Pharmacovigilance Advancements
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Drug Safety in Translational Paediatric Research: Practical Points to Consider for Paediatric Safety Profiling and Protocol Development: a Scoping Review
pharmaceutics Review Drug Safety in Translational Paediatric Research: Practical Points to Consider for Paediatric Safety Profiling and Protocol Development: A Scoping Review Beate Aurich 1 and Evelyne Jacqz-Aigrain 1,2,* 1 Department of Pharmacology, Saint-Louis Hospital, 75010 Paris, France; [email protected] 2 Paris University, 75010 Paris, France * Correspondence: [email protected] Abstract: Translational paediatric drug development includes the exchange between basic, clinical and population-based research to improve the health of children. This includes the assessment of treatment related risks and their management. The objectives of this scoping review were to search and summarise the literature for practical guidance on how to establish a paediatric safety specification and its integration into a paediatric protocol. PubMed, Embase, Web of Science, and websites of regulatory authorities and learned societies were searched (up to 31 December 2020). Retrieved citations were screened and full texts reviewed where applicable. A total of 3480 publica- tions were retrieved. No article was identified providing practical guidance. An introduction to the practical aspects of paediatric safety profiling and protocol development is provided by combining health authority and learned society guidelines with the specifics of paediatric research. The paedi- atric safety specification informs paediatric protocol development by, for example, highlighting the Citation: Aurich, B.; Jacqz-Aigrain, E. need for a pharmacokinetic study prior to a paediatric trial. It also informs safety related protocol Drug Safety in Translational Paediatric Research: Practical Points sections such as exclusion criteria, safety monitoring and risk management. In conclusion, safety to Consider for Paediatric Safety related protocol sections require an understanding of the paediatric safety specification. -
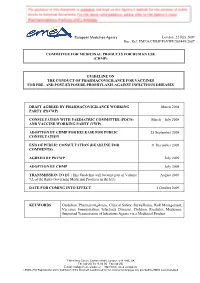
Guideline on the Conduct of Pharmacovigilance for Vaccines for Pre- and Post-Exposure Prophylaxis Against Infectious Diseases
European Medicines Agency London, 22 July 2009 Doc. Ref. EMEA/CHMP/PhVWP/503449/2007 COMMITTEE FOR MEDICINAL PRODUCTS FOR HUMAN USE (CHMP) GUIDELINE ON THE CONDUCT OF PHARMACOVIGILANCE FOR VACCINES FOR PRE- AND POST-EXPOSURE PROPHYLAXIS AGAINST INFECTIOUS DISEASES DRAFT AGREED BY PHARMACOVIGILANCE WORKING March 2008 PARTY (PhVWP) CONSULTATION WITH PAEDIATRIC COMMITTEE (PDCO) March – July 2008 AND VACCINE WORKING PARTY (VWP) ADOPTION BY CHMP FOR RELEASE FOR PUBLIC 25 September 2008 CONSULTATION END OF PUBLIC CONSULTATION (DEADLINE FOR 31 December 2008 COMMENTS) AGREED BY PhVWP July 2009 ADOPTION BY CHMP July 2009 TRANSMISSION TO EC (This Guideline will become part of Volume August 2009 9A of the Rules Governing Medicinal Products in the EU). DATE FOR COMING INTO EFFECT 1 October 2009 KEYWORDS Guideline, Pharmacovigilance, Clinical Safety, Surveillance, Risk Management, Vaccines, Immunisation, Infectious Diseases, Children, Paediatric Medicines, Suspected Transmission of Infectious Agents via a Medicinal Product 7 Westferry Circus, Canary Wharf, London, E14 4HB, UK Tel. (44-20) 74 18 84 00 Fax (44-20) E-mail: [email protected] http://www.emea.europa.eu ©EMEA 2009 Reproduction and/or distribution of this document is authorised for non commercial purposes only provided the EMEA is acknowledged GUIDELINE ON THE CONDUCT OF PHARMACOVIGILANCE FOR VACCINES FOR PRE- AND POST-EXPOSURE PROPHYLAXIS AGAINST INFECTIOUS DISEASES TABLE OF CONTENTS EXECUTIVE SUMMARY_______________________________________________________ 3 1. Introduction ____________________________________________________________ -

Guidance for Industry E2E Pharmacovigilance Planning
Guidance for Industry E2E Pharmacovigilance Planning U.S. Department of Health and Human Services Food and Drug Administration Center for Drug Evaluation and Research (CDER) Center for Biologics Evaluation and Research (CBER) April 2005 ICH Guidance for Industry E2E Pharmacovigilance Planning Additional copies are available from: Office of Training and Communication Division of Drug Information, HFD-240 Center for Drug Evaluation and Research Food and Drug Administration 5600 Fishers Lane Rockville, MD 20857 (Tel) 301-827-4573 http://www.fda.gov/cder/guidance/index.htm Office of Communication, Training and Manufacturers Assistance, HFM-40 Center for Biologics Evaluation and Research Food and Drug Administration 1401 Rockville Pike, Rockville, MD 20852-1448 http://www.fda.gov/cber/guidelines.htm. (Tel) Voice Information System at 800-835-4709 or 301-827-1800 U.S. Department of Health and Human Services Food and Drug Administration Center for Drug Evaluation and Research (CDER) Center for Biologics Evaluation and Research (CBER) April 2005 ICH Contains Nonbinding Recommendations TABLE OF CONTENTS I. INTRODUCTION (1, 1.1) ................................................................................................... 1 A. Background (1.2) ..................................................................................................................2 B. Scope of the Guidance (1.3)...................................................................................................2 II. SAFETY SPECIFICATION (2) ..................................................................................... -

Public/Community Health Nursing Orientation 1 © 2004 NYSNA All Rights Reserved
Public/Community Health Nursing Orientation NYSNA Continuing Education The New York State Nurses Association is accredited as a provider of continuing nursing education by the American Nurses Credentialing Center’s Commission on Accreditation. This course has been awarded 9.6 contact hours. All American Nurses Credentialing Center (ANCC) accredited organizations' contact hours are recognized by all other ANCC accredited organizations. Most states with mandatory continuing education requirements recognize the ANCC accreditation/approval system. Questions about the acceptance of ANCC contact hours to meet mandatory regulations should be directed to the professional licensing board within that state. NYSNA has been granted provider status by the Florida State Board of Nursing as a provider of continuing education in nursing (Provider number 50-1437). How to Take This Course Please take a look at the steps below; these will help you to progress through the course material, complete the course examination and receive your certificate of completion. 1. REVIEW THE OBJECTIVES The objectives provide an overview of the entire course and identify what information will be focused on. Objectives are stated in terms of what you, the learner, will know or be able to do upon successful completion of the course. They let you know what you should expect to learn by taking a particular course and can help focus your study. 2. STUDY EACH SECTION IN ORDER Keep your learning "programmed" by reviewing the materials in order. This will help you understand the sections that follow. 3. COMPLETE THE COURSE EXAM After studying the course, click on the "Course Exam" option located on the course navigation toolbar. -

PUBLIC HEALTH and PUBLIC HEALTH NURSING by David J
POSITION PAPER PUBLIC HEALTH AND PUBLIC HEALTH NURSING By David J. Reyes, DNP, MPH, RN, PHNA-BC White paper: Public health Page 1 POSITION STATEMENT The Washington State Nurses Association (WSNA) recommends allocation of sustainable funding and resources in the public health system and workforce in order to provide essential and Foundational Public Health Services, address the underlying causes of preventable illness and disease, improve population health, and achieve health equity. WSNA recognizes the leadership role of public health nurses in achieving these aims and calls for sustainable investments in public health nursing education, practice and research that supports and builds the capacity of qualified public health nurses to address contemporary and future public health challenges and priorities. OVERVIEW Despite efforts to reform the nation’s health system, improving Since the Great Recession (2008-2016), continued decreases overall population health remains a significant challenge as in financial resources have compounded LHJ’s capacity to persons of all ages in the U.S. continue to experience gaps and/ effectively respond to current and future public health prior- or lack of health insurance coverage (Martinez, Zammitti & ities, including emerging infectious diseases, substance use, Cohen, 2018). While uninsured rates vary, the overall numbers and other non-communicable diseases (National Association of insured persons have decreased since 2014, in particular of County & City Health Officials, 2017). Concurrently, LHJ’s due to reforms of the Affordable Care Act (Keith, 2019). At the have experienced a total workforce decline of 21%, repre- same time population health outcomes, particularly among senting a 20% reduction in full-time equivalent staff capacity. -

Ecological Impacts of Veterinary Pharmaceuticals: More Transparency – Better Protection of the Environment
Ecological Impacts of Veterinary Pharmaceuticals: More Transparency – Better Protection of the Environment Avoiding Environmental Pollution from Veterinary Pharmaceuticals To reduce the contamination of air, soil, and bodies of pharmaceuticals more stringently, monitoring systematically water caused by veterinary medicinal products used in their occurrence in the environment, converting animal hus- agriculture and livestock farming, effective measures bandry practices to preserve animals’ health with a minimal must be taken throughout the entire life cycle of these use of antibiotics, and enforcing legal regulations to ensure products – from production and authorisation to appli- implementation of all the measures outlined here. cation and disposal. In the context of the revision of veterinary medicinal products All stakeholders – whether they are farmers, veterinarians, legislation that is currently underway, this background paper consumers, or political decision makers – are called upon focuses on three measures that would contribute to mak- to contribute to reducing contamination of the environment ing information on the occurrence of veterinary drugs in the caused by pharmaceutical residues and to improving pro- environment and their eco-toxicological effects more widely tection of the environment and human health. Appropriate available and enhance protection of the environment from measures include establishing “clean” production plants, contamination with veterinary pharmaceuticals. developing pharmaceuticals with reduced environmental -

Enhancing the Role of Community Health Nursing for Universal Health Coverage
ENHANCING THE ROLE OF COMMUNITY HEALTH NURSING FOR UNIVERSAL HEALTH COVERAGE Human Resources for Health Observer Series No. 18 Health Workforce Department World Health Organization 20 Avenue Appia CH 1211 Geneva 27 Switzerland www.who.int/hrh ISBN 978 92 4 15118969 Series No. 18 A Human Resources for Health Observer B ENHANCING THE ROLE OF COMMUNITY HEALTH NURSING FOR UNIVERSAL HEALTH COVERAGE Human Resources for Health Observer Series No. 18 Series No. 18 i Human Resources for Health Observer Enhancing the role of community health nursing for universal health coverage Human Resources for Health Observer Series No. 18 ISBN 978-92-4-151189-6 © World Health Organization 2017 Some rights reserved. This work is available under the Creative Commons Attribution-NonCommercial-ShareAlike 3.0 IGO licence (CC BY-NC-SA 3.0 IGO; https://creativecommons.org/licenses/by-nc-sa/3.0/igo). Under the terms of this licence, you may copy, redistribute and adapt the work for non-commercial purposes, provided the work is appropriately cited, as indicated below. In any use of this work, there should be no suggestion that WHO endorses any specific organization, products or services. The use of the WHO logo is not permitted. If you adapt the work, then you must license your work under the same or equivalent Creative Commons licence. If you create a translation of this work, you should add the following disclaimer along with the suggested citation: “This translation was not created by the World Health Organization (WHO). WHO is not responsible for the content or accuracy of this translation. -

1 Public Health Nurse Orientation Section II: Immunizations Learning
Public Health Nurse Orientation Learning Objectives Services to Prevent and Control Communicable Disease After completing the module, participants should be able to: Section II: • AlApply sa fife immun itiization prac titthitices to their Immunizations own nursing practice • Locate resources to guide safe immunization practice 23 24 Wisconsin Division of Public Health Immunizations Immunization Program Healthy People 2010 Objective: Vision: To eliminate vaccine preventable Achieve and maintain effective vaccination coverage levels for universally recommended vaccines among disease through immunization. young children: 90% 25 Website: http://dhfs.wisconsin.gov/immunization/aboutus.htm 26 Immunization Definitions and Terms Safe Immunization Practice • Acellular vaccine • Immunity • Adjuvants • Immunization • Primary Prevention • Advisory Committee on Immunization • Immunosupression Inactive vaccine Practices (ACIP): • Incidence • Anaphylaxis • Incubation period • Delegated Function • Antibody •Isolation • Antigens • Live vaccine – Wisconsin Statute Chapter 441 • Antitoxin • Pandemic • Antiviral • Passive immunity • Attenuated vaccine • Polysaccharide vaccines • Community immunity • Quarantine • Combination vaccine • Recombinant • Conjugate vaccine • Seroconversion • Contraindication. • Susceptible •Efficacy rate • Titer (Immune Status Test) • Excipient • Vaccination • Guillain-Barre Syndrome (GBS) • Vaccine • Immune globulin • Waning Immunity http://nxt.legis.state.wi.us/nxt/gateway.dll/?f=templates&fn=default.htm 27 28 1 Wisconsin Immunization -

Unlocking the Power of Pharmacovigilance* an Adaptive Approach to an Evolving Drug Safety Environment
Unlocking the power of pharmacovigilance* An adaptive approach to an evolving drug safety environment PricewaterhouseCoopers’ Health Research Institute Contents Executive summary 01 Background 02 The challenge to the pharmaceutical industry 02 Increased media scrutiny 02 Greater regulatory and legislative scrutiny 04 Investment in pharmacovigilance 05 The reactive nature of pharmacovigilance 06 Unlocking the power of pharmacovigilance 07 Organizational alignment 07 Operations management 07 Data management 08 Risk management 10 The three strategies of effective pharmacovigilance 11 Strategy 1: Align and clarify roles, responsibilities, and communications 12 Strategy 2: Standardize pharmacovigilance processes and data management 14 Strategy 3: Implement proactive risk minimization 20 Conclusion 23 Endnotes 24 Glossary 25 Executive summary The idea that controlled clinical incapable of addressing shifts in 2. Standardize pharmacovigilance trials can establish product safety public expectations and regulatory processes and data management and effectiveness is a core principle and media scrutiny. This reality has • Align operational activities across of the pharmaceutical industry. revealed issues in the four areas departments and across sites Neither the clinical trials process involved in patient safety operations: • Implement process-driven standard nor the approval procedures of the organizational alignment, operations operating procedures, work U.S. Food and Drug Administration management, data management, and instructions, and training -

Causality in Pharmacoepidemiology and Pharmacovigilance: a Theoretical Excursion
DOI: 10.1590/1980-5497201700030010 ARTIGO ORIGINAL / ORIGINAL ARTICLE Causalidade em farmacoepidemiologia e farmacovigilância: uma incursão teórica Causality in Pharmacoepidemiology and Pharmacovigilance: a theoretical excursion Daniel Marques MotaI,II, Ricardo de Souza KuchenbeckerI RESUMO: O artigo teceu algumas considerações sobre causalidade em farmacoepidemiologia e farmacovigilância. Inicialmente, fizemos uma breve introdução sobre a importância do tema, ressaltando que o entendimento da relação causal é considerado como uma das maiores conquistas das ciências e que tem sido, ao longo dos tempos, uma preocupação contínua e central de filósofos e epidemiologistas. Na sequência, descrevemos as definições e os tipos de causas, demonstrando suas influências no pensamento farmacoepidemiológico. Logo a seguir, apresentamos o modelo multicausal de Rothman como um dos fundantes para a explicação da causalidade múltipla, e o tema da determinação da causalidade. Concluímos com alguns comentários e reflexões sobre causalidade na perspectiva da vigilância sanitária, particularmente, para as ações de regulação em farmacovigilância. Palavras-chave: Aplicações da epidemiologia. Causalidade. Efeitos colaterais e reações adversas relacionados a medicamentos. Farmacoepidemiologia. Farmacovigilância. Vigilância sanitária. IPrograma de Pós-Graduação em Epidemiologia, Faculdade de Medicina, Universidade Federal do Rio Grande do Sul – Porto Alegre (RS), Brasil. IIAgência Nacional de Vigilância Sanitária – Brasília (DF), Brasil. Autor correspondente: Daniel Marques Mota. Programa de Pós-Gradução em Epidemiologia da Faculdade de Medicina da Universidade Federal do Rio Grande do Sul. Rua Ramiro Barcelos, 2.400, 2º andar, CEP: 90035-003, Porto Alegre, RS, Brasil. E-mail: [email protected] Conflito de interesses: nada a declarar – Fonte de financiamento: nenhuma. 475 REV BRAS EPIDEMIOL JUL-SET 2017; 20(3): 475-486 MOTA, D.M., KUCHENBECKER, R.S. -

Public Health Nurse
PUBLIC HEALTH Public Health Nurse DEFINITION Position includes, but is not limited to promoting and protecting the health of and preventing disease in the Town’s population, performing highly responsible professional nursing duties in a variety of public health programs, observing and evaluating the physical and emotional conditions of patients, conducting investigations of communicable diseases, and making home visits. ESSENTIAL FUNCTIONS The essential functions or duties listed below are intended only as illustrations of the various type of work that may be performed. The omission of specific statements of duties does not exclude them from the position if the work is similar, related, or a logical assignment to the position. Administers prescribed medications, immunizations and TB screenings and educates clients on doses, mechanism of action, interactions and potential side effects. Monitors clients for adverse reactions and responds according to established standards of care. Coordinates programs, services and other activities to promote wellness, prevent disease, including planning, scheduling and overseeing the annual health fair, safety fair and influenza vaccination clinics throughout Town; trains and supervises all public health nursing staff and volunteers to assigned roles. Monitors state communicable disease information system (MAVEN), and conducts investigations in accordance with state laws and regulations. Conducts isolation and quarantine as necessary to protect community at large. Maintains variety of files, documents and data systems; prepares, maintains and updates client records, vendor invoices, billing statements, including billing for vaccines, supplies, reports; remains compliant with HIPAA/state laws and regulations. FLSA Non- Exempt 355 – G August 2017 1 Develops programs that support individual and community health effort, including planning, scheduling and conducting health clinics, health fairs, home visits, telephone consults, emergency preparedness trainings, exercises and drills. -
Learning Guide: Public Health Nursing Practice for the 21St Century
PUBLIC HEALTH NURSING PRACTICE ST FOR THE 21 CENTURY National Satellite Learning Conference Learning Guide PUBLIC HEALTH NURSING PRACTICE FOR THE 21 ST CENTURY: COMPETENCY DEVELOPMENT IN POPULATION- BASED PRACTICE Learning Guide Minnesota Department of Health Community Health Services Division Section of Public Health Nursing 121 East 7th Place, St. Paul, MN 55164 Phone 651-296-6567 This project was supported by a grant to the Minnesota Department of Health from the Division of Nursing, Bureau of Health Professions, Health Resources and Services Administration at the Department of Health and Human Services, grant #6 D10 HP 30392. Suggested citation: Public Health Nursing Section, Minnesota Department of Health. (2000). Public Health Nursing Practice for the 21st Century; Competency Development in Population-based Practice. St. Paul, MN. Table of Contents INTRODUCTION 1 SESSION 1 SESSION 3 Learning Objectives 5 Learning Objectives 65 Content 5 Content 65 Content Outline 7 Content Outline 67 Learner Materials 11 Learner Materials 69 Handout 1 – Population-based Practice 12 Handout 1 – Public Health Nursing Process 70 Handout 2 – Levels of Prevention 14 Handout 2 – Examples from Practice 72 Handout 3 – Levels of Practice 15 Handout 3 – Discussion Questions 73 Handout 4 – Definitions of Public Health Interventions 16 Handout 4 – Selected Resources 74 Handout 5 – Discussion Questions 19 Pre test 76 Pre test 20 Post test 78 Post test 22 SESSION 2 Learning Objectives 25 BIOGRAPHICAL SKETCHES 81 Content 26 Laurel Briske 82 Content Outline 27