Available Online at ISSN NO
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

ICD-10 Diagnoses on Router
L ARTHRITIS R L HAND R L ANKLE R L FRACTURES R OSTEOARTHRITIS: PRIMARY, 2°, POST TRAUMA, POST _____ CONTUSION ACHILLES TEN DYSFUNCTION/TENDINITIS/RUPTURE FLXR TEN CLAVICLE: STERNAL END, SHAFT, ACROMIAL END CRYSTALLINE ARTHRITIS: GOUT: IDIOPATHIC, LEAD, CRUSH INJURY AMPUTATION TRAUMATIC LEVEL SCAPULA: ACROMION, BODY, CORACOID, GLENOID DRUG, RENAL, OTHER DUPUYTREN’S CONTUSION PROXIMAL HUMERUS: SURGICAL NECK 2 PART 3 PART 4 PART CRYSTALLINE ARTHRITIS: PSEUDOGOUT: HYDROXY LACERATION: DESCRIBE STRUCTURE CRUSH INJURY PROXIMAL HUMERUS: GREATER TUBEROSITY, LESSER TUBEROSITY DEP DIS, CHONDROCALCINOSIS LIGAMENT DISORDERS EFFUSION HUMERAL SHAFT INFLAMMATORY: RA: SEROPOSITIVE, SERONEGATIVE, JUVENILE OSTEOARTHRITIS PRIMARY/SECONDARY TYPE _____ LOOSE BODY HUMERUS DISTAL: SUPRACONDYLAR INTERCONDYLAR REACTIVE: SECONDARY TO: INFECTION ELSEWHERE, EXTENSION OR NONE INTESTINAL BYPASS, POST DYSENTERIC, POST IMMUNIZATION PAIN OCD TALUS HUMERUS DISTAL: TRANSCONDYLAR NEUROPATHIC CHARCOT SPRAIN HAND: JOINT? OSTEOARTHRITIS PRIMARY/SECONDARY TYPE _____ HUMERUS DISTAL: EPICONDYLE LATERAL OR MEDIAL AVULSION INFECT: PYOGENIC: STAPH, STREP, PNEUMO, OTHER BACT TENDON RUPTURES: EXTENSOR OR FLEXOR PAIN HUMERUS DISTAL: CONDYLE MEDIAL OR LATERAL INFECTIOUS: NONPYOGENIC: LYME, GONOCOCCAL, TB TENOSYNOVITIS SPRAIN, ANKLE, CALCANEOFIBULAR ELBOW: RADIUS: HEAD NECK OSTEONECROSIS: IDIOPATHIC, DRUG INDUCED, SPRAIN, ANKLE, DELTOID POST TRAUMATIC, OTHER CAUSE SPRAIN, ANKLE, TIB-FIB LIGAMENT (HIGH ANKLE) ELBOW: OLECRANON WITH OR WITHOUT INTRA ARTICULAR EXTENSION SUBLUXATION OF ANKLE, -

Pes Anserine Bursitis
BRIGHAM AND WOMEN’S HOSPITAL Department of Rehabilitation Services Physical Therapy Standard of Care: Pes Anserine Bursitis ICD 9 Codes: 726.61 Case Type / Diagnosis: The pes anserine bursa lies behind the medial hamstring, which is composed of the tendons of the sartorius, gracilis and semitendinosus (SGT) muscles. Because these 3 tendons splay out on the anterior aspect of the tibia and give the appearance of the foot of a goose, pes anserine bursitis is also known as goosefoot bursitis.1 These muscles provide for medial stabilization of the knee by acting as a restraint to excessive valgus opening. They also provide a counter-rotary torque function to the knee joint. The pes anserine has an eccentric role during the screw-home mechanism that dampens the effect of excessively forceful lateral rotation that may accompany terminal knee extension.2 Pes anserine bursitis presents as pain, tenderness and swelling over the anteromedial aspect of the knee, 4 to 5 cm below the joint line.3 Pain increases with knee flexion, exercise and/or stair climbing. Inflammation of this bursa is common in overweight, middle-aged women, and may be associated with osteoarthritis of the knee. It also occurs in athletes engaged in activities such as running, basketball, and racquet sports.3 Other risk factors include: 1 • Incorrect training techniques, or changes in terrain and/or distanced run • Lack of flexibility in hamstring muscles • Lack of knee extension • Patellar malalignment Indications for Treatment: • Knee Pain • Knee edema • Decreased active and /or passive ROM of lower extremities • Biomechanical dysfunction lower extremities • Muscle imbalances • Impaired muscle performance (focal weakness or general conditioning) • Impaired function Contraindications: • Patients with active signs/symptoms of infection (fever, chills, prolonged and obvious redness or swelling at hip joint). -

Hughston Health Alert US POSTAGE PAID the Hughston Foundation, Inc
HughstonHughston HealthHealth AlertAlert 6262 Veterans Parkway, PO Box 9517, Columbus, GA 31908-9517 • www.hughston.com/hha VOLUME 24, NUMBER 3 - SUMMER 2012 Normal knee anatomy Fig. 1. Anterior knee Inside... pain can be caused by patellofemoral syndrome, • Orthopaedic Components: Quadriceps often called “cyclist’s knee,” muscle What makes a total knee implant? or by patellar tendinitis. • Tennis and Back Pain • Glucosamine and Chondroitin Femur • New Heat Policies - Summer 2012 Patella (kneecap) Imbalances in strength and • Hughston Clinic tone of the lower body Patellar can result in excessive tendon Fibula compressive forces Tibia across the joint. (shinbone) Cycling Overuse Injuries of the Knee Patellofemoral syndrome Compression and shearing across the cartilage of the Quadriceps The economy and higher gas prices are patella can lead to loss of muscle straining wallets and making cycling a more cartilage and the beginning attractive mode of transportation. Health of arthritis. Calf enthusiasts use cycling as a low-impact muscles exercise to improve overall fitness and Patella minimize knee pain. Cities throughout the (kneecap) country are turning old, abandoned railroad Damaged lines into miles of beautiful biking trails and cartilage Femur adding bike lanes to existing roads. In essence, Trochlear cycling is becoming one of the nation’s most groove popular pastimes. Patellar tendinitis Cycling has many health benefits; you Front Quadriceps Cross section of can tone your muscles, improve your view muscle a bent knee cardiovascular fitness, and burn as many as of bent 300 calories an hour during a steady ride. knee People often turn to cycling as a form of Fibula Femur exercise and enjoyment because it is a low- Tibia (thighbone) impact exercise that is easy on the knees. -

Imaging of the Bursae
Editor-in-Chief: Vikram S. Dogra, MD OPEN ACCESS Department of Imaging Sciences, University of HTML format Rochester Medical Center, Rochester, USA Journal of Clinical Imaging Science For entire Editorial Board visit : www.clinicalimagingscience.org/editorialboard.asp www.clinicalimagingscience.org PICTORIAL ESSAY Imaging of the Bursae Zameer Hirji, Jaspal S Hunjun, Hema N Choudur Department of Radiology, McMaster University, Canada Address for correspondence: Dr. Zameer Hirji, ABSTRACT Department of Radiology, McMaster University Medical Centre, 1200 When assessing joints with various imaging modalities, it is important to focus on Main Street West, Hamilton, Ontario the extraarticular soft tissues that may clinically mimic joint pathology. One such Canada L8N 3Z5 E-mail: [email protected] extraarticular structure is the bursa. Bursitis can clinically be misdiagnosed as joint-, tendon- or muscle-related pain. Pathological processes are often a result of inflammation that is secondary to excessive local friction, infection, arthritides or direct trauma. It is therefore important to understand the anatomy and pathology of the common bursae in the appendicular skeleton. The purpose of this pictorial essay is to characterize the clinically relevant bursae in the appendicular skeleton using diagrams and corresponding multimodality images, focusing on normal anatomy and common pathological processes that affect them. The aim is to familiarize Received : 13-03-2011 radiologists with the radiological features of bursitis. Accepted : 27-03-2011 Key words: Bursae, computed tomography, imaging, interventions, magnetic Published : 02-05-2011 resonance, ultrasound DOI : 10.4103/2156-7514.80374 INTRODUCTION from the adjacent joint. The walls of the bursa thicken as the bursal inflammation becomes longstanding. -

Diagnosing & Treating Non-Traumatic Knee Pain
ORTHOPEDIC PRIMARY CARE: Diagnosing & Treating Non-Traumatic Knee Pain © Jackson Orthopaedic Foundation www.jacksonortho.org Acknowledgement This lecture was originally developed as part of Orthopedic Primary Care, a six-month continuing education program presented yearly by the Jackson Orthopaedic Foundation, a non-profit organization in Oakland, California. More information at: OrthoPrimaryCare.Info www.jacksonortho.org Disclosure Statement of Unapproved/Investigative Use • This presentation contains no discussion of the unapproved/investigative use of any commercial product or device. www.jacksonortho.org Disclosure Statement of Financial Interest Neither Dr. Benham nor Dr. Geier has any financial interests/arrangements or affiliations with one or more organizations that could be perceived to have real or apparent conflicts of interest in the context of the subject of this presentation. www.jacksonortho.org Learning Objectives • At the conclusion of this presentation, participants will be able to 1. Identify likely causes of non-traumatic, non-arthritic knee pain based on presentation and history. 2. Appropriately apply specialty exam techniques and order diagnostic imaging as needed to definitively diagnose non-traumatic, non-arthritic knee pain. 3. Implement appropriate treatment plans to include integrative and pharmaceutical modalities. The use and effects of the following pharmaceutical types will be discussed: acetaminophen, NSAIDs, injectable corticosteroids and topical analgesics. www.jacksonortho.org Learning Objectives • At the conclusion of this presentation, participants will be able to 1. Identify likely causes of non-traumatic, non-arthritic knee pain based on presentation and history. 2. Appropriately apply specialty exam techniques and order diagnostic imaging as needed to definitively diagnose non-traumatic, non-arthritic knee pain. -

Keep Your Joint. Stop Your Pain. T
P A T I E N T RESOURCES KEEP YOUR JOINT. STOP YOUR PAIN. T A I N T R O T O M U S C U L O S K E L E T A L B A (01) T E N D O N I T I S / B U R S I T I S O F T H E H I P L E O G R E A T E R T R O C H A N T E R I C F B U R S I T I S C 02 O N T 03 I L L I O P S O A S B U R S I T I S E N T S 04 S A C R O I L I T I S I N T R O T P M U S C U L O S K E L E T A L B (05) T E N D O N I T I S / B U R S I T I S O F K N E E 06 P E S A N S E R I N E B U R S I T I S 07 S U P R A P A T E L L A R B U R S I T I S I L L I O T I B I A L B A N D 08 S Y N D R O M E 09 P A T E L L A R T E N D I N I T I S I N T R O T P M U S C U L O S K E L E T A L C (10) T E N D O N I T I S / B U R S I T I S O F S H O U L D E R S U B A C R O M I N A L B U R S I T I S A ( I M P I N G E M E N T S Y N D R O M E ) R 11 O M B I C E P S T E N D I N I T I S O 12 T I O F R O Z E N S H O U L D E R N 13 ( A D H E S I V E C A P S U L I T I S ) 01 MUSCULOSKELETAL TENDONITIS/BURSITIS OF THE HIP When the pain stops abruptly the muscles and ligaments will respond to the sudden shifting in the swing of You recently had a procedure the joint and this will create pain, performed and are surely feeling soreness and even tendonitis and changes to the pain and function of bursitis. -

Outline Knee Anatomy
8/7/2013 Physical Exam Skills and Outline Office Procedures in Orthopaedics • Knee exam • Knee aspiration and injection • Shoulder exam • Subacromial bursa injection UCSF Essentials of Primary Care August 14, 2012 Carlin Senter, M.D. The quadriceps muscles extend the knee Knee Anatomy http://thefitcoach.wordpress.com/2012/04/07/267/ http://scientia.wikispaces.com/Thigh+and +Leg+-+Lecture+Notes 1 8/7/2013 The quadriceps muscles merge to form the quadriceps tendon… patellar tendon The hamstrings flex the knee www.hep2go.com Pes anserine bursa There are 4 main ligaments in the knee http://meded.ucsd.edu/clinicalmed/joints.htm 2 8/7/2013 Meniscus Knee exam Common Causes of Knee Pain by Location of Musculoskeletal work-up Symptoms • Anterior: • Medial • History - Patellofemoral syndrome - Medial joint-line: meniscus tear or OA - Quadriceps tendinitis - MCL sprain • Inspection - Patellar tendinitis - Pes anserine bursitis P • Lateral: • Posterior • alpation - Lateral jointline: meniscus tear - Hamstring tendinitis or OA - Gastrocnemius strain - IT band syndrome • Range of motion - OA, meniscus tears, - LCL sprain (rare) effusion, popliteal cyst…. - Fibular head: fracture (rare) • Other Tests 3 8/7/2013 Palpation of joint line Inspection seated or supine http://www.rheumors.com/kneeexam/palpation.html http://doctorhoang.wordpress.com/20 http://meded.ucsd.edu/cl 10/09/06/valgus-knee-and-bunion/ inicalmed/joints.htm Palpation of patella - supine Palpation of patellar facet Ballottement 4 8/7/2013 Knee range of motion Other Tests: Lachman to evaluate ACL Sensitivity 75-100% Specificity 95-100% • ROM: normal 0-135 – Determine if knee is locking or if ROM is limited due to effusion – Locking: think bucket handle meniscus. -

Anserine Syndrome
Artigo de revisÃO A síndrome anserina Milton Helfenstein Jr1 e Jorge Kuromoto2 RESUMO Dor no joelho é uma condição comum na clínica diária e a patologia anserina, também conhecida como pata de ganso, tem sido considerada uma das principais causas. O diagnóstico tem sido realizado de maneira eminentemente clínica, o que tem gerado equívocos. Os pacientes queixam-se tipicamente de dor na parte medial do joelho, com sensibilidade na porção ínferomedial. Estudos de imagem têm sido realizados para esclarecer se tais pacientes possuem bursite, tendinite ou ambos os distúrbios na região conhecida como pata de ganso. Entretanto, o defeito estrutural responsável pelos sintomas permanece desconhecido, motivo pelo qual preferimos intitular como “Síndrome Anserina”. O diabetes mellitus é um fator predisponente bem reconhecido. O sobrepeso e a osteoartrite de joelho parecem ser fatores adicionais de risco, contudo, seus papéis na gênese da moléstia ainda não são bem entendidos. O tratamento atual inclui anti-inflamatório, fisioterapia e infiltração de corticoide, com evolução muito variável, que oscila entre 10 dias e 36 meses. A falta de conhecimento sobre a etiofisiopatologia e dados epidemiológicos exige futuros estudos para esse frequente e intrigante distúrbio. Palavras-chave: bursite anserina, tendinite da pata de ganso, síndrome da bursite/tendinite anserina, pata de ganso. INTRODUÇÃO A síndrome tem sido evidenciada em atletas corredores de longa distância.3 O diabetes mellitus (DM) tem sido identifi- A inserção combinada dos tendões dos músculos sartório, grácil cado em uma substancial proporção desses pacientes.4 Casos e semitendinoso, a cerca de 5 cm distalmente da porção medial considerados como bursite crônica foram documentados em da articulação do joelho, forma uma estrutura que se assemelha artrite reumatoide e em osteoartrite.5,6 à membrana natatória do ganso, razão pela qual os anatomistas A etiologia também inclui trauma, retração da musculatura a denominaram de “pata de ganso”, ou, do latim, pes anserinus. -
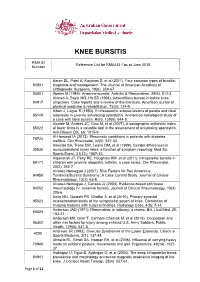
Reference List for RMA431-1As at June 2018 Number
KNEE BURSITIS RMA ID Reference List for RMA431-1as at June 2018 Number Aaron DL, Patel A, Kayiaros S, et al (2011). Four common types of bursitis: 84931 diagnosis and management. The Journal of American Academy of Orthopaedic Surgeons, 19(6): 359-67. 85001 Abeles M (1986). Anserine bursitis. Arthritis & Rheumatism, 29(6): 812-3. Ahmed A, Bayol MG, Ha SB (1994). Adventitious bursae in below knee 84917 amputees. Case reports and a review of the literature. American journal of physical medicine & rehabilitation, 73(2): 124-9. Albert J, Lagier R (1983). Enthesopathic erosive lesions of patella and tibial 85148 tuberosity in juvenile ankylosing spondylitis. Anatomico-radiological study of a case with tibial bursitis. Rofo, 139(5): 544-8. Alcalde M, Acebes JC, Cruz M, et al (2007). A sonographic enthesitic index 85022 of lower limbs is a valuable tool in the assessment of ankylosing spondylitis. Ann Rheum Dis, 66: 1015-9. Al-Homood IA (2013). Rheumatic conditions in patients with diabetes 78722 mellitus. Clin Rheumatol, 32(5): 527-33. Almeida SA, Trone DW, Leone DM, et al (1999). Gender differences in 39530 musculoskeletal injury rates: a function of symptom reporting. Med Sci Sports Exerc, 31(12): 1807-12. Alqanatish JT, Petty RE, Houghton KM, et al (2011). Infrapatellar bursitis in 85171 children with juvenile idiopathic arthritis: a case series. Clin Rheumatol, 30(2): 263-7. Alvarez-Nemegyei J (2007). Risk Factors for Pes Anserinus 84950 Tendinitis/Bursitis Syndrome: A Case Control Study. Journal of Clinical Rheumatology, 13(2): 63-5. Alvarez-Nemegyei J, Canoso JJ (2004). Evidence-based soft tissue 84552 rheumatology IV: anserine bursitis. -

Pes Anserine Bursitis
A Patient's Guide to Pes Anserine Bursitis Introduction around from the back of the leg to the front. It inserts into the medial surface of the tibia and Bursitis of the knee occurs when constant deep connective tissue of the lower leg. Medial friction on the bursa causes inflammation. refers to the inside of the knee or the side The bursa is a small sac that cushions the closest to the other knee. bone from tendons that rub over the bone. Bursae can also protect other tendons as Just above the insertion of the semitendinosus tissues glide over one another. Bursae can tendon is the gracilis tendon. The gracilis become inflamed and irritated causing pain muscle adducts or moves the leg toward the and tenderness. body. The semitendinosus tendon is also just behind the attachment of the sartorius muscle. This guide will help you understand The sartorius muscle bends and externally • what part of the knee is affected rotates the hip. Together, these three tendons • what causes this condition splay out on the tibia and look like a goose- • how the doctors diagnosis this condition foot. This area is called the pes anserine or pes • what treatment options are available anserinus. Anatomy What parts of the knee are affected? The pes anserine bursa is the main area affected by this condition. The pes anserine bursa is a small lubricating sac between the tibia (shinbone) and the hamstring muscle. The hamstring muscle is located along the back of the thigh. There are three tendons of the hamstring: the semitendinosus, semimembranosus, and the biceps femoris. -

Your Template!
2019 UCSF Primary Care Medicine Principles and Practice Management of Common Problems in Sports Medicine Cindy J. Chang, M.D. Clinical Professor, Primary Care Sports Medicine Depts. of Orthopaedics and Family & Community Medicine Past President, American Medical Society for Sports Medicine Board of Trustees, American College of Sports Medicine Disclosure ▪ I have no conflict of interest in relation to this presentation ▪ Ossur Americas: independent lectures on osteoarthritis ▪ NeuroSlam: scientific advisor ▪ Agency for Student Health Research: medical advisory board 2 Cindy J. Chang M.D. 1 | [footer text here] Objective ▪ Review common problems in sports medicine ▪ Understand basic anatomy of the musculoskeletal system and its clinical correlation to injuries 3 Cindy J. Chang M.D. History (MS OLDCARTS vs OPQRST) ▪ Mechanism ▪ Symptoms ▪ Onset (O) – date of injury ▪ Location – point to where the pain is ▪ Duration – acute or chronic ▪ Character (Q) – burning, sharp, dull, achy ▪ Aggravating/Alleviating (P) – provokes/palliates ▪ Radiation (R) – come from or go anywhere else ▪ Timing (T) – constant, at night, with activity ▪ Severity (S) – grade pain https://meded.ucsd.edu/clinicalmed/history.htm 4 Cindy J. Chang M.D. 2 | [footer text here] Case - Elbow Pain ▪ Your patient is a 36 yo female recreational tennis player with elbow pain radiating down the posterior aspect of her forearm that has increased over the past two days. She recently began playing tennis on a USTA team that practices nightly. ▪ She has no medical problems. She takes a combination oral contraceptive. Family history is noncontributory. She does not use tobacco, alcohol, or recreational drugs. ▪ She is afebrile with normal vital signs. Examination reveals tenderness distal to the lateral epicondyle, with pain increased with wrist extension against resistance. -

Imaging Ultrasound Imaging for the Rheumatologist XI. Ultrasound Imaging in Regional Pain Syndromes A
Imaging Ultrasound imaging for the rheumatologist XI. Ultrasound imaging in regional pain syndromes A. Iagnocco1, E. Filippucci2, G. Meenagh3, L. Riente4, A. Delle Sedie4, S. Bombardieri4, W. Grassi2, G. Valesini1 1Cattedra di Reumatologia, Sapienza - ABSTRACT In the present review, an update of the Università di Roma, Roma, Italy; Regional pain syndromes (RPS) are available data about US imaging in 2 Cattedra di Reumatologia, Università common complaints in clinical rheu- RPS is provided and the research agen- Politecnica delle Marche, Jesi, Italy; matological practice. Ultrasound (US) da relating to US imaging of local soft 3AntrimAntrim AreaArea Hospital,Hospital, Antrim,Antrim, NorthernNorthern Ireland, United Kingdom; allows a detailed assessment of soft tis- tissue rheumatism is discussed. 4Unità Operativa di Reumatologia, sue involvement and its use may have Università di Pisa, Pisa, Italy. considerable impact on the manage- Clinical applications Annamaria Iagnocco, MD; Emilio ment of RPS. The present review pro- A list of the most common RPS to- Filippucci, MD; Gary Meenagh, MD; vides an update of the available data gether with the corresponding patho- Lucrezia Riente, MD; Andrea Delle Sedie, about US imaging in RPS together with logical conditions that may be revealed MD; Stefano Bombardieri, MD, Professor research issues relating to periarticu- by US is presented in Table I. Differ- of Rheumatology; Walter Grassi, MD, lar soft tissue pathology. The research ent pathological conditions may mani- Professor of Rheumatology; Guido agenda covers: defi nition of standard fest with similar clinical features and Valesini, MD, Professor of Rheumatology. scanning protocols for US examination US assessment may be critical for the Please address correspondence to: of the most common RPS assessed by Dr.