Ocn244448874-FY07.Pdf (2.060Mb)
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Assessment Actions
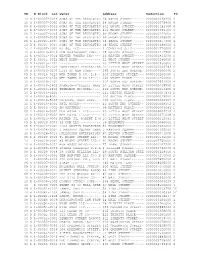
Assessment Actions Borough Code Block Number Lot Number Tax Year Remission Code 1 1883 57 2018 1 385 56 2018 2 2690 1001 2017 3 1156 62 2018 4 72614 11 2018 2 5560 1 2018 4 1342 9 2017 1 1390 56 2018 2 5643 188 2018 1 386 36 2018 1 787 65 2018 4 9578 3 2018 4 3829 44 2018 3 3495 40 2018 1 2122 100 2018 3 1383 64 2017 2 2938 14 2018 Page 1 of 604 09/27/2021 Assessment Actions Owner Name Property Address Granted Reduction Amount Tax Class Code THE TRUSTEES OF 540 WEST 112 STREET 105850 2 COLUM 226-8 EAST 2ND STREET 228 EAST 2 STREET 240500 2 PROSPECT TRIANGLE 890 PROSPECT AVENUE 76750 4 COM CRESPA, LLC 597 PROSPECT PLACE 23500 2 CELLCO PARTNERSHIP 6935500 4 d/ CIMINELLO PROPERTY 775 BRUSH AVENUE 329300 4 AS 4305 65 REALTY LLC 43-05 65 STREET 118900 2 PHOENIX MADISON 962 MADISON AVENUE 584850 4 AVENU CELILY C. SWETT 277 FORDHAM PLACE 3132 1 300 EAST 4TH STREET H 300 EAST 4 STREET 316200 2 242 WEST 38TH STREET 242 WEST 38 STREET 483950 4 124-469 LIBERTY LLC 124-04 LIBERTY AVENUE 70850 4 JOHN GAUDINO 79-27 MYRTLE AVENUE 35100 4 PITKIN BLUE LLC 1575 PITKIN AVENUE 49200 4 GVS PROPERTIES LLC 559 WEST 164 STREET 233748 2 EP78 LLC 1231 LINCOLN PLACE 24500 2 CROTONA PARK 1432 CROTONA PARK EAS 68500 2 Page 2 of 604 09/27/2021 Assessment Actions 1 1231 59 2018 3 7435 38 2018 3 1034 39 2018 3 7947 17 2018 4 370 1 2018 4 397 7 2017 1 389 22 2018 4 3239 1001 2018 3 140 1103 2018 3 1412 50 2017 1 1543 1001 2018 4 659 79 2018 1 822 1301 2018 1 2091 22 2018 3 7949 223 2018 1 471 25 2018 3 1429 17 2018 Page 3 of 604 09/27/2021 Assessment Actions DEVELOPM 268 WEST 84TH STREET 268 WEST 84 STREET 85350 2 BANK OF AMERICA 1415 AVENUE Z 291950 4 4710 REALTY CORP. -

Upper Cape Cod Vacation Planner.Pdf
2 0 1 5 UPPER CAPE COD VACATI ON PLANNER 1 Cape Cod Vacation Planner Contents About Cape Cod Vacation Planner Listings It's difficult to define what it is about Cape Cod Dining . 3 that has continued to draw so many of us back Activities . 6 to experience it again and again each summer. Perhaps it's the irresistible combination of its Shopping. 7 unique natural beauty - miles of beautiful, white- Art & Museums . 9 sand beaches and dunes and lush, fascinating marshes teeming with wildlife - its charming Fitness & Beauty . 10 history dating back to the 17th century, and its Services. 10 abundance of family-oriented activities. If lying Transportation. 10 on a gorgeous beach or reading a book on a porch overlooking wetlands isn't enough for you, Articles we suggest you take advantage of some of these The Lure of Cape Cod. 11 wonderful, quintessentially-Cape experiences you Biking. 15 will find within the Cape Cod Vacation Planner. Kayaking . 17 Contact Us Golfing . 19 Wellesley Office: (888) 281-8660 Lobsters & Steamers . 21 Brewster Office: (774) 323-3911 Website: WeNeedaVacation.com Email: [email protected] Dining Ben & Bill's Chocolate Emporium A small family of chocolate and ice cream shops in Massachusetts and Maine. We use family recipes that have been passed down from generations of candy makers. We offer the finest ingredients available for the freshest, most delicious hand-made candies. Categories: Ice Cream & Candy 209 Main Street, Falmouth ~ (508) 548-7878 ~ www.benandbills.com Bleu French Bistro $$$$ Enjoy French cuisine and culture at this stylish bistro which has as received numerous awards for "consistently top-notch" cuisine. -

FROM BULLDOGS to SUN DEVILS the EARLY YEARS ASU BASEBALL 1907-1958 Year ...Record
THE TRADITION CONTINUES ASUBASEBALL 2005 2005 SUN DEVIL BASEBALL 2 There comes a time in a little boy’s life when baseball is introduced to him. Thus begins the long journey for those meant to play the game at a higher level, for those who love the game so much they strive to be a part of its history. Sun Devil Baseball! NCAA NATIONAL CHAMPIONS: 1965, 1967, 1969, 1977, 1981 2005 SUN DEVIL BASEBALL 3 ASU AND THE GOLDEN SPIKES AWARD > For the past 26 years, USA Baseball has honored the top amateur baseball player in the country with the Golden Spikes Award. (See winners box.) The award is presented each year to the player who exhibits exceptional athletic ability and exemplary sportsmanship. Past winners of this prestigious award include current Major League Baseball stars J. D. Drew, Pat Burrell, Jason Varitek, Jason Jennings and Mark Prior. > Arizona State’s Bob Horner won the inaugural award in 1978 after hitting .412 with 20 doubles and 25 RBI. Oddibe McDowell (1984) and Mike Kelly (1991) also won the award. > Dustin Pedroia was named one of five finalists for the 2004 Golden Spikes Award. He became the seventh all-time final- ist from ASU, including Horner (1978), McDowell (1984), Kelly (1990), Kelly (1991), Paul Lo Duca (1993) and Jacob Cruz (1994). ODDIBE MCDOWELL > With three Golden Spikes winners, ASU ranks tied for first with Florida State and Cal State Fullerton as the schools with the most players to have earned college baseball’s top honor. BOB HORNER GOLDEN SPIKES AWARD WINNERS 2004 Jered Weaver Long Beach State 2003 Rickie Weeks Southern 2002 Khalil Greene Clemson 2001 Mark Prior Southern California 2000 Kip Bouknight South Carolina 1999 Jason Jennings Baylor 1998 Pat Burrell Miami 1997 J.D. -

H-1B Petition Approvals for Initial Benefits by Employers FY07
NUMBER OF H-1B PETITIONS APPROVED BY USCIS FOR INITIAL BENEFICIARIES FY 2007 Approved Employer Petitions INFOSYS TECHNOLOGIES LIMITED 4,559 WIPRO LIMITED 2,567 SATYAM COMPUTER SERVICES LTD 1,396 COGNIZANT TECH SOLUTIONS US CORP 962 MICROSOFT CORP 959 TATA CONSULTANCY SERVICES LIMITED 797 PATNI COMPUTER SYSTEMS INC 477 US TECHNOLOGY RESOURCES LLC 416 I-FLEX SOLUTIONS INC 374 INTEL CORPORATION 369 ACCENTURE LLP 331 CISCO SYSTEMS INC 324 ERNST & YOUNG LLP 302 LARSEN & TOUBRO INFOTECH LIMITED 292 DELOITTE & TOUCHE LLP 283 GOOGLE INC 248 MPHASIS CORPORATION 248 UNIVERSITY OF ILLINOIS AT CHICAGO 246 AMERICAN UNIT INC 245 JSMN INTERNATIONAL INC 245 OBJECTWIN TECHNOLOGY INC 243 DELOITTE CONSULTING LLP 242 PRINCE GEORGES COUNTY PUBLIC SCHS 238 JPMORGAN CHASE & CO 236 MOTOROLA INC 234 MARLABS INC 229 KPMG LLP 227 GOLDMAN SACHS & CO 224 TECH MAHINDRA AMERICAS INC 217 VERINON TECHNOLOGY SOLUTIONS LTD 213 THE JOHNS HOPKINS MED INSTS OIS 205 YASH TECHNOLOGIES INC 202 ADVANSOFT INTERNATIONAL INC 201 UNIVERSITY OF MARYLAND 199 BALTIMORE CITY PUBLIC SCHOOLS 196 PRICEWATERHOUSECOOPERS LLP 192 POLARIS SOFTWARE LAB INDIA LTD 191 UNIVERSITY OF MICHIGAN 191 EVEREST BUSINESS SOLUTIONS INC 190 IBM CORPORATION 184 APEX TECHNOLOGY GROUP INC 174 NEW YORK CITY PUBLIC SCHOOLS 171 SOFTWARE RESEARCH GROUP INC 167 EVEREST CONSULTING GROUP INC 165 UNIVERSITY OF PENNSYLVANIA 163 GSS AMERICA INC 160 QUALCOMM INCORPORATED 158 UNIVERSITY OF MINNESOTA 151 MASCON GLOBAL CONSULTING INC 150 MICRON TECHNOLOGY INC 149 THE OHIO STATE UNIVERSITY 147 STANFORD UNIVERSITY 146 COLUMBIA -

Providence College Quick Facts 2010 Women's Soccer Roster
Providence College SPORTS INFORMATION Quick Facts CONTACT Location ...............................................................................................Providence, Rhode Island 02918 John May Founded ................................................................................................................................................... 1917 (P) 401-865-1733 Enrollment ............................................................................................................................................... 3,837 (F) 401-865-2583 President ..................................................................................................Reverend Brian J. Shanley, O.P. Denomination .........................................................................................................Catholic (Dominican) [email protected] Associate VP for College Athletics/Athletic Director .................................. Robert G. Driscoll, Jr. Assistant VP/Executive Associate Athletic Director/SWA ..............................................Jill LaPoint Associate AD/Student-Athlete Development ................................................................Nick Reggio Associate Athletic Director/Facilities/Game Mgmt. ......................................................Carl LaBranche Associate Athletic Director/External Relations ............................................................... Steve Napolillo Associate Athletic Director/Business ..................................................................................................Mac -

Kelly, Colleen A., Comp. Asian Studies: a Catalogue of Asian
DOCUMENT RESUME ED 216 962 SO 014 063 AUTHOR Kelly, Colleen A., Comp. TITLE Asian Studies: A Catalogue of Asian Resources in Connecticut. Area Studies Resources Guides, Number One. INSTITUTION Connecticut Univ., Storrs. Thut (I.N.) World Education Center. PUB DATE 80 NOTE 95p.; Print marginally legible. AVAILABLE FROM I.N. Thut World Cducation Center, Box U-32, University of Connecticut, Storrs, CT 06268 ($3.50, plus $0.70 postage). EDRS PRICE MF01 Plus Postage. PC Not Available from EDRS. DESCRIPTORS Arts Centers; Asian History; *Asian Studies; Dining Facilities; Elementary Secondary Education; Films; Higher Education; Human Resources; Museums; Publishing IndlAstry; Resource Centers; Resource Materials; Theater Arts IDENTIFIERS *Connecticut ABSTRACT This directory cites Asian resources, services, institutions, and groups in Connecticut. It is intended to strengthen international studies through improved state-wide cooperation and communication. The directory is organized by the following' topics: educational centers (including descriptions of the servicesprovided and, in some cases, materials available from the centers); sourcesof curriculum materials and information; performing arts; museumsand art galleries; restaurants and food shops;specialty and antique shops; martial arts; libraries, bookstores, art supply stores,and places of worship; free and rental films; human resources; and publishers. (RM) ********************************************************************** * Reproductions supplied by EDRS are the best that can be made -

Multiplying Strategic Thai Investments in the US
Contents Acknowledgements .................................................................................................................... 3 Executive Summary ................................................................................................................... 5 Introduction ................................................................................................................................ 7 I. Investment Database .............................................................................................................11 Trade and Investment Flows into the U.S...........................................................................11 Calculating Thai Investment Flows into the U.S. ................................................................12 Summary of Thai investment in the U.S. ............................................................................13 Recommendations .............................................................................................................14 Limitations ..........................................................................................................................15 II. State-by-State Analysis .........................................................................................................17 Background ........................................................................................................................17 Methodology ......................................................................................................................17 -

Pool, Cabana Added to COAH Proposal Developer Submits Revisions for Tutor Time Property
July 23, 2009 Newsstand 75¢ The Home-Delivered 53¢ www.theitemonline.com Serving our Community mmunitySince 1888 Item Night out PMP grant against crime $50,000 helps pay Town holds event rehearsal salaries. of Millburn and Short Hills Aug. 4. See A3 See A7 LIVINGSTON ZONING WACKY COMPETITOR MAKES A SPLASH Pool, cabana added to COAH proposal Developer submits revisions for Tutor Time property By Erin Patricia Griffiths The plan maintains the propos- Livingston Short Hills Coalition, of The Item al for the four-story, 100-unit apart- brought their concerns before the ment buildings with 20 percent Township Committee in Decem- TMB Partners, the developer low to moderate income housing ber. The Committee responded by who submitted plans proposing to availability on the 4.275-acre prop- hiring experts for the case in Janu- build 73-foot high, four-story apart- erty, but includes the addition of a ary, who submitted a report on the ment buildings on the property on pool, hot tub and cabana along environmental impact to the court South Orange Avenue bordering with 213 parking spaces. that month. Millburn Township, submitted a When TMB Partners submitted On Feb. 19, a judge postponed new plan Friday for the 4.2-acre the initial application for the con- the hearing to determine whether property which proposes a pool, struction of two buildings to the or not Millburn officials could par- hot tub and cabana club in addi- Livingston Planning Board, sever- ticipate in the Livingston case. tion to the high-rises. al township residents on the bor- Millburn Township officials In response to the latest plans, der of the property raised issue were denied the motion to inter- the Short Hills Association and the with the proposal. -
Actions on Applications in 2010
YR B Block Lot Owner Address Reduction TC 10 R 1-00007-0029 SONS OF THE REVOLUTIO 26 WATER STREET~~~~~~ 0000000048200 4 10 R 1-00007-0030 SONS OF THE REVOLUTIO 24 WATER STREET~~~~~~ 0000000075400 4 09 R 1-00007-0033 SONS OF THE REVOLUTIO 101 BROAD STREET~~~~~ 0000000183700 4 10 R 1-00007-0033 SONS OF THE REVOLUTIO 101 BROAD STREET~~~~~ 0000000386500 4 09 R 1-00007-0035 SONS OF THE REVOLUTIO 99 BROAD STREET~~~~~~ 0000000244000 4 10 R 1-00007-0035 SONS OF THE REVOLUTIO 99 BROAD STREET~~~~~~ 0000000305500 4 09 R 1-00007-0037 SONS OF THE REVOLUTIO 58 PEARL STREET~~~~~~ 0000000277800 4 10 R 1-00007-0037 SONS OF THE REVOLUTIO 58 PEARL STREET~~~~~~ 0000000389000 4 10 R 1-00007-1001 BZ 66, LLC~~~~~~~~~~~ 1 COENTIES SLIP~~~~~~ 0000001770000 4 10 R 1-00010-0019 JMW RESTAURANT CORP~~ 25 BRIDGE STREET~~~~~ 0000000217500 4 10 R 1-00011-0014 BEAVER TOWERS INC~~~~ 26 BEAVER STREET~~~~~ 0000000813000 2 10 R 1-00015-0022 WEST EDEN~~~~~~~~~~~~ 21 WEST STREET~~~~~~~ 0000000280000 2 09 R 1-00015-1101 ~~~~~~~~~~~~~~~~~~~~~ 20 LITTLE WEST STREET 0000000950000 4 10 R 1-00015-1102 TWENTYWEST PROPERTIES 20 LITTLE WEST STREET 0000000003783 2 09 R 1-00016-0100 CITY OF NEW YORK~~~~~ 345 SOUTH END AVENUE~ 0000005600000 2 09 R 1-00016-0120 WFP TOWER A CO. L.P.~ 200 LIBERTY STREET~~~ 0000010200000 4 09 R 1-00016-0150 WFP TOWER D CO LP~~~~ 250 VESEY PLACE~~~~~~ 0000010250000 4 10 R 1-00016-1301 ~~~~~~~~~~~~~~~~~~~~~ 102 NORTH END AVENUE~ 0000007661000 4 10 R 1-00016-1402 SCANLON-O'KELLY, MARY 30 LITTLE WEST STREET 0000000018585 2 09 R 1-00016-2200 ZEMELMAN MICHAEL~~~~~ -

Up Foreign Aid Bill
Distribution jf*V, Mj* Ant N. Mf if Toefey 4$bt, tow fa tbe Ms. T#taorraw, 23,425 Mr. Ugh in die mid Ms. SUB- tore*. SM weather, p*je 1. DIAL 741-0010 *xUu. kud Cl»u Pott*|i 86, NO. ioo iddMoul JOUtas Otflm. RED BANK, N. J_ FRIDAY, NOVEMBER IS. 1963 7c PER COPY PAGE Up Foreign Aid Bill WASHINGTON (AP)-A bit- It broke out over an amend- was defeated 46-40. Senate Re- Communist bloc countries. Thursday, appeared on the ment would not be voted on any iright, D-Ark., floor manager strategic goods to Yugoslavia tor dispute over proposed grain ment by Sen. Karl E. Mundt, publican Leader Everett M. Once the tabling motion was verge of final passage. time soon "if I can help it." for the bill and chairman of the and in transactions with "many, sales to the Soviet bloc is hold- R-S.D.. td prohibit the Export- Dlrkseh'of Illinois, who has defeated, and with no end of the Kennedy charged tha^ the Mundt said his amendment, 'orelgn Relations Committee, many countries." Ing up Senate passage of Presi- Import Bank from guaranteeing worked with Mansfield for the debate in sight, the Senate re- cuts were denying him an es- on file for days, was promptei contended this involved a nor- It was 10:35 p.m. when the dent Kennedy's badly mauled payments for private grata bill's passage, failed to vote cessed until noon today. sential foreign policy tool. by Export-Import Bank plans t< mal business practice. -

Brockton Public Schools
BROCKTON PUBLIC SCHOOLS SUMMER RESOURCE GUIDE FAMILY FUN IN THE CITY AND BEYOND! B.P.S. School Registration and Parent Information Center SUMMER 2013 SUMMER 2013 Summer is almost here and many parents and family members will be looking for activities, programs and things to do with their children. We have complied a listing of many summer activities for the children and their parents to take part in. This summer guide to get you going and give you plenty of things to do! No more excuses like "I'm bored,’ "There's nothing to do." Many exciting activities for everyone from young to old. School's out, so why not fill your days with activities that score high marks with the whole family. From ways to take learning on the road to the discoveries your child can make right in your backyard, these ideas will welcome a season to explore, learn, and play. We hope this guide is helpful in planning for an educational, fun and healthy summer of 2013. Please call the programs listed for more information. For additional information please contact: Jane Feroli ~ Brockton Public Schools Specialist for Parent Engagement at 508-894-4328 or email [email protected] Have a fun and safe summer! This guide was created with the assistance from the parent liaisons as part of the Parent Engagement Program in the Brockton Public Schools. TABLE of CONTENTS Page 3 Brockton School Department Information Page 4 Summer Fun in Brockton Page 5 Mayor Balzotti’s Friday Night Movies Page 6 Farmers Markets Page 7 Brockton Summer Free Lunch Program Page 8 - 9 Brockton After Dark Page 10 B.P.S. -

Massachusetts Department of Revenue
Massachusetts Department of Revenue Business Name Sales Name Sales Street Sales City State Zip Issued Number SMARTSTOP CONVENIENCE INC SMARTSTOP CONVENIENT STORE 270 NORTH AVE ABINGTON MA 02351 10/01/2016 212783104 AMEERA INC TEDESCHI FOOD SHOPS 394 145 NORTH QUINCY STREET ABINGTON MA 02351 10/01/2016 2068418560 JAY UMIYA INC MICHAELS CONVENIENCE STORE 194 NORTH AVE ABINGTON MA 02351 10/01/2016 693841920 A&D GAS CO INC A&D GAS CO INC 115 BROCKTON AVE ABINGTON MA 02351 12/06/2016 174862336 STONES AUTO RECYCLING INC ABINGTON SUNOCO 907 BEDFORD ST ABINGTON MA 02351 12/08/2016 1801433088 ZALA INC J D VARIETY 201 N QUINCY ST ABINGTON MA 02351 10/01/2016 1595068416 S R PACKAGE STORE INC BILLY LIQUORS 760 BROCKTON AVE ABINGTON MA 02351 10/01/2016 546820096 BEST BUY AUTO WHOLESALERS INC ABINGTON GAS 225 BROCKTON AVE ABINGTON MA 02351 10/14/2016 445427712 DEVAL CONVENIENCE INC DEVAL CONVENIENCE INC 852 HANCOCK ST ABINGTON MA 02351 10/01/2016 1615712256 SHIVA KISHA CORP ABINGTON LIQUORS 585 WASHINGTON ST ABINGTON MA 02351 10/01/2016 1020481536 KANAIYO LLC ROSIE'S LIQUOR & DELI 751 BEDFORD ST ABINGTON MA 02351 11/23/2016 1892274176 MOHAMMAD H ABUSABIHA 7-ELEVEN 32437E 2 BROCKTON AVE ABINGTON MA 02351 10/01/2016 1034268672 SMIT SUPER STORE LLC ROUTE 18 SUPER STORE 336 WASHINGTON ST ABINGTON MA 02351 10/01/2016 1754615808 MUGHAL BROTHERS INC CENTER AVENUE SUNOCO 336 CENTER AVENUE ABINGTON MA 02351 11/17/2016 688533504 RBRC, INC. D'ANN'S SPORTS & ENTERTAINMENT 340 CENTRE AVE ABINGTON MA 02351 10/01/2016 1781354496 DJG CORPORATION BORDERLINE SERVICE