracentrifugation) and detergents (n-dodecyl β-d-maltoside, Triton X-100, and Digitonin) for solubilization of exosomal proteins and enhanced detection by mass spectrometry. A total of 1,107 exosomal proteins were identifed in both cell lines, 726 of which were unique to the MDA-MB-231 breast cancer cell line. Among them, 87 proteins were predicted to be relevant to breast cancer and 16 proteins to cancer metastasis. Three exosomal membrane/surface proteins, glucose transporter 1 (GLUT-1), glypican 1 (GPC-1), and disintegrin and metalloproteinase domain-containing protein 10 (ADAM10), were identifed as potential breast cancer biomarkers and validated with Western blotting and high-resolution fow cytometry. We demonstrated that exosomes are a rich source of breast cancer-related proteins and surface biomarkers that may be used for disease diagnosis and prognosis. -

Regulation Pathway of Mesenchymal Stem Cell Immune Dendritic Cell
Downloaded from http://www.jimmunol.org/ by guest on September 26, 2021 is online at: average * The Journal of Immunology , 13 of which you can access for free at: 2010; 185:5102-5110; Prepublished online 1 from submission to initial decision 4 weeks from acceptance to publication October 2010; doi: 10.4049/jimmunol.1001332 http://www.jimmunol.org/content/185/9/5102 Inhibition of Immune Synapse by Altered Dendritic Cell Actin Distribution: A New Pathway of Mesenchymal Stem Cell Immune Regulation Alessandra Aldinucci, Lisa Rizzetto, Laura Pieri, Daniele Nosi, Paolo Romagnoli, Tiziana Biagioli, Benedetta Mazzanti, Riccardo Saccardi, Luca Beltrame, Luca Massacesi, Duccio Cavalieri and Clara Ballerini J Immunol cites 38 articles Submit online. Every submission reviewed by practicing scientists ? is published twice each month by Submit copyright permission requests at: http://www.aai.org/About/Publications/JI/copyright.html Receive free email-alerts when new articles cite this article. Sign up at: http://jimmunol.org/alerts http://jimmunol.org/subscription http://www.jimmunol.org/content/suppl/2010/10/01/jimmunol.100133 2.DC1 This article http://www.jimmunol.org/content/185/9/5102.full#ref-list-1 Information about subscribing to The JI No Triage! Fast Publication! Rapid Reviews! 30 days* Why • • • Material References Permissions Email Alerts Subscription Supplementary The Journal of Immunology The American Association of Immunologists, Inc., 1451 Rockville Pike, Suite 650, Rockville, MD 20852 Copyright © 2010 by The American Association of -

Thousands of Cpgs Show DNA Methylation Differences in ACPA-Positive Individuals
G C A T T A C G G C A T genes Article Thousands of CpGs Show DNA Methylation Differences in ACPA-Positive Individuals Yixiao Zeng 1,2, Kaiqiong Zhao 2,3, Kathleen Oros Klein 2, Xiaojian Shao 4, Marvin J. Fritzler 5, Marie Hudson 2,6,7, Inés Colmegna 6,8, Tomi Pastinen 9,10, Sasha Bernatsky 6,8 and Celia M. T. Greenwood 1,2,3,9,11,* 1 PhD Program in Quantitative Life Sciences, Interfaculty Studies, McGill University, Montréal, QC H3A 1E3, Canada; [email protected] 2 Lady Davis Institute for Medical Research, Jewish General Hospital, Montréal, QC H3T 1E2, Canada; [email protected] (K.Z.); [email protected] (K.O.K.); [email protected] (M.H.) 3 Department of Epidemiology, Biostatistics and Occupational Health, McGill University, Montréal, QC H3A 1A2, Canada 4 Digital Technologies Research Centre, National Research Council Canada, Ottawa, ON K1A 0R6, Canada; [email protected] 5 Cumming School of Medicine, University of Calgary, Calgary, AB T2N 1N4, Canada; [email protected] 6 Department of Medicine, McGill University, Montréal, QC H4A 3J1, Canada; [email protected] (I.C.); [email protected] (S.B.) 7 Division of Rheumatology, Jewish General Hospital, Montréal, QC H3T 1E2, Canada 8 Division of Rheumatology, McGill University, Montréal, QC H3G 1A4, Canada 9 Department of Human Genetics, McGill University, Montréal, QC H3A 0C7, Canada; [email protected] 10 Center for Pediatric Genomic Medicine, Children’s Mercy, Kansas City, MO 64108, USA 11 Gerald Bronfman Department of Oncology, McGill University, Montréal, QC H4A 3T2, Canada * Correspondence: [email protected] Citation: Zeng, Y.; Zhao, K.; Oros Abstract: High levels of anti-citrullinated protein antibodies (ACPA) are often observed prior to Klein, K.; Shao, X.; Fritzler, M.J.; Hudson, M.; Colmegna, I.; Pastinen, a diagnosis of rheumatoid arthritis (RA). -

Gene Structure, Chromosomal Location, and Basis for Alternative Mrna Splicing of the Human VCAMI Gene (Vascular Cell Adhesion Molecule 1/Endotheial Cell) MYRON 1
Proc. Nati. Acad. Sci. USA Vol. 88, pp. 7859-7863, September 1991 Biochemistry Gene structure, chromosomal location, and basis for alternative mRNA splicing of the human VCAMI gene (vascular cell adhesion molecule 1/endotheial cell) MYRON 1. CYBULSKY*, JOCHEN W. U. FRIES*, AMY J. WILLIAMS*, PARVEZ SULTAN*, ROGER EDDYt, MARY BYERSt, THOMAS SHOWSt, MICHAEL A. GIMBRONE, JR.*, AND TUCKER COLLINS*: *Vascular Research Division, Department of Pathology, Brigham and Women's Hospital and Harvard Medical School, Boston, MA 02115; and tDepartment of Human Genetics, Roswell Park Memorial Institute, Buffalo, NY 14163 Communicated by Vincent T. Marchesi, June 13, 1991 ABSTRACT Vascular cell adhesion molecule 1 (VCAM-1) from activated cultured human umbilical vein endothelial is a cell surface glycoprotein adhesive for certain blood leuko- cells was reported to contain six extracellular C2 or H-type cytes and tumor cels, which is ex by activated endothe- immunoglobulin-like domains (3). However, cDNAs were lium in a variety of pthog conditions ncl og atheroscle- isolated from cytokine-activated endothelium that contains rosis. Genomic clones encoding the VCAMI gene were isoated an additional immunoglobulin domain, designated AS-1 or and the organization of the gene was d d . The gene, domain 4 (the remaining domains were designated 5-7) (11, which is present in a single copy in the human genome, contains 12). This additional immunoglobulin domain is most homol- 9 exons nning =25 kiobas of DNA. Exons 2-8 contain C2 ogous to domain 1, the existing N-terminal domain. Both or H-type nunoglobulin domains. At least two different transcript forms of VCAM-1 were detected in interleukin 1,8 VCAM-1 precursors can be generated frou the human gene as (IL-103)-stimulated human umbilical vein endothelial cells, a result of alternative mRNA spicng events, which include or although the seven-domain form appeared predominant (11, exclude exon 5. -

Intercellular Adhesion Molecule-1: a Protective Haplotype Against Multiple Sclerosis
Genes and Immunity (2003) 4, 518–523 & 2003 Nature Publishing Group All rights reserved 1466-4879/03 $25.00 www.nature.com/gene BRIEF COMMUNICATION Intercellular adhesion molecule-1: a protective haplotype against multiple sclerosis I Cournu-Rebeix1,EGe´nin2, G Lesca1, A Azoulay-Cayla3, N Tubridy1, E Noe´1, M Clanet4, G Edan5, F Clerget-Darpoux2,GSe´mana6 and B Fontaine1,3 1Laboratoire des affections de la mye´line et des canaux ioniques musculaires-INSERM U546, Faculte´ de Me´decine Pitie´-Salpeˆtrie`re, Paris, France; 2INSERM U535, Centre Hospitalier Universitaire, Le Kremlin Biceˆtre, France; 3Fe´de´ration de Neurologie, Groupe Hospitalier Pitie´-Salpeˆtrie`re, Paris, France; 4Service de Neurologie, Centre Re´gional Hospitalier Universitaire Purpan, Toulouse, France; 5Service de Neurologie, Centre Re´gional Hospitalier Universitaire Pontchaillou, Rennes, France; 6Laboratoire d’Immunoge´ne´tique, Etablissement Franc¸ais du Sang Bretagne et Laboratoire d’Immunologie (UPRES EA 1257), Centre Hospitalier Re´gional Universitaire et Faculte´ de Me´decine, Rennes, France Intercellular adhesion molecule-1 (ICAM-1) and its receptors are adhesion molecules that play a key role in the transmigration of inflammatory cells through the blood–brain barrier, one of the earliest events in multiple sclerosis (MS), which leads to demyelination in the central nervous system. To investigate the role of genes encoding ICAM-1 and its receptors, we used a strategy of genetic linkage and association in 439 case–parent MS families of French origin, well characterized according to HLA status and severity. We demonstrate that the genes encoding ICAM-1 receptors do not influence MS susceptibility or severity. ICAM-1 had a modest, but significant effect on MS genetic susceptibility, independent of HLA and disease severity. -

The Role of Cell Adhesion Molecule 1 (CADM1) in Cutaneous Malignancies
International Journal of Molecular Sciences Review The Role of Cell Adhesion Molecule 1 (CADM1) in Cutaneous Malignancies Yu Sawada *, Emi Mashima, Natsuko Saito-Sasaki and Motonobu Nakamura Department of Dermatology, University of Occupational and Environmental Health, 1-1 Iseigaoka, Yahatanishi-ku, Kitakyushu 807-8555, Japan; [email protected] (E.M.); [email protected] (N.S.-S.); [email protected] (M.N.) * Correspondence: [email protected]; Tel.: +81-093-691-7445 Received: 19 November 2020; Accepted: 16 December 2020; Published: 20 December 2020 Abstract: Cell adhesion ability is one of the components to establish cell organization and shows a great contribution to human body construction consisting of various types of cells mixture to orchestrate tissue specific function. The cell adhesion molecule 1 (CADM1) is a molecule of cell adhesion with multiple functions and has been identified as a tumor suppressor gene. CADM1 has multifunctions on the pathogenesis of malignancies, and other normal cells such as immune cells. However, little is known about the function of CADM1 on cutaneous cells and cutaneous malignancies. CADM1 plays an important role in connecting cells with each other, contacting cells to deliver their signal, and acting as a scaffolding molecule for other immune cells to develop their immune responses. A limited number of studies reveal the contribution of CADM1 on the development of cutaneous malignancies. Solid cutaneous malignancies, such as cutaneous squamous cell carcinoma and malignant melanoma, reduce their CADM1 expression to promote the invasion and metastasis of the tumor. On the contrary to these cutaneous solid tumors except for Merkel cell carcinoma, cutaneous lymphomas, such as adult-T cell leukemia/lymphoma, mycosis fungoides, and Sézary syndrome, increase their CADM1 expression for the development of tumor environment. -

Molecule-1 Promoter the Platelet Endothelial Cell Adhesion B Site In
Identification of a Functional NF-κB Site in the Platelet Endothelial Cell Adhesion Molecule-1 Promoter This information is current as Luisa M. Botella, Amaya Puig-Kröger, Nuria Almendro, of September 26, 2021. Tilman Sánchez-Elsner, Eduardo Muñoz, Angel Corbí and Carmelo Bernabéu J Immunol 2000; 164:1372-1378; ; doi: 10.4049/jimmunol.164.3.1372 http://www.jimmunol.org/content/164/3/1372 Downloaded from References This article cites 35 articles, 17 of which you can access for free at: http://www.jimmunol.org/content/164/3/1372.full#ref-list-1 http://www.jimmunol.org/ Why The JI? Submit online. • Rapid Reviews! 30 days* from submission to initial decision • No Triage! Every submission reviewed by practicing scientists • Fast Publication! 4 weeks from acceptance to publication by guest on September 26, 2021 *average Subscription Information about subscribing to The Journal of Immunology is online at: http://jimmunol.org/subscription Permissions Submit copyright permission requests at: http://www.aai.org/About/Publications/JI/copyright.html Email Alerts Receive free email-alerts when new articles cite this article. Sign up at: http://jimmunol.org/alerts The Journal of Immunology is published twice each month by The American Association of Immunologists, Inc., 1451 Rockville Pike, Suite 650, Rockville, MD 20852 Copyright © 2000 by The American Association of Immunologists All rights reserved. Print ISSN: 0022-1767 Online ISSN: 1550-6606. Identification of a Functional NF-B Site in the Platelet Endothelial Cell Adhesion Molecule-1 Promoter1 Luisa M. Botella,2,3* Amaya Puig-Kro¨ger,3* Nuria Almendro,* Tilman Sa´nchez-Elsner,* Eduardo Mun˜oz,† Angel Corbı´,* and Carmelo Bernabe´u* Platelet endothelial cell adhesion molecule-1 (PECAM-1) is a type I transmembrane adhesion protein of 130 kDa that belongs to a subgroup of the Ig gene superfamily, characterized by the presence of immunoreceptor tyrosine-based inhibitory motifs. -
Name Aliases Binding Partner Physiology / Oncology References
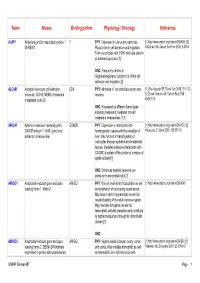
Name Aliases Binding partner Physiology / Oncology References AJAP1 Adherens junction associated protein 1, ? PHY : Expressed in uterus and pancreas. [1] http://www.uniprot.org/uniprot/Q9UKB5. [2] SHREW1 Plays a role in cell adhesion and migration. McDonald JM, Cancer Biol Ther 2006, 5:300-4 Forms a complex with CDH1 and beta-catenin at adherens junctions [1] ONC : Frequently deleted in oligodendrogliomas, functions to inhibit cell adhesion and migration [2] ALCAM Activated leukocyte cell adhesion CD6 PHY : Adhesion of activated leukocytes and [1] Ofori-Acquah SF, Transl Res 2008, 151:122- molecule, CD166, MEMD (melanoma neurons 8. [2] van Kilsdonk JW, Cancer Res 2008, metastasis clone D) 68:3671-9 ONC : Expressed by different tumor types including melanoma; mediates cancer/ melanoma invasiveness [1,2] AMICA1 Adhesion molecule interacting with CXADR PHY : Expression is restricted to the [1] http://www.uniprot.org/uniprot/Q86YT9. [2] CXADR antigen 1, JAML (junctional hematopoietic tissues with the exception of Moog-Lutz C, Blood 2003, 102:3371-8 adhesion molecule-like) liver. May function in transmigration of leukocytes through epithelial and endothelial tissues. Mediates adhesive interactions with CXADR, a protein of the junctional complex of epithelial cells [1] ONC : Enhances myeloid leukemia cell adhesion to endothelial cells [2] AMIGO1 Amphoterin-induced gene and open AMIGO PHY : May be involved in fasciculation as well [1] http://www.uniprot.org/uniprot/Q86WK6 reading frame 1, Alivin-2 as myelination of developing neural axons. May have a role in regeneration as well as neural plasticity in the adult nervous system. May mediate homophilic as well as heterophilic cell-cell interaction and contribute to signal transduction through its intracellular domain [1] ONC : - AMIGO2 Amphoterin-induced gene and open AMIGO PHY : Highest levels in breast, ovary, cervix, [1] http://www.uniprot.org/uniprot/Q86SJ2. -
Adhesion Molecule 1 by Tumor Necrosis Factor a Is Mediated by NF-KB Proteins (Transcription Regulation) MASAHIRO TAKEUCHI* and VIJAY R
Proc. Natl. Acad. Sci. USA Vol. 92, pp. 3561-3565, April 1995 Biochemistry Induction of the gene encoding mucosal vascular addressin cell adhesion molecule 1 by tumor necrosis factor a is mediated by NF-KB proteins (transcription regulation) MASAHIRO TAKEUCHI* AND VIJAY R. BAICHWALt# *Yamanouchi Pharmaceutical Co., Ltd., 21 Miyukigaoka, Tsukuba, Ibaraki, 305, Japan; and tTularik, Inc., 270 East Grand Avenue, South San Francisco, CA 94080 Communicated by David V. Goeddel, Tularik Inc., South San Francisco, CA, December 21, 1994 (received for review December 1, 1994) ABSTRACT Mucosal vascular addressin cell adhesion Butcher, unpublished work). To investigate the mechanism of molecule 1 (MAdCAM-1) is involved in trafficking of lym- TNF-a-induced expression of MAdCAM-1 in bEnd.3 cells and phocytes to mucosal endothelium. Expression of MAdCAM-1 the role of the NF-KB sites, we conducted mutational analysis is induced in the murine endothelial cell line bEnd.3 by tumor of the promoter region and DNA-binding experiments with necrosis factor a (TNF-a), interleukin 1, and bacterial lipo- cell extracts from cells stimulated with TNF-a. The data show polysaccharide. Here we show that TNF-a enhances expres- that TNF-a induction of MAdCAM-1 gene expression in sion of a firefly luciferase reporter directed by the MAd- bEnd.3 cells is mediated primarily by the p65 member of the CAM-1 promoter, confirming transcriptional regulation of NF-KB family. MAdCAM-1. Mutational analysis of the promoter indicates that a DNA fragment extending from nt -132 to nt +6 of the MATERIALS AND METHODS gene is sufficient for TNF-a inducibility.