Flavin-Containing Monooxygenases: Mutations, Disease and Drug Response Phillips, IR; Shephard, EA
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Regulation of Ribulose-1, 5-Bisphosphate Carboxylase
Plant Physiol. (1993) 102: 21-28 Regulation of Ribulose- 1,5-Bisphosphate Carboxylase/Oxygenase Activity in Response to Reduced Light lntensity in C4 Plants' Rowan F. Sage* and Jeffrey R. Seemann Department of Botany, University of Georgia, Athens, Ceorgia 30602 (R.F.S.); and Department of Biochemistry, University of Nevada, Reno, Nevada 89557 (J.R.S.) tion of Rubisco activity by reversible carbamylation occurs in lhe light-dependent regulation of ribulose-1,5-bisphosphate response to changes in light intensity as well as the concen- carboxylase/oxygenase (Rubisco) activity was studied in 16 species tration of C02and 02,whereas inhibition of Rubisco activity of C, plants representing all three biochemical subtypes and a by CAlP occurs only in response to varying PPFD (Sharkey variety of taxonomic groups. Rubisco regulation was assessed by et al., 1986; Sage et al., 1990; Seemann et al., 1990). At measuring (a) the ratio of initial to total Rubisco activity, which physiological levels of COz in C3 plants (5-10 PM), full reflects primarily the carbamylation state of the enzyme, and (b) carbamylation of Rubisco requires Rubisco activase (Salvucci, total Rubisco activity per mo1 of Rubisco catalytic sites, which 1989; Portis, 1990). In the absence of Rubisco activase, only declines when 2-carboxyarabinitol I-phosphate (CAlP) binds to carbamylated Rubisco. In all species examined, the activity ratio of 20 to 40% of Rubisco catalytic sites are carbamylated under Rubisco declined with a reduction in light intensity, although sub- physiological conditions, leading to a significant inhibition of stantial variation was apparent between species in the degree of photosynthesis (Salvucci, 1989; Portis, 1990). -

Upregulation of Peroxisome Proliferator-Activated Receptor-Α And
Upregulation of peroxisome proliferator-activated receptor-α and the lipid metabolism pathway promotes carcinogenesis of ampullary cancer Chih-Yang Wang, Ying-Jui Chao, Yi-Ling Chen, Tzu-Wen Wang, Nam Nhut Phan, Hui-Ping Hsu, Yan-Shen Shan, Ming-Derg Lai 1 Supplementary Table 1. Demographics and clinical outcomes of five patients with ampullary cancer Time of Tumor Time to Age Differentia survival/ Sex Staging size Morphology Recurrence recurrence Condition (years) tion expired (cm) (months) (months) T2N0, 51 F 211 Polypoid Unknown No -- Survived 193 stage Ib T2N0, 2.41.5 58 F Mixed Good Yes 14 Expired 17 stage Ib 0.6 T3N0, 4.53.5 68 M Polypoid Good No -- Survived 162 stage IIA 1.2 T3N0, 66 M 110.8 Ulcerative Good Yes 64 Expired 227 stage IIA T3N0, 60 M 21.81 Mixed Moderate Yes 5.6 Expired 16.7 stage IIA 2 Supplementary Table 2. Kyoto Encyclopedia of Genes and Genomes (KEGG) pathway enrichment analysis of an ampullary cancer microarray using the Database for Annotation, Visualization and Integrated Discovery (DAVID). This table contains only pathways with p values that ranged 0.0001~0.05. KEGG Pathway p value Genes Pentose and 1.50E-04 UGT1A6, CRYL1, UGT1A8, AKR1B1, UGT2B11, UGT2A3, glucuronate UGT2B10, UGT2B7, XYLB interconversions Drug metabolism 1.63E-04 CYP3A4, XDH, UGT1A6, CYP3A5, CES2, CYP3A7, UGT1A8, NAT2, UGT2B11, DPYD, UGT2A3, UGT2B10, UGT2B7 Maturity-onset 2.43E-04 HNF1A, HNF4A, SLC2A2, PKLR, NEUROD1, HNF4G, diabetes of the PDX1, NR5A2, NKX2-2 young Starch and sucrose 6.03E-04 GBA3, UGT1A6, G6PC, UGT1A8, ENPP3, MGAM, SI, metabolism -
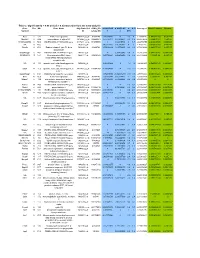
Table 2. Significant
Table 2. Significant (Q < 0.05 and |d | > 0.5) transcripts from the meta-analysis Gene Chr Mb Gene Name Affy ProbeSet cDNA_IDs d HAP/LAP d HAP/LAP d d IS Average d Ztest P values Q-value Symbol ID (study #5) 1 2 STS B2m 2 122 beta-2 microglobulin 1452428_a_at AI848245 1.75334941 4 3.2 4 3.2316485 1.07398E-09 5.69E-08 Man2b1 8 84.4 mannosidase 2, alpha B1 1416340_a_at H4049B01 3.75722111 3.87309653 2.1 1.6 2.84852656 5.32443E-07 1.58E-05 1110032A03Rik 9 50.9 RIKEN cDNA 1110032A03 gene 1417211_a_at H4035E05 4 1.66015788 4 1.7 2.82772795 2.94266E-05 0.000527 NA 9 48.5 --- 1456111_at 3.43701477 1.85785922 4 2 2.8237185 9.97969E-08 3.48E-06 Scn4b 9 45.3 Sodium channel, type IV, beta 1434008_at AI844796 3.79536664 1.63774235 3.3 2.3 2.75319499 1.48057E-08 6.21E-07 polypeptide Gadd45gip1 8 84.1 RIKEN cDNA 2310040G17 gene 1417619_at 4 3.38875643 1.4 2 2.69163229 8.84279E-06 0.0001904 BC056474 15 12.1 Mus musculus cDNA clone 1424117_at H3030A06 3.95752801 2.42838452 1.9 2.2 2.62132809 1.3344E-08 5.66E-07 MGC:67360 IMAGE:6823629, complete cds NA 4 153 guanine nucleotide binding protein, 1454696_at -3.46081884 -4 -1.3 -1.6 -2.6026947 8.58458E-05 0.0012617 beta 1 Gnb1 4 153 guanine nucleotide binding protein, 1417432_a_at H3094D02 -3.13334396 -4 -1.6 -1.7 -2.5946297 1.04542E-05 0.0002202 beta 1 Gadd45gip1 8 84.1 RAD23a homolog (S. -

Somatic Aging Pathways Regulate Reproductive Plasticity in Caenorhabditis Elegans Maria C Ow, Alexandra M Nichitean, Sarah E Hall*
RESEARCH ARTICLE Somatic aging pathways regulate reproductive plasticity in Caenorhabditis elegans Maria C Ow, Alexandra M Nichitean, Sarah E Hall* Department of Biology, Syracuse University, Syracuse, United States Abstract In animals, early-life stress can result in programmed changes in gene expression that can affect their adult phenotype. In C. elegans nematodes, starvation during the first larval stage promotes entry into a stress-resistant dauer stage until environmental conditions improve. Adults that have experienced dauer (postdauers) retain a memory of early-life starvation that results in gene expression changes and reduced fecundity. Here, we show that the endocrine pathways attributed to the regulation of somatic aging in C. elegans adults lacking a functional germline also regulate the reproductive phenotypes of postdauer adults that experienced early-life starvation. We demonstrate that postdauer adults reallocate fat to benefit progeny at the expense of the parental somatic fat reservoir and exhibit increased longevity compared to controls. Our results also show that the modification of somatic fat stores due to parental starvation memory is inherited in the F1 generation and may be the result of crosstalk between somatic and reproductive tissues mediated by the germline nuclear RNAi pathway. Introduction Evidence indicating that experiences during early development affect behavior and physiology in a stress-specific manner later in life is abundant throughout the animal kingdom (Telang and Wells, *For correspondence: [email protected] 2004; Weaver et al., 2004; Binder et al., 2008; Pellegroms et al., 2009; van Abeelen et al., 2012; Zhao and Zhu, 2014; Canario et al., 2017; Dantzer et al., 2019; Vitikainen et al., 2019). -

A Three-Component Dicamba O-Demethylase from Pseudomonas Maltophilia, Strain DI-6 GENE ISOLATION, CHARACTERIZATION, and HETEROLOGOUS EXPRESSION*
THE JOURNAL OF BIOLOGICAL CHEMISTRY Vol. 280, No. 26, Issue of July 1, pp. 24759–24767, 2005 © 2005 by The American Society for Biochemistry and Molecular Biology, Inc. Printed in U.S.A. A Three-component Dicamba O-Demethylase from Pseudomonas maltophilia, Strain DI-6 GENE ISOLATION, CHARACTERIZATION, AND HETEROLOGOUS EXPRESSION* Received for publication, January 18, 2005, and in revised form, March 16, 2005 Published, JBC Papers in Press, April 26, 2005, DOI 10.1074/jbc.M500597200 Patricia L. Herman‡, Mark Behrens, Sarbani Chakraborty, Brenda M. Chrastil, Joseph Barycki, and Donald P. Weeks§ From the Department of Biochemistry, University of Nebraska-Lincoln, Lincoln, Nebraska 65888-0664 Dicamba O-demethylase is a multicomponent enzyme The herbicide dicamba (2-methoxy-3,6-dichlorobenzoic acid) from Pseudomonas maltophilia, strain DI-6, that cata- has been used to effectively control broadleaf weeds in crops lyzes the conversion of the widely used herbicide di- such as corn and wheat for almost 40 years. Like a number of camba (2-methoxy-3,6-dichlorobenzoic acid) to DCSA other chlorinated organic compounds, dicamba does not persist (3,6-dichlorosalicylic acid). We recently described the in the soil because it is efficiently metabolized by a consortium biochemical characteristics of the three components of of soil bacteria under both aerobic and anaerobic conditions this enzyme (i.e. reductaseDIC, ferredoxinDIC, and oxy- (1–4). Studies with different soil types treated with dicamba genaseDIC) and classified the oxygenase component of have demonstrated that 3,6-dichlorosalicylic acid (DCSA),1 a dicamba O-demethylase as a member of the Rieske non- compound without herbicidal activity, is a major product of the heme iron family of oxygenases. -

A Computational Approach for Defining a Signature of Β-Cell Golgi Stress in Diabetes Mellitus
Page 1 of 781 Diabetes A Computational Approach for Defining a Signature of β-Cell Golgi Stress in Diabetes Mellitus Robert N. Bone1,6,7, Olufunmilola Oyebamiji2, Sayali Talware2, Sharmila Selvaraj2, Preethi Krishnan3,6, Farooq Syed1,6,7, Huanmei Wu2, Carmella Evans-Molina 1,3,4,5,6,7,8* Departments of 1Pediatrics, 3Medicine, 4Anatomy, Cell Biology & Physiology, 5Biochemistry & Molecular Biology, the 6Center for Diabetes & Metabolic Diseases, and the 7Herman B. Wells Center for Pediatric Research, Indiana University School of Medicine, Indianapolis, IN 46202; 2Department of BioHealth Informatics, Indiana University-Purdue University Indianapolis, Indianapolis, IN, 46202; 8Roudebush VA Medical Center, Indianapolis, IN 46202. *Corresponding Author(s): Carmella Evans-Molina, MD, PhD ([email protected]) Indiana University School of Medicine, 635 Barnhill Drive, MS 2031A, Indianapolis, IN 46202, Telephone: (317) 274-4145, Fax (317) 274-4107 Running Title: Golgi Stress Response in Diabetes Word Count: 4358 Number of Figures: 6 Keywords: Golgi apparatus stress, Islets, β cell, Type 1 diabetes, Type 2 diabetes 1 Diabetes Publish Ahead of Print, published online August 20, 2020 Diabetes Page 2 of 781 ABSTRACT The Golgi apparatus (GA) is an important site of insulin processing and granule maturation, but whether GA organelle dysfunction and GA stress are present in the diabetic β-cell has not been tested. We utilized an informatics-based approach to develop a transcriptional signature of β-cell GA stress using existing RNA sequencing and microarray datasets generated using human islets from donors with diabetes and islets where type 1(T1D) and type 2 diabetes (T2D) had been modeled ex vivo. To narrow our results to GA-specific genes, we applied a filter set of 1,030 genes accepted as GA associated. -

Regulation of Xenobiotic and Bile Acid Metabolism by the Anti-Aging Intervention Calorie Restriction in Mice
REGULATION OF XENOBIOTIC AND BILE ACID METABOLISM BY THE ANTI-AGING INTERVENTION CALORIE RESTRICTION IN MICE By Zidong Fu Submitted to the Graduate Degree Program in Pharmacology, Toxicology, and Therapeutics and the Graduate Faculty of the University of Kansas in partial fulfillment of the requirements for the degree of Doctor of Philosophy. Dissertation Committee ________________________________ Chairperson: Curtis Klaassen, Ph.D. ________________________________ Udayan Apte, Ph.D. ________________________________ Wen-Xing Ding, Ph.D. ________________________________ Thomas Pazdernik, Ph.D. ________________________________ Hao Zhu, Ph.D. Date Defended: 04-11-2013 The Dissertation Committee for Zidong Fu certifies that this is the approved version of the following dissertation: REGULATION OF XENOBIOTIC AND BILE ACID METABOLISM BY THE ANTI-AGING INTERVENTION CALORIE RESTRICTION IN MICE ________________________________ Chairperson: Curtis Klaassen, Ph.D. Date approved: 04-11-2013 ii ABSTRACT Calorie restriction (CR), defined as reduced calorie intake without causing malnutrition, is the best-known intervention to increase life span and slow aging-related diseases in various species. However, current knowledge on the exact mechanisms of aging and how CR exerts its anti-aging effects is still inadequate. The detoxification theory of aging proposes that the up-regulation of xenobiotic processing genes (XPGs) involved in phase-I and phase-II xenobiotic metabolism as well as transport, which renders a wide spectrum of detoxification, is a longevity mechanism. Interestingly, bile acids (BAs), the metabolites of cholesterol, have recently been connected with longevity. Thus, this dissertation aimed to determine the regulation of xenobiotic and BA metabolism by the well-known anti-aging intervention CR. First, the mRNA expression of XPGs in liver during aging was investigated. -

Identification of Novel CYP2E1 Inhibitor to Investigate Cellular and Exosomal CYP2E1-Mediated Toxicity
University of Tennessee Health Science Center UTHSC Digital Commons Theses and Dissertations (ETD) College of Graduate Health Sciences 6-2019 Identification of Novel CYP2E1 Inhibitor to Investigate Cellular and Exosomal CYP2E1-Mediated Toxicity Mohammad Arifur Rahman University of Tennessee Health Science Center Follow this and additional works at: https://dc.uthsc.edu/dissertations Part of the Pharmacy and Pharmaceutical Sciences Commons Recommended Citation Rahman, Mohammad Arifur (0000-0002-5589-0114), "Identification of Novel CYP2E1 Inhibitor to Investigate Cellular and Exosomal CYP2E1-Mediated Toxicity" (2019). Theses and Dissertations (ETD). Paper 482. http://dx.doi.org/10.21007/etd.cghs.2019.0474. This Dissertation is brought to you for free and open access by the College of Graduate Health Sciences at UTHSC Digital Commons. It has been accepted for inclusion in Theses and Dissertations (ETD) by an authorized administrator of UTHSC Digital Commons. For more information, please contact [email protected]. Identification of Novel CYP2E1 Inhibitor to Investigate Cellular and Exosomal CYP2E1-Mediated Toxicity Abstract Cytochrome P450 2E1 (CYP2E1)-mediated hepatic and extra-hepatic toxicity is of significant clinical importance. Diallyl sulfide (DAS) has been shown to prevent xenobiotics such as alcohol- (ALC/ETH), acetaminophen- (APAP) induced toxicity and disease (e.g. HIV-1) pathogenesis. DAS imparts its beneficial effect by inhibiting CYP2E1-mediated metabolism of xenobiotics, especially at high concentration. However, DAS also causes toxicity at relatively high dosages and with long exposure times. The objective of the first project was to find potent ASD analogs which can replace DAS as a research tool or as potential adjuvant therapy in CYP2E1-mediated pathologies. -

Citric Acid Cycle
CHEM464 / Medh, J.D. The Citric Acid Cycle Citric Acid Cycle: Central Role in Catabolism • Stage II of catabolism involves the conversion of carbohydrates, fats and aminoacids into acetylCoA • In aerobic organisms, citric acid cycle makes up the final stage of catabolism when acetyl CoA is completely oxidized to CO2. • Also called Krebs cycle or tricarboxylic acid (TCA) cycle. • It is a central integrative pathway that harvests chemical energy from biological fuel in the form of electrons in NADH and FADH2 (oxidation is loss of electrons). • NADH and FADH2 transfer electrons via the electron transport chain to final electron acceptor, O2, to form H2O. Entry of Pyruvate into the TCA cycle • Pyruvate is formed in the cytosol as a product of glycolysis • For entry into the TCA cycle, it has to be converted to Acetyl CoA. • Oxidation of pyruvate to acetyl CoA is catalyzed by the pyruvate dehydrogenase complex in the mitochondria • Mitochondria consist of inner and outer membranes and the matrix • Enzymes of the PDH complex and the TCA cycle (except succinate dehydrogenase) are in the matrix • Pyruvate translocase is an antiporter present in the inner mitochondrial membrane that allows entry of a molecule of pyruvate in exchange for a hydroxide ion. 1 CHEM464 / Medh, J.D. The Citric Acid Cycle The Pyruvate Dehydrogenase (PDH) complex • The PDH complex consists of 3 enzymes. They are: pyruvate dehydrogenase (E1), Dihydrolipoyl transacetylase (E2) and dihydrolipoyl dehydrogenase (E3). • It has 5 cofactors: CoASH, NAD+, lipoamide, TPP and FAD. CoASH and NAD+ participate stoichiometrically in the reaction, the other 3 cofactors have catalytic functions. -

TRANSLATIONALLY by AMPK a Dissertation
CHOLESTEROL 7 ALPHA-HYDROXYLASE IS REGULATED POST- TRANSLATIONALLY BY AMPK A dissertation submitted to Kent State University in partial fulfillment of the requirements for the Degree of Doctor of Philosophy By Mauris E.C. Nnamani May 2009 Dissertation written by Mauris E. C. Nnamani B.S, Kent State University, 2006 Ph.D., Kent State University, 2009 Approved by Diane Stroup Advisor Gail Fraizer Members, Doctoral Dissertation Committee S. Vijayaraghavan Arne Gericke Jennifer Marcinkiewicz Accepted by Robert Dorman , Director, School of Biomedical Science John Stalvey , Dean, Collage of Arts and Sciences ii TABLE OF CONTENTS LIST OF FIGURES……………………………………………………………..vi ACKNOWLEDGMENTS……………………………………………………..viii CHAPTER I: INTRODUCTION……………………………………….…........1 a. Bile Acid Synthesis…………………………………………….……….2 i. Importance of Bile Acid Synthesis Pathway………………….….....2 ii. Bile Acid Transport..…………………………………...…...………...3 iii. Bile Acid Synthesis Pathway………………………………………...…4 iv. Classical Bile Acid Synthesis Pathway…..……………………..…..8 Cholesterol 7 -hydroxylase (CYP7A1)……..........………….....8 Transcriptional Regulation of Cholesterol 7 -hydroxylase by Bile Acid-activated FXR…………………………….....…10 CYP7A1 Transcriptional Repression by SHP-dependant Mechanism…………………………………………………...10 CYP7A1 Transcriptional Repression by SHP-independent Mechanism……………………………………..…………….…….11 CYP7A1 Transcriptional Repression by Activated Cellular Kinase…….…………………………...…………………….……12 v. Alternative/ Acidic Bile Acid Synthesis Pathway…………......…….12 Sterol 27-hydroxylase (CYP27A1)……………….…………….12 -

Hanna Joleen 2018 Thesis.Pdf
Validation of an In Vitro Mutagenicity Assay Based on Pulmonary Epithelial Cells from the Transgenic MutaMouse: Intra-Laboratory Variability and Metabolic Competence By: Joleen Hanna, B.Sc. A thesis submitted in partial fulfillment of the requirements for the degree of Master of Science In Biology Specializing in Chemical and Environmental Toxicology Supervisor: Dr. Paul White (University of Ottawa) Thesis Advisory Committee: Dr. Frances Pick (University of Ottawa) Dr. Iain Lambert (Carleton University) University of Ottawa Ontario, Canada March 2018 © Joleen Hanna, Ottawa, Canada, 2018 Abstract: Genetic toxicity tests used for regulatory screening must be rigorously validated to ensure accuracy, reliability and relevance. Hence, prior to establishment of an internationally- accepted test guideline, a new assay must undergo multi-stage validation. An in vitro transgene mutagenicity assay based on an immortalized cell line derived from MutaMouse lung (i.e., FE1 cells) is currently undergoing formal validation. FE1 cells retain a lacZ transgene in a λgt10 shuttle vector that can be retrieved for scoring of chemically-induced mutations. This work contributes to validation of the in vitro transgene (lacZ) mutagenicity assay in MutaMouse FE1 cells. More specifically, the work includes an intra-laboratory variability study, and a follow-up study to assess the endogenous metabolic capacity of FE1 cells. The former is essential to determine assay reliability, the latter to define the range of chemicals that can be reliably screened without an exogenous metabolic activation mixture (i.e., rat liver S9). The intra- laboratory variability assessment revealed minimal variability; thus, assay reproducibility can be deemed acceptable. Assessment of metabolic capacity involved exposure of FE1 cells to 5 known mutagens, and subsequent assessment of changes in the expression of genes involved in xenobiotic metabolism; induced transgene mutant frequency (±S9) was assessed in parallel. -
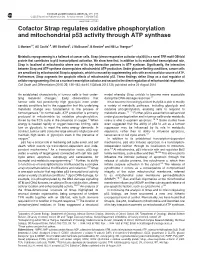
Cofactor Strap Regulates Oxidative Phosphorylation and Mitochondrial P53 Activity Through ATP Synthase
Cell Death and Differentiation (2015) 22, 156–163 & 2015 Macmillan Publishers Limited All rights reserved 1350-9047/15 www.nature.com/cdd Cofactor Strap regulates oxidative phosphorylation and mitochondrial p53 activity through ATP synthase S Maniam1,4, AS Coutts1,4, MR Stratford2, J McGouran3, B Kessler3 and NB La Thangue*,1 Metabolic reprogramming is a hallmark of cancer cells. Strap (stress-responsive activator of p300) is a novel TPR motif OB-fold protein that contributes to p53 transcriptional activation. We show here that, in addition to its established transcriptional role, Strap is localised at mitochondria where one of its key interaction partners is ATP synthase. Significantly, the interaction between Strap and ATP synthase downregulates mitochondrial ATP production. Under glucose-limiting conditions, cancer cells are sensitised by mitochondrial Strap to apoptosis, which is rescued by supplementing cells with an extracellular source of ATP. Furthermore, Strap augments the apoptotic effects of mitochondrial p53. These findings define Strap as a dual regulator of cellular reprogramming: first as a nuclear transcription cofactor and second in the direct regulation of mitochondrial respiration. Cell Death and Differentiation (2015) 22, 156–163; doi:10.1038/cdd.2014.135; published online 29 August 2014 An established characteristic of tumour cells is their under- model whereby Strap unfolds to become more accessible lying metabolic changes.1 Early observations that during the DNA-damage response.12 tumour cells had persistently high