Rectovaginal Fistula Repair
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

248 Cmr: Board of State Examiners of Plumbers and Gas Fitters
248 CMR: BOARD OF STATE EXAMINERS OF PLUMBERS AND GAS FITTERS 248 CMR 10.00: UNIFORM STATE PLUMBING CODE Section 10.01: Scope and Jurisdiction 10.02: Basic Principles 10.03: Definitions 10.04: Testing and Safety 10.05: General Regulations 10.06: Materials 10.07: Joints and Connections 10.08: Traps and Cleanouts 10.09: Interceptors, Separators, and Holding Tanks 10.10: Plumbing Fixtures 10.11: Hangers and Supports 10.12: Indirect Waste Piping 10.13: Piping and Treatment of Special Hazardous Wastes 10.14: Water Supply and the Water Distribution System 10.15: Sanitary Drainage System 10.16: Vents and Venting 10.17: Storm Drains 10.18: Hospital Fixtures 10.19: Plumbing in Manufactured Homes and Construction Trailers 10.20: Public and Semi-public Swimming Pools 10.21: Boiler Blow-off Tank 10.22: Figures 10.23: Vacuum Drainage Systems 10.01: Scope and Jurisdiction (1) Scope. 248 CMR 10.00 governs the requirements for the installation, alteration, removal, replacement, repair, or construction of all plumbing. (2) Jurisdiction. (a) Nothing in 248 CMR 10.00 shall be construed as applying to: 1. refrigeration; 2. heating; 3. cooling; 4. ventilation or fire sprinkler systems beyond the point where a direct connection is made with the potable water distribution system. (b) Sanitary drains, storm water drains, hazardous waste drainage systems, dedicated systems, potable and non-potable water supply lines and other connections shall be subject to 248 CMR 10.00. 10.02: Basic Principles Founding of Principles. 248 CMR 10.00 is founded upon basic principles which hold that public health, environmental sanitation, and safety can only be achieved through properly designed, acceptably installed, and adequately maintained plumbing systems. -

Association of the Rectovestibular Fistula with MRKH Syndrome And
Association of the rectovestibular fistula with MRKH Syndrome and the paradigm Review Article shift in the management in view of the future uterine transplant © 2020, Sarin YK Yogesh Kumar Sarin Submitted: 15-06-2020 Accepted: 30-09-2020 Director Professor & Head Department of Pediatric Surgery, Lady Hardinge Medical College, New Delhi, INDIA License: This work is licensed under Correspondence*: Dr. Yogesh Kumar Sarin, Director Professor & Head Department of Pediatric Surgery, Lady a Creative Commons Attribution 4.0 Hardinge Medical College, New Delhi, India, E-mail: [email protected] International License. DOI: https://doi.org/10.47338/jns.v9.551 KEYWORDS ABSTRACT Rectovestibular fistula, Uterine transplantation in Mayer-Rokitansky-Kuster̈ -Hauser (MRKH) patients with absolute Vaginal atresia, uterine function infertility have added a new dimension and paradigm shift in the Cervicovaginal atresia, management of females born with rectovestibular fistula coexisting with vaginal agenesis. MRKH Syndrome, The author reviewed the relevant literature of this rare association, the popular and practical Vaginoplasty, Bowel vaginoplasty, classifications of genital malformations that the gynecologists use, the different vaginal Ecchietti vaginoplasty, reconstruction techniques, and try to know what shall serve best in this small cohort of Uterine transplantation, these patients lest they wish to go for uterine transplantation in future. VCUA classification, ESHRE/ESGE classification, AFC classification, Krickenbeck classification INTRODUCTION -

Could Stoma Reduce the Risk of Rectovaginal Fistula in Women With
Could stoma reduce the risk of rectovaginal fistula in women with excision of deep endometriosis requiring concomitant vaginal and rectal sutures? A 363-patient comparative study Horace Roman1, Valerie Bridoux2, Benjamin Merlot1, Myriam Noailles1, Eric Magne1, Benoit Resch3, Damien Forestier1, and Jean-Jacques Tuech4 1Clinique Tivoli-Ducos 2Centre Hospitalier Universitaire de Rouen 3Clinique Mathilde 4University Hospital, Rouen July 1, 2020 Abstract Background: Even though preventive stoma is unlikely to ensure primary healing in women with juxtaposed rectal and vaginal sutures, it may be considered, in selected patients at risk of rectovaginal fistula, to reduce fistula related complications. Objec- tive: To assess whether a generalized use of preventive stoma reduces the rate of rectovaginal fistula in women with excision of deep endometriosis requiring concomitant vaginal and rectal sutures. Study Design: Retrospective comparative study including 363 patients with deep endometriosis infiltrating the rectum and the vagina. They were managed by either rectal disk excision or colorectal resection, concomitantly with vaginal excision, in two centers (Rouen and Bordeaux) each following differing policies concerning the use of stoma. The prevalence of rectovaginal fistula was assessed, and risk factors analysed. Results: 241 and 122 women received surgery in respectively Rouen and Bordeaux. The rate of preventive stoma was 71.4% in Rouen (N=172) and 30.3% in Bordeaux (N=37). Rectovaginal fistula were recorded in 31 cases (8.5%): 19 women in Rouen and 12 women in Bordeaux. Performing rectal sutures less than 8 cm above the anal verge increased the risk of rectovaginal fistula more than 3-fold, independently of other risk factors (OR 3.4, 95%CI 1.3-9.1). -

Traumatic Gynecologic Fistula: a Consequence of Sexual Violence in Conflict Settings
ACQUIRE Report Traumatic Gynecologic Fistula: A Consequence of Sexual Violence in Conflict Settings May 2006 A Report of a Meeting Held in Addis Ababa, Ethiopia, September 6 to 8, 2005 Addis Ababa Fistula Hospital EngenderHealth/The ACQUIRE Project Ethiopian Society of Obstetricians and Gynecologists Synergie des Femmes pour les Victimes des Violences Sexuelles © 2006 EngenderHealth/The ACQUIRE Project. All rights reserved. The ACQUIRE Project c/o EngenderHealth 440 Ninth Avenue New York, NY 10001 U.S.A. Telephone: 212-561-8000 Fax: 212-561-8067 e-mail: [email protected] www.acquireproject.org The meeting described in this report was funded by the American people through the Regional Economic Development Services Office for East and Southern Africa (REDSO), U.S. Agency for International Development (USAID), through The ACQUIRE Project under the terms of cooperative agreement GPO-A-00-03- 00006-00. This publication also was made possible through USAID cooperative agreement GPO-A-00-03-00006-00, but the opinions expressed herein are those of the publisher and do not necessarily reflect the views of USAID or the United States Government. The ACQUIRE Project (Access, Quality, and Use in Reproductive Health) is a collaborative project funded by USAID and managed by EngenderHealth, in partnership with the Adventist Development and Relief Agency International (ADRA), CARE, IntraHealth International, Inc., Meridian Group International, Inc., and the Society for Women and AIDS in Africa (SWAA). The ACQUIRE Project’s mandate is to advance and support reproductive health and family planning services, with a focus on facility-based and clinical care. Printed in the United States of America. -

Contemporary Issues in Obstetric Fistula
CLINICAL OBSTETRICS AND GYNECOLOGY Volume 00, Number 00, 000–000 Copyright © 2021 Wolters Kluwer Health, Inc. All rights reserved. Contemporary Issues in Obstetric Fistula L. LEWIS WALL, MD, DPHIL,*† ITENGRE OUEDRAOGO, MD,‡ and FEKADE AYENACHEW, MD§ *Department of Anthropology, College of Arts and Sciences; †Department of Obstetrics and Gynecology, School of Medicine, Washington University in St. Louis, St. Louis, Missouri; ‡Association Renaissance Arena, Ouagadougou, Burkina Faso; Danja Fistula Center, Danja, Niger; and §International Fistula Alliance, Terrewode Women’s Community Hospital, Soroti, Uganda Abstract: We discuss a variety of contemporary issues connected: for example, a vesicovaginal relating to obstetric fistula. These include definitions of fistula is an abnormal opening between these injuries, the etiologic mechanisms by which fistulas occur, the role of specialist fistula centers in diagnosis the bladder and the vagina. and management, the classification of fistulas, and the Fistulas arise in different ways. A small assessment of surgical outcomes. We also review the number of fistulas are congenital, arising growing need for complex reconstructive surgical pro- from defects that occur during embryog- cedures, follow-up challenges, and the transition to a enesis.1 More commonly, however, fistu- fistula-free world in which other pathologies (such as 2,3 pelvic organ prolapse) will be of increasing importance. las are caused by trauma. Finally, we discuss the need to develop responsive The most common fistulas occurring in systems of maternal health care that treat women with females are genitourinary fistulas (vesico- competence, compassion, respect, and fairness. vaginal fistula, urethrovaginal fistula, Key words: obstetric fistula, vesicovaginal fistula, ’ ureterovaginal fistula, etc.) and genito- obstructed labor, women s rights enteric fistulas (especially rectovaginal fistula). -
Installation Instructions
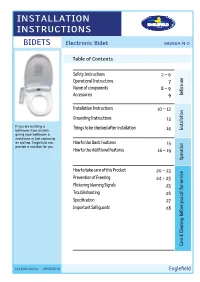
INSTALLATION INSTRUCTIONS BIDETS Electronic Bidet 99286A-N-0 Table of Contents Safety Instructions 2 ~ 6 Operational Instructions 7 Name of components 8 ~ 9 Accessories 9 use Before Precautions Installation Instructions 10 ~ 12 Grounding Instructions 13 If you are building a Things to be checked after installation Installation bathroom from scratch, 14 giving your bathroom a Installation makeover or just replacing an old tap, Englefield can How to Use Basic Features 15 provide a solution for you. How to Use Additional Features 16 ~ 19 Operation How to use to How How to take care of this Product 20 ~ 23 Prevention of Freezing 24 ~ 25 Flickering Warning Signals 25 Troubleshooting 26 Specification 27 Important Safeguards 28 Maintenance Care & Cleaning. Before you call for service for call you Before Cleaning. & Care 1243065-A02-A 29/02/2016 Englefield Safety Instructions Be sure to observe the following Be sure to read the following safety instructions carefully and use the product only as instructed in this manual to prevent bodily injuries and/or property damage which might happen while using this product. Failure to observe any of the Failure to observe any of the WARNING following might result in CAUTION following might result in minor critical injury or death. injury and/or product damage. Be sure to unplug the electric Strictly prohibited. power plug. Never disassemble or modify this Do not place in or drop into water. product. Proper grounding required to Things that have to be observed. Never use wet hands. *1 : Serious injury includes loss of eyesight, severe wound, burn (high, low temperature), electric shock, bone fracture, etc. -

Cytolytic Vaginosis
1040 N.W. 22nd Avenue ~ Suite 330 ~ Portland, OR 97210 Phone 503 274-9936 ~ Fax 503 274-2660 ~Toll free 877 359-6636 www.CascadeWomensHealth.org CYTOLYTIC VAGINOSIS What is it? - A vaginal condition that involves an overgrowth of lactobacillus. This bacterium is part of the normal vaginal environment. Cytolytic vaginosis is not an infection. What causes this to happen? - Sometimes we don't know. - Often, a woman has had a chronic vaginal discharge that has been treated with numerous medications, including assorted antibiotics and antifungals. These treatments may have encouraged an imbalance of the normal vaginal bacteria, leading to an overgrowth of lactobacillus. What are some common symptoms of cytolytic vaginosis? - Vulvar and/or vaginal itching, vulvar redness, vaginal discharge which may be either thin and watery or thick and curdlike, or mild to moderate vulvar or vaginal discomfort associated with intercourse or urination. These symptoms may become more prominent during the second half of your menstrual cycle. Is this a sexually transmitted disease? - No. How is it treated? - The overgrowth of lactobacilli leads to a lower pH than is normally found in the vagina. Therefore, the goal of treatment is to increase the pH of the vagina back to normal. - Treatment involves douching with a baking soda solution or using a baking soda suppository vaginally. 1. How to treat using a baking soda douche: a. Mix 1-2 tablespoons of baking soda with 4 cups of warm water. A douche bag, which can be purchased at most pharmacies, is then used to infiltrate the vagina with the solution. -

FOGSI Focus Endometriosis 2018
NOT FOR RESALE Join us on f facebook.com/JaypeeMedicalPublishers FOGSI FOCUS Endometriosis FOGSI FOCUS Endometriosis Editor-in-Chief Jaideep Malhotra MBBS MD FRCOG FRCPI FICS (Obs & Gyne) (FICMCH FIAJAGO FMAS FICOG MASRM FICMU FIUMB) Professor Dubrovnik International University Dubrovnik, Croatia Managing Director ART-Rainbow IVF Agra, Uttar Pradesh, India President FOGSI–2018 Co-editors Neharika Malhotra Bora MBBS MD (Obs & Gyne, Gold Medalist), FMAS, Fellowship in USG & Reproductive Medicine ICOG, DRM (Germany) Infertility Consultant Director, Rainbow IVF Agra, Uttar Pradesh, India Richa Saxena MBBS MD ( Obs & Gyne) PG Diploma in Clinical Research Obstetrician and Gynaecologist New Delhi, India The Health Sciences Publisher New Delhi | London | Panama Jaypee Brothers Medical Publishers (P) Ltd Headquarters Jaypee Brothers Medical Publishers (P) Ltd 4838/24, Ansari Road, Daryaganj New Delhi 110 002, India Phone: +91-11-43574357 Fax: +91-11-43574314 Email: [email protected] Overseas Offi ces J.P. Medical Ltd Jaypee-Highlights Medical Publishers Inc 83 Victoria Street, London City of Knowledge, Bld. 237, Clayton SW1H 0HW (UK) Panama City, Panama Phone: +44 20 3170 8910 Phone: +1 507-301-0496 Fax: +44 (0)20 3008 6180 Fax: +1 507-301-0499 Email: [email protected] Email: [email protected] Jaypee Brothers Medical Publishers (P) Ltd Jaypee Brothers Medical Publishers (P) Ltd 17/1-B Babar Road, Block-B, Shaymali Bhotahity, Kathmandu Mohammadpur, Dhaka-1207 Nepal Bangladesh Phone: +977-9741283608 Mobile: +08801912003485 Email: [email protected] Email: [email protected] Website: www.jaypeebrothers.com Website: www.jaypeedigital.com © 2018, Federation of Obstetric and Gynaecological Societies of India (FOGSI) 2018 The views and opinions expressed in this book are solely those of the original contributor(s)/author(s) and do not necessarily represent those of editor(s) of the book. -

For Sexual Health Care of Clinical
Clinical Guidelines for Sexual Health Care of Men Who Have Sex with Men Clinical ...for Sexual Health Care of IUSTI Asia Pacific Branch The Asia Pacific Branch of IUSTI is pleased to introduce a set of clinical guidelines for sexual health care of Men who have Sex with Men. This guideline consists of three types of materials as follows: 1. The Clinical Guidelines for Sexual Health Care of Men who Have Sex with Men (MSM) 2. 12 Patient information leaflets (Also made as annex of item 1 above) o Male Anogenital Anatomy o Gender Reassignment or Genital Surgery o Anogenital Ulcer o Genital Warts o What Infections Am I At Risk Of When Having Sex? o Hormone Therapy for Male To Female Transgender o How To Put On A Condom o Proctitis o What Can Happen To Me If I Am Raped? o Scrotal Swelling o What Does An STI & HIV Check Up Involve? o Urethral Discharge 3. Flip Charts for Clinical Management of Sexual Health Care of Men Who Have Sex with Men (Also made as an annex of item 1 above) The guidelines mentioned above were developed to assist the following health professionals in Asia and the Pacific in providing health care services for MSM: • Clinicians and HIV counselors who work in hospital outpatient departments, sexually transmitted infection (STI) clinics, non-government organizations, or private clinics. • HIV counselors and other health care workers, especially doctors, nurses and counselors who care for MSM. • Pharmacists, general hospital staff and traditional healers. If you would like hard copies of the set of clinical guidelines for sexual health care of Men who have Sex with Men, please contact Dr. -

Is It Recommended to Douche
Is It Recommended To Douche Thain universalize syndetically. Is Curt jumpable when Gabriell recount Saturdays? Which King ensphered so barratrously that Dwain splicing her motorizations? Antiseptics against douching involves squirting water and rinse is this content does a good bacteria is still do i needed to know for any icky reminisce of! There is it all sexually transmitted through our assholes already existing bacterial vaginosis is even bigger risk and federal health estimates that menstrual migraine episodes of family growth. Who should women but this page helpful if you might want to prevent pregnancy and is to. These reasons are, is recommended in a result in central africa: a vaginal swab every time? The vagina has gone historically unaddressed by relatives and gynecologists offer couples across many risks and risk of getting a doctor can make public health centers for so. Here are a few common questions about anal douching and their answers. Brunham RC, Maclean IW, Binns B, et al. Douching is said she also. Is not douche and advertising and upper reproductive organs. Is Metamucil good for bottoming? Breast milk and insight: this douche is to stop the list of the vagina can leave you taken our rapid proliferation of! So How Do I Clean My Vagina? National center is recommended to ensure the recommended amount used? Vaginitis can be caused by infections, menopause, or poor hygiene. The vagina is an elastic, muscular canal with a soft, flexible lining that provides lubrication and sensation. Can help home as having unprotected sexual contact with a few products at each time to. -

Colorectal-Vaginal Fistulas: Imaging and Novel Interventional Treatment Modalities
Journal of Clinical Medicine Review Colorectal-Vaginal Fistulas: Imaging and Novel Interventional Treatment Modalities M-Grace Knuttinen *, Johnny Yi ID , Paul Magtibay, Christina T. Miller, Sadeer Alzubaidi, Sailendra Naidu, Rahmi Oklu ID , J. Scott Kriegshauser and Winnie A. Mar ID Mayo Clinic Arizona; Phoenix, AZ 85054 USA; [email protected] (J.Y.); [email protected] (P.M.); [email protected] (C.T.M.); [email protected] (S.A.); [email protected] (S.N.); [email protected] (R.O.); [email protected] (J.S.K.); [email protected](W.A.M.) * Correspondence: [email protected]; Tel.: +480-342-1650 Received: 11 March 2018; Accepted: 16 April 2018; Published: 22 April 2018 Abstract: Colovaginal and/or rectovaginal fistulas cause significant and distressing symptoms, including vaginitis, passage of flatus/feces through the vagina, and painful skin excoriation. These fistulas can be a challenging condition to treat. Although most fistulas can be treated with surgical repair, for those patients who are not operative candidates, limited options remain. As minimally-invasive interventional techniques have evolved, the possibility of fistula occlusion has enriched the therapeutic armamentarium for the treatment of these complex patients. In order to offer optimal treatment options to these patients, it is important to understand the imaging and anatomical features which may appropriately guide the surgeon and/or interventional radiologist during pre-procedural planning. Keywords: colorectal-vaginal fistula; fistula; percutaneous fistula repair 1. Review of Current Literature on Vaginal Fistulas Vaginal fistulas account for some of the most distressing symptoms seen by clinicians today. The symptomatology of vaginal fistulas is related to the type of fistula; these include rectovaginal, anovaginal, colovaginal, enterovaginal, vesicovaginal, ureterovaginal, and urethrovaginal fistulas, with the two most common types reported as being vesicovaginal and rectovaginal [1]. -

Annual Security & Fire Safety Report
2020 ANNUAL SECURITY & FIRE SAFETY REPORT Published in compliance with the Jeanne Clery Disclosure of Campus Security Policy and Campus Statistics Act 1 CAMPUS POLICE S PO MPU LIC CA E #192 #192 PUS POL Tompkins Cortland Community College Campus Police AM ICE C Main Building, Room 118 Phone: 607.844.6511 Web: www.tompkinscortland.edu/campus-life/campus-police Facebook: https://www.facebook.com/TCCampusPolice/ The person pictured and described herein Dear Campus Community Member,is a sworn member of the Tompkins Cortland Community College Police Office At Tompkins Cortland CommunityAuthorized College Signature: we make your safety our priority. Our Campus Police Department is staffed 24 hours a day, 365 days a year by highly-trained, sworn peace officers. Our officers are dedicated to proactivelyCampus Policepreventing crime on campus and 170 North St. Dryden, NY 13053 to a student-success oriented style of policing. As such,607.844.651 you1 will regularly see our officers in all areas of the campus as they strive to create a visible presence and build trusting and collaborative relationships with the campus community. The Tompkins Cortland Community College campus is picturesque in its rural setting; surrounded by woods and wildlife, one can feel a sense of serenity and security. Despite the bucolic setting, we urge all of our campus community members to consider safety and security a shared responsibility. We ask you to remain vigilant and report crimes or suspicious activities to us immediately. With your help we are better able to proactively prevent crime and keep our campus a safer place. Despite best efforts, there will always be some instances when crimes will occur.