TRAMADOL Pre-Review Report Agenda Item 5.3
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Tramadol (Ultram)
TRAMADOL (ULTRAM) Tramadol is FDA approved for the treatment of musculoskeletal pain. Studies have shown it is useful in treating the pain associated with diabetic neuropathy and other pain conditions. Tramadol comes in 50 mg tablets. The maximum dose is two tablets four times per day unless your kidney function is below normal or you are over 75 years old, in which case the maximum dose is two tablets three times per day. The main side effects of Tramadol are drowsiness, sedation, and stomach upset, all of which are minimized by slowly raising the dose. About 5% of patients have stomach upset at any dose of Tramadol and cannot take the medicine. Other risks include seizures (occur in less than 1/100,000 and are more likely if you have seizures) and possibly abuse (relevant if you have abused drugs in the past). Tramadol should be started at a low dose and raise the dose slowly toward the maximum dose. Start with one tablet at bedtime. After 3 - 7 days, increase to one tablet twice daily (morning and bedtime). After an additional 3 - 7 days, increase to one tablet three times per day (morning, noon, and bedtime). After an additional 3 - 7 days, increase to one tablet four times per day (1 tablet with each meal and 1 at bedtime). At that point, the dose may be increased or adjusted depending on how you are doing. To increase further, you will: Add a second tablet at bedtime (one tablet three times per day and two tablets at bedtime). After 3 - 7 days, add a second tablet to another dose (one tablet twice per day and two tablets twice per day). -

Effects of Prophylactic Ketamine and Pethidine to Control Postanesthetic Shivering: a Comparative Study
Biomedical Research and Therapy, 5(12):2898-2903 Original Research Effects of prophylactic ketamine and pethidine to control postanesthetic shivering: A comparative study Masoum Khoshfetrat1, Ali Rosom Jalali2, Gholamreza Komeili3, Aliakbar Keykha4;∗ ABSTRACT Background: Shivering is an undesirable complication following general anesthesia and spinal anesthesia, whose early control can reduce postoperative metabolic and respiratory complications. Therefore, this study aims to compare the effects of prophylactic injection of ketamine and pethi- dine on postoperative shivering.Methods: This double-blind clinical trial was performed on 105 patients with short-term orthopedic and ENT surgery. The patients were randomly divided into three groups; 20 minutes before the end of the surgery, 0.4 mg/kg of pethidine was injected to the first group, 0.5 mg/kg of ketamine was injected to the second group, and normal saline was injected to the third group. After the surgery, the tympanic membrane temperature was measured at 0, 10, 20, and 30 minutes. The shivering was also measured by a four-point grading from zero (no shiv- ering) to four (severe shivering). Data were analyzed by one-way ANOVA, Kruskal Wallis, Chi-square 1Doctor of Medicine (MD), Fellow of and Pearson correlation. Results: The mean age of patients was 35.811.45 years in the ketamine Critical Care Medicine (FCCM), group, 34.811.64 years in the normal saline group, and 33.1110.5 years in the pethidine group. Department of Anesthesiology and The one-way ANOVA showed no significant difference in the mean age between the three groups Critical Care, Khatam-Al-Anbiya (P=0.645). -

Current Awareness in Clinical Toxicology Editors: Damian Ballam Msc and Allister Vale MD
Current Awareness in Clinical Toxicology Editors: Damian Ballam MSc and Allister Vale MD February 2016 CONTENTS General Toxicology 9 Metals 38 Management 21 Pesticides 41 Drugs 23 Chemical Warfare 42 Chemical Incidents & 32 Plants 43 Pollution Chemicals 33 Animals 43 CURRENT AWARENESS PAPERS OF THE MONTH How toxic is ibogaine? Litjens RPW, Brunt TM. Clin Toxicol 2016; online early: doi: 10.3109/15563650.2016.1138226: Context Ibogaine is a psychoactive indole alkaloid found in the African rainforest shrub Tabernanthe Iboga. It is unlicensed but used in the treatment of drug and alcohol addiction. However, reports of ibogaine's toxicity are cause for concern. Objectives To review ibogaine's pharmacokinetics and pharmacodynamics, mechanisms of action and reported toxicity. Methods A search of the literature available on PubMed was done, using the keywords "ibogaine" and "noribogaine". The search criteria were "mechanism of action", "pharmacokinetics", "pharmacodynamics", "neurotransmitters", "toxicology", "toxicity", "cardiac", "neurotoxic", "human data", "animal data", "addiction", "anti-addictive", "withdrawal", "death" and "fatalities". The searches identified 382 unique references, of which 156 involved human data. Further research revealed 14 detailed toxicological case reports. Current Awareness in Clinical Toxicology is produced monthly for the American Academy of Clinical Toxicology by the Birmingham Unit of the UK National Poisons Information Service, with contributions from the Cardiff, Edinburgh, and Newcastle Units. The NPIS is commissioned by Public Health England Current Awareness in Clinical Toxicology Editors: Damian Ballam MSc and Allister Vale MD February 2016 Current Awareness in Clinical Toxicology is produced monthly for the American Academy of Clinical Toxicology by the Birmingham Unit of the UK National Poisons Information Service, with contributions from the Cardiff, Edinburgh, and Newcastle Units. -
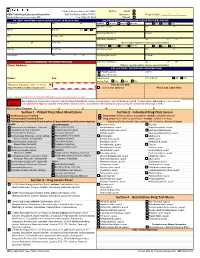
Quantitative Drug Test Menu Section 2
1 Guthrie Square, Sayre, PA 18840 Bill To: Client GMG Toxicology Laboratory Requisition Toll Free Phone (844) 617-4719 Insurance Request Date: _____/______/______ Medical Director: Hani Hojjati, MD Fax (570) 887-4729 Patient PATIENT INFORMATION (PLEASE PRINT IN BLACK INK) INSURANCE BILLING INFORMATION (PLEASE PRINT IN BLACK INK) Pt Last Name First M I PRIMARY Medicare Medicaid Other Ins. Self Spouse Child __ Subscriber Last Name First M Address Birth Date Sex M F Beneficiary/Member # Group # City Pt. SS# or MRN Claims Name and Address City ST ZIP ST ZIP Home Phone (Attach a copy of the patient's insurance card and information) SECONDARY Medicare Medicaid Other Ins. Self Spouse Child Employer Work Phone Subscriber Last Name First M Work Address City ST ZIP Beneficiary/Member # Group # __ CLIENT INFORMATION - REFERRING PHYSICIAN Claims Name and Address City ST ZIP Client Address: (Atttach a copy of the patient's insurance card and information) COLLECTION / REPORTING INFORMATION Copy to: FAX Results to __ CALL Results to Phone: Fax: Date Collected: Time Collected: AM PM Specimen Type: Urine Saliva Other ___________________ Physician Signature (legible - No Stamp) For Lab Use Only (Required for Medicare & Medicaid patient orders) Signed ABN Obtained Place Lab Label Here Contact Laboratory Medical Director (570-887-4719) with questions concerning medical necessity PHYSICIAN When ordering tests, the physician is required to make an independent medical necessity decision with regard to each test thelaboratory will bill. The physician also understands he or she is required NOTICE to (1) submit ICD-10 diagnosis supported in the patient's medical record as documentation of the medical necessity or (2) explain and have the patient sign an ABN. -

Nitrous Oxide in Emergency Medicine Í O’ Sullivan, J Benger
214 ANALGESIA Emerg Med J: first published as 10.1136/emj.20.3.214 on 1 May 2003. Downloaded from Nitrous oxide in emergency medicine Í O’ Sullivan, J Benger ............................................................................................................................. Emerg Med J 2003;20:214–217 Safe and predictable analgesia is required for the identify these zones as there is considerable vari- potentially painful or uncomfortable procedures often ation between people. He also emphasised the importance of the patient’s pre-existing beliefs. If undertaken in an emergency department. The volunteers expect to fall asleep while inhaling characteristics of an ideal analgesic agent are safety, 30% N2O then a high proportion do so. An appro- predictability, non-invasive delivery, freedom from side priate physical and psychological environment increases the actions of N2O and may allow lower effects, simplicity of use, and a rapid onset and offset. doses to be more effective. Unlike many other Newer approaches have threatened the widespread use anaesthetic agents, N2O exhibits an acute toler- of nitrous oxide, but despite its long history this simple ance effect, whereby its potency is greater at induction than after a period of “accommoda- gas still has much to offer. tion”. .......................................................................... MECHANISM OF ACTION “I am sure the air in heaven must be this Some writers have suggested that N2O, like wonder-working gas of delight”. volatile anaesthetics, causes non-specific central nervous system depression. Others, such as 4 Robert Southey, Poet (1774 to 1843) Gillman, propose that N2O acts specifically by interacting with the endogenous opioid system. HISTORY N2O is known to act preferentially on areas of the Nitrous oxide (N2O) is the oldest known anaes- brain and spinal cord that are rich in morphine thetic agent. -

Analgesic Indications: Developing Drug and Biological Products
Guidance for Industry Analgesic Indications: Developing Drug and Biological Products DRAFT GUIDANCE This guidance document is being distributed for comment purposes only. Comments and suggestions regarding this draft document should be submitted within 60 days of publication in the Federal Register of the notice announcing the availability of the draft guidance. Submit electronic comments to http://www.regulations.gov. Submit written comments to the Division of Dockets Management (HFA-305), Food and Drug Administration, 5630 Fishers Lane, rm. 1061, Rockville, MD 20852. All comments should be identified with the docket number listed in the notice of availability that publishes in the Federal Register. For questions regarding this draft document contact Sharon Hertz at 301-796-2280. U.S. Department of Health and Human Services Food and Drug Administration Center for Drug Evaluation and Research (CDER) February 2014 Clinical/Medical 5150dft.doc 01/15/14 Guidance for Industry Analgesic Indications: Developing Drug and Biological Products Additional copies available from: Office of Communications, Division of Drug Information Center for Drug Evaluation and Research Food and Drug Administration 10903 New Hampshire Ave., Bldg. 51, rm. 2201 Silver Spring, MD 20993-0002 Tel: 301-796-3400; Fax: 301-847-8714; E-mail: [email protected] http://www.fda.gov/Drugs/GuidanceComplianceRegulatoryInformation/Guidances/default.htm U.S. Department of Health and Human Services Food and Drug Administration Center for Drug Evaluation and Research (CDER) February -

Diclofenac Topical Patch Gel Solution Monograph
Diclofenac Topical Patch, Gel and Solution National Drug Monograph March 2016 VHA Pharmacy Benefits Management Services, Medical Advisory Panel, and VISN Pharmacist Executives The purpose of VA PBM Services drug monographs is to provide a focused drug review for making formulary decisions. Updates will be made when new clinical data warrant additional formulary discussion. Documents will be placed in the Archive section when the information is deemed to be no longer current. FDA Approval Information Description/Mechanism of Action Diclofenac is the only nonsteroidal antiinflammatory drug (NSAID) approved in the U.S. for topical application. The mechanism of diclofenac is believed to be inhibition of prostaglandin synthesis, primarily by nonselectively inhibiting cyclooxygenase. The agents covered in this review are the four diclofenac topical products approved for analgesic purposes: Diclofenac epolamine / hydroxyethylpyrrolidine patch (DEHP) 1.3% approved in January 2007 Diclofenac sodium topical gel 1%, approved in October 2007 Diclofenac sodium topical solution 1.5% with dimethyl sulfoxide (DMSO, 45.5% w/w), approved in November 2009 Diclofenac sodium topical solution 2% with dimethyl sulfoxide (DMSO, 45.5% w/w), approved in January 2014 Indication(s) Under Review in this document (may include off Solution 1.5% Solution 2% label) Patch 1.3% Gel 1% (Drops) (MDP) Topical treatment Relief of the pain of Treatment of signs Treatment of the Also see Table 1 Product Descriptions of acute pain due osteoarthritis of joints and symptoms of pain of below. to minor strains, amenable to topical osteoarthritis of the osteoarthritis of sprains, and treatment, such as the knee(s) the knee(s) contusions knees and those of the hands. -

CAN YOU TAKE TRAMADOL with NEFOPAM Can You Take Tramadol with Nefopam
CAN YOU TAKE TRAMADOL WITH NEFOPAM can you take tramadol with nefopam tramadol 37 5 vs percocet 5 325 ultram tramadol pictures tramadol hcl tabs 50 mg tramadol 200 mg recreational drugs and heart can tramadol and percocet be mixed hbs robaxin tramadol interaction generic tramadol 319 immediate release how long tramadol stay in your urine does tramadol make you sleepy or awake tramadol acetaminophen\/codeine 120 12mg sol b tracert ex tramadol dosage for adults meloxicam/tramadol/amitriptyline/lidocaine/prilocaine apo tramadol high feeling on hydrocodone tramadol apteka internetowa olmed order tramadol/paracetamol from mexico tramadol quizlet flashcards microbiology tramadol has mu opioid agonist activity director jobs tramadol met ritalin sr strengths hur ta tramadol withdrawal in dogs tramadol te gebruiken bij tramadol dosis cachorros bulldog 2015 100mg tramadol 10mg hydrocodone images 100 tramadol termasuk jenis obat apa acyclovir side how to get rid of a tramadol high 200 ml tramadol withdrawal timeline drug interactions between percocet and tramadol comparison tramadol e morfina presentacion de tres can tramadol be taken with paracetamol indication and action tramadol review article template with photos tramadol codeine allergy rash best price tramadol online tramadol 93 58 dosage for ibuprofen tramadol v oxycodone pill colors can tramadol make you drowsy doll b tracert ex tramadol addiction withdrawal tramadol instant release oxycontin pictures can you drink wine with tramadol i can function tramadol hydrochloride sleepy tramadol cva -

Diclofenac Sodium Enteric-Coated Tablets) Tablets of 75 Mg Rx Only Prescribing Information
® Voltaren (diclofenac sodium enteric-coated tablets) Tablets of 75 mg Rx only Prescribing Information Cardiovascular Risk • NSAIDs may cause an increased risk of serious cardiovascular thrombotic events, myocardial infarction, and stroke, which can be fatal. This risk may increase with duration of use. Patients with cardiovascular disease or risk factors for cardiovascular disease may be at greater risk. (See WARNINGS.) • Voltaren® (diclofenac sodium enteric-coated tablets) is contraindicated for the treatment of perioperative pain in the setting of coronary artery bypass graft (CABG) surgery (see WARNINGS). Gastrointestinal Risk • NSAIDs cause an increased risk of serious gastrointestinal adverse events including inflammation, bleeding, ulceration, and perforation of the stomach or intestines, which can be fatal. These events can occur at any time during use and without warning symptoms. Elderly patients are at greater risk for serious gastrointestinal events. (See WARNINGS.) DESCRIPTION Voltaren® (diclofenac sodium enteric-coated tablets) is a benzene-acetic acid derivative. Voltaren is available as delayed-release (enteric-coated) tablets of 75 mg (light pink) for oral administration. The chemical name is 2-[(2,6-dichlorophenyl)amino] benzeneacetic acid, monosodium salt. The molecular weight is 318.14. Its molecular formula is C14H10Cl2NNaO2, and it has the following structural formula The inactive ingredients in Voltaren include: hydroxypropyl methylcellulose, iron oxide, lactose, magnesium stearate, methacrylic acid copolymer, microcrystalline cellulose, polyethylene glycol, povidone, propylene glycol, sodium hydroxide, sodium starch glycolate, talc, titanium dioxide. CLINICAL PHARMACOLOGY Pharmacodynamics Voltaren® (diclofenac sodium enteric-coated tablets) is a nonsteroidal anti-inflammatory drug (NSAID) that exhibits anti-inflammatory, analgesic, and antipyretic activities in animal models. The mechanism of action of Voltaren, like that of other NSAIDs, is not completely understood but may be related to prostaglandin synthetase inhibition. -

Use of Non-Opioid Analgesics As Adjuvants to Opioid Analgesia for Cancer Pain Management in an Inpatient Palliative Unit: Does T
Support Care Cancer (2015) 23:695–703 DOI 10.1007/s00520-014-2415-9 ORIGINAL ARTICLE Use of non-opioid analgesics as adjuvants to opioid analgesia for cancer pain management in an inpatient palliative unit: does this improve pain control and reduce opioid requirements? Shivani Shinde & Pamela Gordon & Prashant Sharma & James Gross & Mellar P. Davis Received: 2 October 2013 /Accepted: 18 August 2014 /Published online: 29 August 2014 # Springer-Verlag Berlin Heidelberg 2014 Abstract morphine equivalent doses of the opioid in both groups (median Background Cancer pain is complex, and despite the intro- (min, max); 112 (58, 504) vs. 200 (30, 5,040)) at the time of duction of the WHO cancer pain ladder, few studies have discharge; 75–80 % of patients had improvement in pain scores looked at the prevalence of adjuvant medication use in an as measured by a two-point reduction in numerical rating scale inpatient palliative medicine unit. In this study, we evaluate (NRS). the use of adjuvant pain medications in patients admitted to an Discussion This study shows that adjuvant medications are inpatient palliative care unit and whether their use affects pain commonly used for treating pain in patients with cancer. More scores or opiate dosing. than half of study population were on two adjuvants or an Methods In this retrospective observational study, patients adjuvant plus NSAID along with an opioid. We did not admitted to the inpatient palliative care unit over a 3-month demonstrate any benefit in terms of improved pain scores or period with a diagnosis of cancer on opioid therapy were opioid doses with adjuvants, but this could reflect confound- selected. -

Parkinson's Disease Fact Sheet
Parkinson’s Disease Fact Sheet About Parkinson’s Disease Parkinson’s disease is a progressive, incurable neurological disorder associated with a loss of dopamine-generating cells in the brain. It is primarily associated with progressive loss of motor control, but it results in a complex array of symptoms, including many non-motor symptoms. Parkinson’s impacts an estimated one million people in the United States. Critical Clinical Care Considerations • To avoid serious side effects, Parkinson’s patients need their medications on time, every time — do not skip or postpone doses. • Write down the exact times of day medications are to be administered so that doses are given on the same schedule the patient follows at home. • Do not substitute Parkinson’s medications or stop levodopa therapy abruptly. • Resume medications immediately following procedures, unless vomiting or severely incapacitated. • If an antipsychotic is necessary, use pimavanserin (Nuplazid), quetiapine (Seroquel) or clozapine (Clozaril). • Be alert for symptoms of dysphagia (trouble swallowing) and risk of pneumonia. • Ambulate as soon as medically safe. Patients may require assistance. Common Symptoms of Parkinson’s Disease Motor Non-Motor • Shaking or tremor at rest • Depression • Bradykinesia or freezing (being stuck • Anxiety in place when attempting to walk) • Constipation • Low voice volume or muffled speech • Cognitive decline and dementia • Lack of facial expression • Impulse control disorders • Stiffness or rigidity of the arms, legs • Orthostatic hypotension or -

ATC CODING for MEDICATION DATA SAS DATASET NAME: Meds1 8S PROTOCOL NAME: Meds1 8S Protocol.Don
ATC CODING FOR MEDICATION DATA SAS DATASET NAME: meds1_8s PROTOCOL NAME: meds1_8s_protocol.don Medications were coded using the World Health Organization‟s Anatomical Therapeutic Chemical (ATC) classifications. Information about the ATC classification system can be found at http://www.whocc.no/atcddd/. Briefly, The numeric ATC codes assigned to a drug can be broken down into five parts. For example in the code N02BE01: The first character (N) represents the main anatomical group. In this example N = Nervous System. Characters two and three (02) represent the therapeutic subgroup. In this example N02 = Analgesics. Character four (B) represents the pharmacological subgroup. In this example N02B = Other analgesics and antipyretics. Character five (E) represents the chemical subgroup. In this example N02BE = Anilides. Characters six and seven (01) represent the chemical substance. In this example N02BE01 = Paracetamol (acetaminophen). If a medication consists of multiple compounds, all unique compounds were coded leaving up to four codes per medication in the coded database (variable names = atc_cod1,…,atc_cod4). There were a few exceptions including oral contraceptives, vitamins/supplements and other multi-compound medications not assigned to one code per compound due to the nature of the medication. Looking at the contraceptive example below, if we use the first two codes instead of one of the second two codes we lose the info about fixed or sequential doses and the fact that it is specifically an oral contraceptive: (1) G03AC03 LEVONORGESTREL