NIE Annual Report Model Final.Indd
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Thiruvallur District
DISTRICT DISASTER MANAGEMENT PLAN FOR 2017 TIRUVALLUR DISTRICT tmt.E.sundaravalli, I.A.S., DISTRICT COLLECTOR TIRUVALLUR DISTRICT TAMIL NADU 2 COLLECTORATE, TIRUVALLUR 3 tiruvallur district 4 DISTRICT DISASTER MANAGEMENT PLAN TIRUVALLUR DISTRICT - 2017 INDEX Sl. DETAILS No PAGE NO. 1 List of abbreviations present in the plan 5-6 2 Introduction 7-13 3 District Profile 14-21 4 Disaster Management Goals (2017-2030) 22-28 Hazard, Risk and Vulnerability analysis with sample maps & link to 5 29-68 all vulnerable maps 6 Institutional Machanism 69-74 7 Preparedness 75-78 Prevention & Mitigation Plan (2015-2030) 8 (What Major & Minor Disaster will be addressed through mitigation 79-108 measures) Response Plan - Including Incident Response System (Covering 9 109-112 Rescue, Evacuation and Relief) 10 Recovery and Reconstruction Plan 113-124 11 Mainstreaming of Disaster Management in Developmental Plans 125-147 12 Community & other Stakeholder participation 148-156 Linkages / Co-oridnation with other agencies for Disaster 13 157-165 Management 14 Budget and Other Financial allocation - Outlays of major schemes 166-169 15 Monitoring and Evaluation 170-198 Risk Communications Strategies (Telecommunication /VHF/ Media 16 199 / CDRRP etc.,) Important contact Numbers and provision for link to detailed 17 200-267 information 18 Dos and Don’ts during all possible Hazards including Heat Wave 268-278 19 Important G.Os 279-320 20 Linkages with IDRN 321 21 Specific issues on various Vulnerable Groups have been addressed 322-324 22 Mock Drill Schedules 325-336 -
Camp Day FN/AN Camp Site ( Site, Village Name and Name of PHC Area)
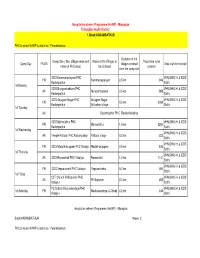
Hospital on wheels Programme (HoWP) - Microplan Thiruvallur Health District 1.Block:KADAMBATHUR PHC to which HoWP is attached : Perambakkam Distance of the Camp Site ( Site, Village name and Name of the Villages to Population to be Camp Day FN/AN villages covered Area staff to involved name of PHC area) be Covered covered from the camp site ICDS Kamavarpalayam PHC VHN,SHN, HI & ICDS FN Kammavarpalyam 0.5 km 946 Kadampathur Staffs 1st Monday ICDS Nungambakkam PHC VHN,SHN, HI & ICDS AN Nungambakkam 0.5 km 988 Kadampathur Staffs ICDS Anjugam Nagar PHC Anjugam Nagar, VHN,SHN, HI & ICDS FN 0.5 km 2360 Kadampathur Adikathur village Staffs 1st Tuesday AN Kadambathur PHC Review Meeting ICDS Mellnalathur PHC VHN,SHN, HI & ICDS FN Mellnalathur 1.0 km 3264 Kadampathur Staffs 1st Wednesday VHN,SHN, HI & ICDS AN Temple Pattarai PHC Kadampathur Pattarai village 0.3 km 532 Staffs VHN,SHN, HI & ICDS FN ICDS Madathukuppam PHC Vidaiyur Madathukuppam 0.5 km 510 Staffs 1st Thursday VHN,SHN, HI & ICDS AN ICDS Raman koil PHC Vidaiyur Raman koil 1.0 km 1141 Staffs VHN,SHN, HI & ICDS FN ICDS Veppanchetti PHC Vidaiyur Veppanchettai 0.2 km 494 Staffs 1st Friday CST Church Phillispuram PHC VHN,SHN, HI & ICDS AN Phillispuram 0.2 km 455 Vidaiyur Staffs PU School Madurakandigai PHC VHN,SHN, HI & ICDS 1st Saturday FN Madurakandigai & Chenji 0.2 km 345 Vidaiyur Staffs Hospital on wheels Programme (HoWP) - Microplan Block:KADAMBATHUR Week: 2 PHC to which HoWP is attached : Perambakkam Distance of the Camp Site ( Site, Village name and Name of the Villages to Population -

Sustaining the Traditional Paithani Saree Weaving of Maharashtra, India Reena Bhatia1* and Deepti Desai2
Available online at www.globalilluminators.org GlobalIlluminators FULL PAPER PROCEEDING Multidisciplinary Studies Full Paper Proceeding ITMAR -2014, Vol. 1, 529-536 ISBN: 978-969-9948-24-4 ITMAR-14 Sustaining The Traditional Paithani Saree Weaving Of Maharashtra, India 1* 2 Reena Bhatia and Deepti Desai 1,2Department of Clothing and Textiles, Faculty of Family and Community Sciences, The Maharaja Sayajirao University of Baroda, Vadodara, Gujarat, India. Abstract Among the hand woven sarees of India, Paithani is famous and has played a significant role in weaving together the socio-cultural fabric of Maharashtra since it is traditionally a part of the trousseau of every Maharashtra bride. The aim of the study was to document the existing weaving traditions of Paithani and explore the possibility of weaving Paithani as a yardage with different product layout. To achieve the formulated objectives a descriptive cum exploratory study was planned. Data collection was done through observation and interview schedule during field visits in Bhandge Lane, Yeola. The weavers were selected through purposive random sampling. Adaptation of Paithani saree layout on handloom was done for selected product range to unearth new opportunities for a local craft and help them expand their market. Data analysis indicated that the younger generation was involved in the traditional weaving of Paithani saree. The weavers were training their children in traditional weaving practices of Paithani; contributing positively to its sustainability. The craft details in terms of raw materials, loom set-up, dyeing, weaving process, types of Paithani, colours and motifs was documented through photographs and supplemented with text. It was reassuring to learn that 80 per cent of weavers would prefer to diversify into other products instead of just weaving saree if done using same technique of Paithani weaving. -

SNO APP.No Name Contact Address Reason 1 AP-1 K
SNO APP.No Name Contact Address Reason 1 AP-1 K. Pandeeswaran No.2/545, Then Colony, Vilampatti Post, Intercaste Marriage certificate not enclosed Sivakasi, Virudhunagar – 626 124 2 AP-2 P. Karthigai Selvi No.2/545, Then Colony, Vilampatti Post, Only one ID proof attached. Sivakasi, Virudhunagar – 626 124 3 AP-8 N. Esakkiappan No.37/45E, Nandhagopalapuram, Above age Thoothukudi – 628 002. 4 AP-25 M. Dinesh No.4/133, Kothamalai Road,Vadaku Only one ID proof attached. Street,Vadugam Post,Rasipuram Taluk, Namakkal – 637 407. 5 AP-26 K. Venkatesh No.4/47, Kettupatti, Only one ID proof attached. Dokkupodhanahalli, Dharmapuri – 636 807. 6 AP-28 P. Manipandi 1stStreet, 24thWard, Self attestation not found in the enclosures Sivaji Nagar, and photo Theni – 625 531. 7 AP-49 K. Sobanbabu No.10/4, T.K.Garden, 3rdStreet, Korukkupet, Self attestation not found in the enclosures Chennai – 600 021. and photo 8 AP-58 S. Barkavi No.168, Sivaji Nagar, Veerampattinam, Community Certificate Wrongly enclosed Pondicherry – 605 007. 9 AP-60 V.A.Kishor Kumar No.19, Thilagar nagar, Ist st, Kaladipet, Only one ID proof attached. Thiruvottiyur, Chennai -600 019 10 AP-61 D.Anbalagan No.8/171, Church Street, Only one ID proof attached. Komathimuthupuram Post, Panaiyoor(via) Changarankovil Taluk, Tirunelveli, 627 761. 11 AP-64 S. Arun kannan No. 15D, Poonga Nagar, Kaladipet, Only one ID proof attached. Thiruvottiyur, Ch – 600 019 12 AP-69 K. Lavanya Priyadharshini No, 35, A Block, Nochi Nagar, Mylapore, Only one ID proof attached. Chennai – 600 004 13 AP-70 G. -

S. No. App.No. Name Address 1 AP-6 J.R. Rahul 2 AP-16 K. Pradeep
Accepted list for the post of Reader - BC (OTBCM) (NP) -2 S. No. App.No. Name Address 1 AP-6 J.R. Rahul No.23/61, Gokulam Attingarai, Manavalakurichi, Kanyakumari – 629 252 2 AP-16 K. Pradeep Subramanian No.30, Pandiyan Street, Sundar Nagar, Thirunagar, Madurai – 625 006. 3 AP-30 A. John Antony K.Rasiamangalam(Po.), Alangankudi Taluk, Pudhukottai – 622 301. 4 AP-33 M. Subha Door No.6, 2ndFloor, Vasanth Apartments, C Block, No.1, Maduraiswamy Madam Street, Perambur, Chennai – 600 011. 5 AP-35 R. Vijayalakshmi No.26-A, Sathymoorthy Street, Narimedu, Madurai – 625 002. 6 AP-40 P. Ganesh Old No.L/1229, New No.20, 29thCross Street, Thiruvalluvar Nagar, Thiruvanmiyur, Chennai – 600 041. 7 AP-45 K. Balasubramanian No.6/40, Thiruvalluvar Street, Kuladheepamangalam (Post) Thirukovilur Taluk, Villupuram – 605 756. 8 AP-51 L. Babu No.73/45, Munusamy Street, Ayanavaram, Chennai – 600 023. 9 AP-56 S. Barkavi No.168, Sivaji Nagar, Veerampattinam, Pondicherry – 605 007. 10 AP-62 R.D. Mathanram No.57, Jeeyar Narayanapalayam St, Kanchipuram – 631 501 11 AP-77 M.Parameswari No.8/4, Alagiri Nagar, 1ststreet, Vadapalani, chennai -26. 12 AP-83 G. Selva Kumari No. 12, G Block, Singara thottam, Police Quarters, Old Washermen pet, Chennai 600 021 13 AP-89 P. Mythili No.137/64, Sanjeeviroyan Koil Street, Old Washermenpet, Chennai – 600 021. 14 AP-124 K. Balaji No.11, Muthumariamman Koil Street, Bharath Nagar, Selaiyur, Chennai – 600 073. 15 AP-134 S. Anitha No.5/55-A, Main Road, Siruvangunam, Iraniyasithi Post, Seiyur Taluk, Kancheepuram – 603 312. -

Tiruvallur - District Agricultural Plan
Tiruvallur - District Agricultural Plan Wrapper Project team Foreword Preface Executive Summary Chapter I Chapter II Chapter III Chapter IV Chapter V Chapter VI Meeting Proceedings Photos NATIONAL AGRICULTURAL DEVELOPMENT PROGRAMME (NADP) DISTRICT AGRICULTURE PLAN THIRUVALLUR DISTRICT Centre for Agricultural and Rural Development Studies (CARDS) Tamil Nadu Agricultural University Coimbatore – 641 003 2008 NATIONAL AGRICULTURE DEVELOPMENT PROJECT – DISTRICT AGRICULTURE PLAN PROJECT TEAM Overall Coordination : Dr. K. Palanisami, Director, CARDS and Nodal Officer (NADP) Dr. R. Venkatram, Professor and Principal Coordinator (NADP) District Level : Dr. R. Agila Coordination Associate Professor Dept. of Agrl. Extension and Sociology TNAU, Coimbatore - 3 V. Jeyabal Professor and Head RRS, Tirur G. Sudhakar Assistant Professor RRS, Tirur K. Parasuraman Agricultural Officer Office of the Joint Director of Agriculture, Thiruvallur Thiru. P. Pandian Executive Engineer Department of Agricultural Engneering Thiruvallur district Tmt. Darling Pradeepa Horticulture Officer Cholavaram, Chennai Thiru. K. Nagaraj Asst. Horticulture Officer Ekkadau, Thiruvallur Thiru. J.S. Vijayakumar Deputy Director (Agrl. Marketing) Thiruvallur Thiru. R.K.R. Rajasekar Assistant Executive Engineer, PWD, WRD, Aranian Basin Sub division, Ponneri Tmt. R. Uma Maheswari Assistant Director of Fisheries (marine) Ponneri Tamil Nadu Agricultural University Prof. C.RAMASAMY COIMBATORE-641 003 Vice-Chancellor TAMIL NADU INDIA. FOREWORD Date ........................... The National Development Council resolved that Agricultural Development strategies must be reoriented to meet the needs of farmers and called upon the Central and State governments to evolve a strategy to rejuvenate agriculture with a commitment to achieve four per cent annual growth in the agricultural sector during the 11th plan. The council also recommended special Additional Central Assistance Scheme named National Agriculture Development Programme (NADP) be launched. -

Fact Sheets Fact Sheets
DistrictDistrict HIV/AIDSHIV/AIDS EpidemiologicalEpidemiological PrProfilesofiles developeddeveloped thrthroughough DataData TTriangulationriangulation FFACTACT SHEETSSHEETS MaharastraMaharastra National AIDS Control Organisation India’s voice against AIDS Ministry of Health & Family Welfare, Government of India 6th & 9th Floors, Chandralok Building, 36, Janpath, New Delhi - 110001 www.naco.gov.in VERSION 1.0 GOI/NACO/SIM/DEP/011214 Published with support of the Centers for Disease Control and Prevention under Cooperative Agreement No. 3U2GPS001955 implemented by FHI 360 District HIV/AIDS Epidemiological Profiles developed through Data Triangulation FACT SHEETS Maharashtra National AIDS Control Organisation India’s voice against AIDS Ministry of Health & Family Welfare, Government of India 6th & 9th Floors, Chandralok Building, 36, Janpath, New Delhi - 110001 www.naco.gov.in December 2014 Dr. Ashok Kumar, M.D. F.I.S.C.D & F.I.P.H.A Dy. Director General Tele : 91-11-23731956 Fax : 91-11-23731746 E-mail : [email protected] FOREWORD The national response to HIV/AIDS in India over the last decade has yielded encouraging outcomes in terms of prevention and control of HIV. However, in recent years, while declining HIV trends are evident at the national level as well as in most of the States, some low prevalence and vulnerable States have shown rising trends, warranting focused prevention efforts in specific areas. The National AIDS Control Programme (NACP) is strongly evidence-based and evidence-driven. Based on evidence from ‘Triangulation of Data’ from multiple sources and giving due weightage to vulnerability, the organizational structure of NACP has been decentralized to identified districts for priority attention. The programme has been successful in creating a robust database on HIV/AIDS through the HIV Sentinel Surveillance system, monthly programme reporting data and various research studies. -

The Institute of Road Transport Driver Training Wing, Gummidipundi
THE INSTITUTE OF ROAD TRANSPORT DRIVER TRAINING WING, GUMMIDIPUNDI LIST OF TRAINEES COMPLETED THE HVDT COURSE Roll.No:17SKGU2210 Thiru.BARATH KUMAR E S/o. Thiru.ELANCHEZHIAN D 2/829, RAILWAY STATION ST PERUMAL NAICKEN PALAYAM 1 8903739190 GUMMIDIPUNDI MELPATTAMBAKKAM PO,PANRUTTI TK CUDDALORE DIST Pincode:607104 Roll.No:17SKGU3031 Thiru.BHARATH KUMAR P S/o. Thiru.PONNURENGAM 950 44TH BLOCK 2 SATHIYAMOORTHI NAGAR 9789826462 GUMMIDIPUNDI VYASARPADI CHENNAI Pincode:600039 Roll.No:17SKGU4002 Thiru.ANANDH B S/o. Thiru.BALASUBRAMANIAN K 2/157 NATESAN NAGAR 3 3RD STREET 9445516645 GUMMIDIPUNDI IYYPANTHANGAL CHENNAI Pincode:600056 Roll.No:17SKGU4004 Thiru.BHARATHI VELU C S/o. Thiru.CHELLAN 286 VELAPAKKAM VILLAGE 4 PERIYAPALAYAM PO 9789781793 GUMMIDIPUNDI UTHUKOTTAI TK THIRUVALLUR DIST Pincode:601102 Roll.No:17SKGU4006 Thiru.ILAMPARITHI P S/o. Thiru.PARTHIBAN A 133 BLA MURUGAN TEMPLE ST 5 ELAPAKKAM VILLAGE & POST 9952053996 GUMMIDIPUNDI MADURANDAGAM TK KANCHIPURAM DT Pincode:603201 Roll.No:17SKGU4008 Thiru.ANANTH P S/o. Thiru.PANNEER SELVAM S 10/191 CANAL BANK ROAD 6 KASTHURIBAI NAGAR 9940056339 GUMMIDIPUNDI ADYAR CHENNAI Pincode:600020 Roll.No:17SKGU4010 Thiru.VIJAYAKUMAR R S/o. Thiru.RAJENDIRAN TELUGU COLONY ROAD 7 DEENADAYALAN NAGAR 9790303527 GUMMIDIPUNDI KAVARAPETTAI THIRUVALLUR DIST Pincode:601206 Roll.No:17SKGU4011 Thiru.ULIS GRANT P S/o. Thiru.PANNEER G 68 THAYUMAN CHETTY STREET 8 PONNERI 9791745741 GUMMIDIPUNDI THIRUVALLUR THIRUVALLUR DIST Pincode:601204 Roll.No:17SKGU4012 Thiru.BALAMURUGAN S S/o. Thiru.SUNDARRAJAN N 23A,EGAMBARAPURAM ST 9 BIG KANCHEEPURAM 9698307081 GUMMIDIPUNDI KANCHEEPURAM DIST Pincode:631502 Roll.No:17SKGU4014 Thiru.SARANRAJ M S/o. Thiru.MUNUSAMY K 5 VOC STREET 10 DR. -

Administrative Units of Maharashtra, Download PDF in English
www.gradeup.co Administrative Units of Maharashtra Administrative divisions are an integral part of the state. There is an extended network of smaller administrative units or territories with lesser control for better and effective governance. They work in a coordinated and hierarchical manner. Hence, the administrative division includes dependent territories and accepted administrative divisions. In India, the state of Maharashtra lies in the western and central part of the country. The state has a long coastline (720 km) along the Arabian Sea. • Maharashtra came into existence on 1 May 1960; the day is observed as Maharashtra Day. These districts are grouped into six administrative divisions shown below. • Based on the population, Maharashtra is the second largest state in India and 3rd in terms of geographical extent. • As per Census 2011, 9.3% of the total population resides in Maharashtra, and the state is highly urbanized, with 45.2% people live in urban areas. • Maharashtra has 35 districts, divided into six revenue divisions, i.e., Aurangabad, Amravati, Konkan, Pune, Nashik, and Nagpur, for administrative purposes. • Maharashtra has five central regions based on geographical, political, historical and cultural sentiments. These are: 1. Konkan 2. Desh (Pune Division) 3. Khandesh 4. Marathwada 5. Vidarbha • Note: Maharashtra has a long tradition of having statutory bodies for planning at the district level. • To govern the rural areas for effective local self-governance, there are 33 Zilla Parishads, 351 Panchayat Samitis and 27,906 -

July 2015–December 2015
ACUITAS-The Journal of Management ACUITAS The Journal of Management Research Volume VI Issue-II July 2015–December 2015 Vol VI, Issue-II, (July-December, 2015) Page 1 ACUITAS-The Journal of Management ACUITAS - The Journal of Management Research Volume VI Issue-I January 2015–June 2015 Patron: Bhadant Arya Nagarjuna Shurei Sasai Chairman, P.P. Dr. Babasaheb Ambedkar Smarak Samiti, Deeksha Bhoomi, Nagpur Shri. S.J. Fulzele Secretary, P.P. Dr. Babasaheb Ambedkar Smarak Samiti, Deeksha Bhoomi, Nagpur Advisory Board: Dr. Vilas Chopde, Vice-Principal, Dr. Ambedkar College, Nagpur Capt. C.M. Chitale, Dean, Faculty of management, Savitribai Phule Pune University Dr. Babanrao Taywade, Dean, Faculty of Commerce, RTM Nagpur, University, Nagpur Editorial Board: Dr. Sudhir Fulzele, Director, Dr. Babasaheb Ambedkar Institute of Management Studies and Research, Nagpur Dr. S.G. Metre, Professor, Dr. BabasahebAmbedkar Institute of Management Studies and Research, Nagpur Dr. Charles Vincent, Professor, Centrum Catolica, Pontificia Universidad Catalica de Peru, South Africa Dr. S.S. Kaptan, Head of the Department and Research Centre, Savitribai Phule Pune University Dr. V.S. Deshpande, Professor, Department of Business Management, RTM Nagpur University, Dr. D.Y. Chacharkar, Reader, SGB Amravati University Dr. S.B. Sadar, Head of the Department, Department of Business Management, SGB Amravati University Dr. J.K. Nandi, Associate Dean, IBS, Nagpur Dr. Anil Pathak, Assistant Professor, MDI, Gurgaon Mr. Sangeet Gupta, Managing Director, Synapse World Wide, Canberra, Australia Ms. Sanchita Kumar, GM-HRD, Diffusion Engineering Ltd. Vol VI, Issue-II, (July-December, 2015) Page 2 ACUITAS-The Journal of Management Editorial Committee: Dr. Nirzar Kulkarni Executive Editor Dr. -

Journal 33.Pdf
1 GOVERNMENT OF INDIA GEOGRAPHICAL INDICATIONS JOURNAL NO. 33 APRIL 30, 2010 / VAISAKHA 2, SAKA 1932 2 INDEX Page S.No. Particulars No. 1. Official Notices 4 2. G.I Application Details 5 3. Public Notice 11 4. Sandur Lambani Embroidery 12 5. Hand Made Carpet of Bhadohi 31 6. Paithani Saree & Fabrics 43 7. Mahabaleshwar Strawberry 65 8. Hyderabad Haleem 71 9. General Information 77 10. Registration Process 81 3 OFFICIAL NOTICES Sub: Notice is given under Rule 41(1) of Geographical Indications of Goods (Registration & Protection) Rules, 2002. 1. As per the requirement of Rule 41(1) it is informed that the issue of Journal 33 of the Geographical Indications Journal dated 30th April 2010 / Vaisakha 2, Saka 1932 has been made available to the public from 30th April 2010. 4 G.I. Geographical Indication Class Goods App.No. 1 Darjeeling Tea (word) 30 Agricultural 2 Darjeeling Tea (Logo) 30 Agricultural 3 Aranmula Kannadi 20 Handicraft 24, 25 & 4 Pochampalli Ikat Textile 27 5 Salem Fabric 24 Textile 6 Payyannur Pavithra Ring 14 Handicraft 7 Chanderi Fabric 24 Textile 8 Solapur Chaddar 24 Textile 9 Solapur Terry Towel 24 Textile 10 Kotpad Handloom fabric 24 Textile 24, 25 & 11 Mysore Silk Textile 26 12 Kota Doria 24 & 25 Textile 13 Mysore Agarbathi 3 Manufactured 14 Basmati Rice 30 Agricultural 15 Kancheepuram Silk 24 & 25 Textile 16 Bhavani Jamakkalam 24 Textile 17 Navara - The grain of Kerala 30 Agricultural 18 Mysore Agarbathi "Logo" 3 Manufactured 19 Kullu Shawl 24 Textile 20 Bidriware 6, 21 & 34 Handicraft 21 Madurai Sungudi Saree 24 & 25 -

Some Wild Edible Plants of Malegaon Region from Nashik District, (Maharashtra) Dr
www.ijcrt.org © 2020 IJCRT | Volume 8, Issue 3 March 2020 | ISSN: 2320-2882 Some Wild Edible Plants of Malegaon Region from Nashik District, (Maharashtra) Dr. N. B. Pawar P.G. Department of Botany, L.V. H. College, Panchvati, Nashik Abstract The present study of wild edible plants of Malegaon region from Nashik district contains 19 species belonging to 19 Genera and 16 Families. The wild plants are rich in vitamins and nutrients, many times this plants used by tribal peoples to cure various diseases. Root, Stem, Leaves, Flowers, Fruits and seeds are used to cook. Different tribes have different methodologies and recipes to use the wild plants. The tribals have good knowledge of these plants with their medicinal properties. Key words – Vitamins, Recipes, Tribals Introduction Wild edible plants are a part of the cultural and genetic heritage of various regions of the planet. These are the interesting sources of micronutrients and bioactive compounds. Wild Edible Plants are still consumed traditionally by different communities and are gaining relevance in modern era. Wild edible plants are existing within the forests, protected areas, rural domicile sites, wetlands and grasslands which may be used as food through appropriate means of collection, preparation and preservation. The edible wild plants are greatly valued throughout the region and show a crucial source of non-conventional food for indigenous communities. Wild edible plants increase the nutritional quality of rural diets as an example, micronutrients (vitamins and minerals) which are sometimes superior to those of domesticated varieties. Wild edible plants also constitute the part of natural vegetation and maintain the ecological balance of the forest.