A Closer Look at Nitric Oxide in Glaucoma James C. T
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

2018 Department of Ophthalmology Chair Report
SAVE THE▼ DATE Department of 200 Ophthalmology Years www.NYEE.edu Anniversary SPECIALTY REPORT | FALL 2018 www.NYEE.edu Celebration Join us for 200 Years and Counting: Bicentennial Cocktail Celebration October 15, 2020 Research Breakthrough: The Plaza 768 5th Avenue Gene Transfer New York, NY Therapy Restores 200 Years and Counting: Ophthalmology Vision in Mice Symposium October 16, 2020 Stay tuned for details on tickets and registration information. Cover image: Slice of a central retina section showing all layers (ONL, INL, GCL). Red indicates rod photoreceptors, located in outer nuclear layer (ONL). Green indicates Müller glial cells, whose cell bodies are located in inner nuclear layer (INL), and their branches across all three layers. Dark blue indicates the nucleus of all cells in three layers (GCL). Icahn School of Medicine at Medical Directors Neuro-Ophthalmology Uveitis and Ocular Immunology Mount Sinai Departmental Mark Kupersmith, MD Douglas Jabs, MD, MBA Avnish Deobhakta, MD Leadership System Chief, System Chief, Uveitis and Ocular Medical Director, NYEE - Neuro-Ophthalmology, Immunology, MSHS James C. Tsai, MD, MBA East 85th Street MSHS President, NYEE Stephanie Llop, MD System Chair, Department of Robin N. Ginsburg, MD 3 Message From the System Chair of the DepartmentValerie Elmalem, of Ophthalmology MD Sophia Saleem, MD Ophthalmology, MSHS Medical Director, NYEE- Joel Mindel, MD East 102nd Street Louis4 R. Pasquale,Breaking MD New Ground in Gene Transfer Therapy to Restore Vision Affiliated Leadership Ocular Oncology Site Chair, Department of Gennady Landa, MD Paul Finger, MD Ebby Elahi, MD, MBA Ophthalmology, MSH and MSQ Medical Director, NYEE- 6 This i-Doctor Is Transforming the Field of Ophthalmology President, NYEE/MSH System Vice Chair, Translational Williamsburg and Tribeca Ophthalmic Pathology Ophthalmology Alumni Ophthalmology Research, MSHS Jodi Sassoon, MD Society Kira Manusis, MD Inside Feature Site Chair, Pathology, NYEE Medical Director, NYEE- Paul A. -
RETINAL DISORDERS Eye63 (1)
RETINAL DISORDERS Eye63 (1) Retinal Disorders Last updated: May 9, 2019 CENTRAL RETINAL ARTERY OCCLUSION (CRAO) ............................................................................... 1 Pathophysiology & Ophthalmoscopy ............................................................................................... 1 Etiology ............................................................................................................................................ 2 Clinical Features ............................................................................................................................... 2 Diagnosis .......................................................................................................................................... 2 Treatment ......................................................................................................................................... 2 BRANCH RETINAL ARTERY OCCLUSION ................................................................................................ 3 CENTRAL RETINAL VEIN OCCLUSION (CRVO) ..................................................................................... 3 Pathophysiology & Etiology ............................................................................................................ 3 Clinical Features ............................................................................................................................... 3 Diagnosis ......................................................................................................................................... -

UCSF Ophthalmology Advice Guide Authors: Seanna Grob, MD, MAS
UCSF Ophthalmology Advice Guide Authors: Seanna Grob, MD, MAS and Neeti Parikh, MD Hello! We are excited that you are interested in ophthalmology! It is truly a special field in medicine. From saving someone’s vision after severe eye trauma, to restoring vision with cataract, retina, or cornea surgery, to preserving someone’s vision with glaucoma management and surgery, to reconstructing someone’s periocular area after trauma, burns, or tumor removal, amazing things can happen in ophthalmology. Ophthalmologists love their job and the majority say they would pick this specialty again if they had the choice. An incredible amount of job satisfaction comes from saving someone’s vision! We are here for you in the UCSF Department of Ophthalmology! We have put together this guide to help you through the process. This guide is meant to be very comprehensive. We want to make sure you are aware of all the opportunities and resources you have so that you can plan accordingly. You do not have to do everything we mention! Please feel free to reach out with questions about the specialty, how to get involved, and how to become a great ophthalmology applicant! 1 Medical School A well-rounded application is important for a successful match and any way you can prove to ophthalmology programs that you are dedicated to the field will be helpful to you. As more objective data (such as grades and board scores become less prevalent) other parts of your application will become more important. Various experiences you seek out are not only fun and educational, but will offer exposure to this wonderful field. -

Ophthalmology Abbreviations Alphabetical
COMMON OPHTHALMOLOGY ABBREVIATIONS Listed as one of America’s Illinois Eye and Ear Infi rmary Best Hospitals for Ophthalmology UIC Department of Ophthalmology & Visual Sciences by U.S.News & World Report Commonly Used Ophthalmology Abbreviations Alphabetical A POCKET GUIDE FOR RESIDENTS Compiled by: Bryan Kim, MD COMMON OPHTHALMOLOGY ABBREVIATIONS A/C or AC anterior chamber Anterior chamber Dilators (red top); A1% atropine 1% education The Department of Ophthalmology accepts six residents Drops/Meds to its program each year, making it one of nation’s largest programs. We are anterior cortical changes/ ACC Lens: Diagnoses/findings also one of the most competitive with well over 600 applicants annually, of cataract whom 84 are granted interviews. Our selection standards are among the Glaucoma: Diagnoses/ highest. Our incoming residents graduated from prestigious medical schools ACG angle closure glaucoma including Brown, Northwestern, MIT, Cornell, University of Michigan, and findings University of Southern California. GPA’s are typically 4.0 and board scores anterior chamber intraocular ACIOL Lens are rarely lower than the 95th percentile. Most applicants have research lens experience. In recent years our residents have gone on to prestigious fellowships at UC Davis, University of Chicago, Northwestern, University amount of plus reading of Iowa, Oregon Health Sciences University, Bascom Palmer, Duke, UCSF, Add power (for bifocal/progres- Refraction Emory, Wilmer Eye Institute, and UCLA. Our tradition of excellence in sives) ophthalmologic education is reflected in the leadership positions held by anterior ischemic optic Nerve/Neuro: Diagno- AION our alumni, who serve as chairs of ophthalmology departments, the dean neuropathy ses/findings of a leading medical school, and the director of the National Eye Institute. -

Relationships Involved Cataract Surgery
"" OPHTHALMOLOGVOPTOMETRY RELATIONSHIPS INVOLVED CATARACT SURGERY +t-" SIIlYICls. l/ ""Ia OFFICE OF INSPECTOR GENERAL OFFICE OF ANALYSIS AND INSPECTIONS APRIL 1989 PHTHALMOLOGVO PTO ETRY RELATIONSHIPS INVOLVED CATARACT SURGERY RICHARD P. KUSSEROW INSPECTOR GENERAL o AI-07 -88-00460 APRIL 1989 EXECUTIVE SUMMARY OBJECTIVES This inspection focuses on issues involving optometrsts ' providing postoperative care to Medicare beneficiares following catat surgery. The overall objectives of the inspection were to detennne: the extent and frequency of postoperative care by optometrsts; the extent of referral arangements between ophthalmologists and optometrsts; the manner of billng by ophthalmologists and optometrsts for cataract surgery when an optometrst provides postoperative car; and whether the practice of optometrsts ' providing cataract surgery postoperative care could lead to abusive referral arrangements, and possible duplicate bilings. BACKGROUND This program inspection was requested by the Administrtor of the Health Care Financing Ad ministration (HCFA), who was concerned about the issue of optometrsts ' providing postopera tive care to Medicare beneficiares who had cataract surgery. This practice increased after Medicare coverage was expanded by the Omnibus Budget Reconciliation Act of 1986. This legislation penntted coverage of optometrsts as physicians for any services they ar legally authorized to perform in the State in which they practice. All 50 States permit optometrsts to use diagnostic drgs. Funher, 23 States have passed legislation allowing optometrsts to use and prescribe therapeutic drugs, greatly expanding their scope of practice and ability to treat patients during the postoperative period following cataract surgery. METHODOLOGY Preinspection work included meetings and contacts with the Americ n Academy of Ophthal mology, the American Optometrc Association, State licensing boards, Medicare carrers, and HCFA staf. -

Acquired Colour Vision Defects in Glaucoma—Their Detection and Clinical Significance
1396 Br J Ophthalmol 1999;83:1396–1402 Br J Ophthalmol: first published as 10.1136/bjo.83.12.1396 on 1 December 1999. Downloaded from PERSPECTIVE Acquired colour vision defects in glaucoma—their detection and clinical significance Mireia Pacheco-Cutillas, Arash Sahraie, David F Edgar Colour vision defects associated with ocular disease have The aims of this paper are: been reported since the 17th century. Köllner1 in 1912 + to provide a review of the modern literature on acquired wrote an acute description of the progressive nature of col- colour vision in POAG our vision loss secondary to ocular disease, dividing defects + to diVerentiate the characteristics of congenital and into “blue-yellow” and “progressive red-green blindness”.2 acquired defects, in order to understand the type of This classification has become known as Köllner’s rule, colour vision defect associated with glaucomatous although it is often imprecisely stated as “patients with damage retinal disease develop blue-yellow discrimination loss, + to compare classic clinical and modern methodologies whereas optic nerve disease causes red-green discrimina- (including modern computerised techniques) for tion loss”. Exceptions to Köllner’s rule34 include some assessing visual function mediated through chromatic optic nerve diseases, notably glaucoma, which are prima- mechanisms rily associated with blue-yellow defects, and also some reti- + to assess the eVects of acquired colour vision defects on nal disorders such as central cone degeneration which may quality of life in patients with POAG. result in red-green defects. Indeed, in some cases, there might be a non-specific chromatic loss. Comparing congenital and acquired colour vision Colour vision defects in glaucoma have been described defects since 18835 and although many early investigations Congenital colour vision deficiencies result from inherited indicated that red-green defects accompanied glaucoma- cone photopigment abnormalities. -

Eugene and Marilyn Glick Eye Institute Ophthalmology Update
Indiana University School of Medicine Eugene and Marilyn Glick Eye Institute Ophthalmology Update Department of Ophthalmology Spring 2013 Research team commits to Glick Eye Institute Vision research at the Eugene and researcher, Maria Grant, M.D., will Translational Research in the Marilyn Glick Eye Institute will receive be the first to hold the new Marilyn K. Department of Ophthalmology at a double boost when husband- Glick Senior Chair. They will join the the University of Florida and holds and-wife research scientists from department on July 1. professorships in ophthalmology; the University of Florida join the physiology and functional genomics; Department of Ophthalmology at the Dr. Boulton is currently director medicine; and psychiatry. Her Indiana University School of Medicine of research and professor in the research focuses on understanding this year. Department of Anatomy and Cell and repairing the damage to blood Biology at the University of Florida. vessels in the eye as a result of Michael Boulton, Ph.D., has been His research has focused on age- diabetes. appointed as the first director of related changes in the retina and basic science research and will hold retinal neovascularization. “We are thrilled to welcome Drs. the Merrill Grayson Senior Chair in Boulton and Grant,” said Louis Ophthalmology; his wife and fellow Dr. Grant is currently director of B. Cantor, M.D., Chairman of the (Continued on page 10) Teen is one of first in Indiana to Read about faculty research, new Department of Ophthalmology fac- participate in an intraocular lens grant awards, publications and ulty travel to Zambia and China implant study. -
Root Eye Dictionary a "Layman's Explanation" of the Eye and Common Eye Problems
Welcome! This is the free PDF version of this book. Feel free to share and e-mail it to your friends. If you find this book useful, please support this project by buying the printed version at Amazon.com. Here is the link: http://www.rooteyedictionary.com/printversion Timothy Root, M.D. Root Eye Dictionary A "Layman's Explanation" of the eye and common eye problems Written and Illustrated by Timothy Root, M.D. www.RootEyeDictionary.com 1 Contents: Introduction The Dictionary, A-Z Extra Stuff - Abbreviations - Other Books by Dr. Root 2 Intro 3 INTRODUCTION Greetings and welcome to the Root Eye Dictionary. Inside these pages you will find an alphabetical listing of common eye diseases and visual problems I treat on a day-to-day basis. Ophthalmology is a field riddled with confusing concepts and nomenclature, so I figured a layman's dictionary might help you "decode" the medical jargon. Hopefully, this explanatory approach helps remove some of the mystery behind eye disease. With this book, you should be able to: 1. Look up any eye "diagnosis" you or your family has been given 2. Know why you are getting eye "tests" 3. Look up the ingredients of your eye drops. As you read any particular topic, you will see that some words are underlined. An underlined word means that I've written another entry for that particular topic. You can flip to that section if you'd like further explanation, though I've attempted to make each entry understandable on its own merit. I'm hoping this approach allows you to learn more about the eye without getting bogged down with minutia .. -

Intraocular Pressure During Phacoemulsification
J CATARACT REFRACT SURG - VOL 32, FEBRUARY 2006 Intraocular pressure during phacoemulsification Christopher Khng, MD, Mark Packer, MD, I. Howard Fine, MD, Richard S. Hoffman, MD, Fernando B. Moreira, MD PURPOSE: To assess changes in intraocular pressure (IOP) during standard coaxial or bimanual micro- incision phacoemulsification. SETTING: Oregon Eye Center, Eugene, Oregon, USA. METHODS: Bimanual microincision phacoemulsification (microphaco) was performed in 3 cadaver eyes, and standard coaxial phacoemulsification was performed in 1 cadaver eye. A pressure transducer placed in the vitreous cavity recorded IOP at 100 readings per second. The phacoemulsification pro- cedure was broken down into 8 stages, and mean IOP was calculated across each stage. Intraocular pressure was measured during bimanual microphaco through 2 different incision sizes and with and without the Cruise Control (Staar Surgical) connected to the aspiration line. RESULTS: Intraocular pressure exceeded 60 mm Hg (retinal perfusion pressure) during both standard coaxial and bimanual microphaco procedures. The highest IOP occurred during hydrodissection, oph- thalmic viscosurgical device injection, and intraocular lens insertion. For the 8 stages of the phaco- emulsification procedure delineated in this study, IOP was lower for at least 1 of the bimanual microphaco eyes compared with the standard coaxial phaco eye in 4 of the stages (hydro steps, nu- clear disassembly, irritation/aspiration, anterior chamber reformation). CONCLUSION: There was no consistent difference in IOP between the bimanual microphaco eyes and the eye that had standard coaxial phacoemulsification. Bimanual microincision phacoemul- sification appears to be as safe as standard small incision phacoemulsification with regard to IOP. J Cataract Refract Surg 2006; 32:301–308 Q 2006 ASCRS and ESCRS Bimanual microincision phacoemulsification, defined as capable of insertion through these microincisions become cataract extraction through 2 incisions of less than 1.5 mm more widely available. -
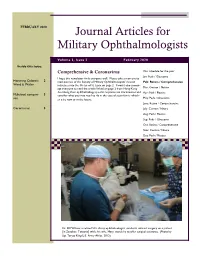
Journal Articles for Military Ophthalmologists
FEBRUARY 2020 Journal Articles for Military Ophthalmologists Volume 3, Issue 2 February 2020 Inside this issue: Comprehensive & Coronavirus Our schedule for the year: Jan: Peds / Glaucoma I hope this newsletter finds everyone well. Please take a moment to Honoring Colonels 2 read out two of the Society of Military Ophthalmologists’ newest Feb: Retina / Comprehensive Ward & Waller inductees into the Order of St. Lucia on page 2. I would also encour- age everyone to read the article linked on page 2 from Hong Kong Mar: Cornea / Neuro describing their ophthalmology-specific responses to Coronavirus and Apr: Path / Plastics Multifocal compari- 3 consider what you may need to do in the case of a pandemic: wheth- May: Peds / Glaucoma son er it be now or in the future. June: Retina / Comprehensive Coronavirus 3 July: Cornea / Neuro Aug: Path / Plastics Sep: Peds / Glaucoma Oct: Retina / Comprehensive Nov: Cornea / Neuro Dec: Path / Plastics Dr. Bill Wilson, a retired U.S. Army ophthalmologist, conducts cataract surgery on a patient [in Zanzibar, Tanzania] while his wife, Mary, stands by to offer surgical assistance. (Photo by Sgt. Terysa King/U.S. Army Africa, 2012) Page 2 Journal Articles for Military Ophthalmologists St Lucia Inductees The Society of Military Ophthalmology is pleased to announce the induction of Stephen Waller, MD, Col, USAF (ret) and Jane Ward, MD, Col, USAF (ret) into the Hon- orable Order of St. Lucia. Thank you for your life-long selfless service on behalf of mili- tary ophthalmology and military medicine, having achieved national and international prominence in the field of Military Medicine, Global Ophthalmology and Global Health Engagement. -

17-2021 CAMI Pilot Vision Brochure
Visual Scanning with regular eye examinations and post surgically with phoria results. A pilot who has such a condition could progress considered for medical certification through special issuance with Some images used from The Federal Aviation Administration. monofocal lenses when they meet vision standards without to seeing double (tropia) should they be exposed to hypoxia or a satisfactory adaption period, complete evaluation by an eye Helicopter Flying Handbook. Oklahoma City, Ok: US Department The probability of spotting a potential collision threat complications. Multifocal lenses require a brief waiting certain medications. specialist, satisfactory visual acuity corrected to 20/20 or better by of Transportation; 2012; 13-1. Publication FAA-H-8083. Available increases with the time spent looking outside, but certain period. The visual effects of cataracts can be successfully lenses of no greater power than ±3.5 diopters spherical equivalent, at: https://www.faa.gov/regulations_policies/handbooks_manuals/ techniques may be used to increase the effectiveness of treated with a 90% improvement in visual function for most One prism diopter of hyperphoria, six prism diopters of and by passing an FAA medical flight test (MFT). aviation/helicopter_flying_handbook/. Accessed September 28, 2017. the scan time. Effective scanning is accomplished with a patients. Regardless of vision correction to 20/20, cataracts esophoria, and six prism diopters of exophoria represent series of short, regularly-spaced eye movements that bring pose a significant risk to flight safety. FAA phoria (deviation of the eye) standards that may not be A Word about Contact Lenses successive areas of the sky into the central visual field. Each exceeded. -
Final Version (2017-06-28) of the Vision Camp
Young Researcher VisionCamp An international Career building Symposium 2017 Castle Wildenstein Leibertingen Germany www.vision-camp.eu Contact: Jugendherberge Burg Wildenstein 88637 Leibertingen-Wildenstein Tel: +49 7466-411 Fax: +49 7466-417 E-Mail: [email protected] www.leibertingen-wildenstein.jugendherberge-bw.de Preamble Dear Colleagues, Dear Participants of the Young Researcher Vision Camp 2017, The aim of this camp is to give young investigators (MSc and PhD students, young MDs and post-docs) an opportunity to present themselves and their work to fellow researchers, to allow them to build and strengthen personal networks in an international environment. Take the time for professional and social networking Take the time for new views on career paths to shape your future Take the time to bridge the gap between basic and clinical research Take the time to revive a medieval castle ENJOY THE YOUNG RESEARCHER VISION CAMP Thomas Wheeler-Schilling on behalf of the organising committee (in alphabetical order) Michaela Bitzer Sigrid Diether Philipp Hunger Norbert Kinkl Arne Ohlendorf Francois Paquet-Durand Vera Schmid Timm Schubert 3 Agenda FRIDAY, JUNE 30th, 2017 until 16:00 Arrival (for details see ‘How to get there’) 16:25 - 16:30 Welcome 16:30 - 17:00 Keynote Lecture I ‘Primary Cilia in the Visual System’ Helen May-Simera 17:00 - 18:00 Scientific Session I: ‘Retinal development and homeo- stasis’ Chair: Jérôme Roger • Elena Braginskaja: “Glycogen Synthase Kinases 3 are Critical for Retinal Develop- ment and Homeostasis”