Polyclinics and Alternatives, a Patient-Centred Analysis of How Organisation Constrains Care Coordination
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-
Health Care Systems in the Eu a Comparative Study
EUROPEAN PARLIAMENT DIRECTORATE GENERAL FOR RESEARCH WORKING PAPER HEALTH CARE SYSTEMS IN THE EU A COMPARATIVE STUDY Public Health and Consumer Protection Series SACO 101 EN This publication is available in the following languages: EN (original) DE FR The opinions expressed in this document are the sole responsibility of the author and do not necessarily represent the official position of the European Parliament. Reproduction and translation for non-commercial purposes are authorized, provided the source is acknowledged and the publisher is given prior notice and sent a copy. Publisher: EUROPEAN PARLIAMENT L-2929 LUXEMBOURG Author: Dr.med. Elke Jakubowski, MSc. HPPF, Advisor in Public Health Policy Department of Epidemiology and Social Medicine, Medical School Hannover Co-author: Dr.med. Reinhard Busse, M.P.H., Department of Epidemiology and Social Medicine, Medical School Hannover Editor: Graham R. Chambers BA Directorate-General for Research Division for Policies on Social Affairs, Women, Health and Culture Tel.: (00 352) 4300-23957 Fax: (00 352) 4300-27720 e-mail: [email protected] WITH SPECIAL GRATITUDE TO: James Kahan, Panos Kanavos, Julio Bastida-Lopez, Elias Mossialos, Miriam Wiley, Franco Sassi, Tore Schersten, Juha Teperi for their helpful comments and reviews of earlier drafts of the country chapters, and Manfred Huber for additional explanatory remarks on OECD Health Data. The manuscript was completed in May 1998. EUROPEAN PARLIAMENT DIRECTORATE GENERAL FOR RESEARCH WORKING PAPER HEALTH CARE SYSTEMS IN THE EU A COMPARATIVE STUDY Public Health and Consumer Protection Series SACO 101 EN 11-1998 Health Care Systems CONTENTS INTRODUCTION ........................................................... 5 PART ONE: A Comparative Outline of the Health Care Systems of the EU Member States ........................................ -
Full-Text Provided on Manchester Research Explorer Is the Author Accepted Manuscript Or Proof Version This May Differ from the Final Published Version
The University of Manchester Research Moving Services out of hospital: Joining up General Practice and community services? Link to publication record in Manchester Research Explorer Citation for published version (APA): Bramwell, D., Checkland, K., Allen, P., & Peckham, S. (2014). Moving Services out of hospital: Joining up General Practice and community services? Policy Research Unit in Commissioning and the Healthcare System Manchester Centre for Health Economics. Citing this paper Please note that where the full-text provided on Manchester Research Explorer is the Author Accepted Manuscript or Proof version this may differ from the final Published version. If citing, it is advised that you check and use the publisher's definitive version. General rights Copyright and moral rights for the publications made accessible in the Research Explorer are retained by the authors and/or other copyright owners and it is a condition of accessing publications that users recognise and abide by the legal requirements associated with these rights. Takedown policy If you believe that this document breaches copyright please refer to the University of Manchester’s Takedown Procedures [http://man.ac.uk/04Y6Bo] or contact [email protected] providing relevant details, so we can investigate your claim. Download date:04. Oct. 2021 Moving Services out of hospital: Joining up General Practice and community services? August 2014 Research Team: Dr Donna Bramwell1 Dr Kath Checkland1 Dr Pauline Allen2 Professor Stephen Peckham3 Disclaimer: This research is funded by the Department of Health via the Policy Research Programme. The views expressed are those of the researchers and not necessarily those of the Department of Health. -

Health Care Facilities Hospitals Report on Training Visit
SLOVAK UNIVERSITY OF TECHNOLOGY IN BRATISLAVA FACULTY OF ARCHITECTURE INSTITUTE OF HOUSING AND CIVIC STRUCTURES HEALTH CARE FACILITIES HOSPITALS REPORT ON TRAINING VISIT In the frame work of the project No. SAMRS 2010/12/10 “Development of human resource capacity of Kabul polytechnic university” Funded by UÜtà|áÄtät ECDC cÜÉA Wtâw f{t{ YtÜâÖ December, 14, 2010 Prof. Daud Shah Faruq Health Care Facilities, Hospitals 2010/12/14 Acknowledgement: I Daud Shah Faruq professor of Kabul Poly Technic University The author of this article would like to express my appreciation for the Scientific Training Program to the Faculty of Architecture of the Slovak University of Technology and Slovak Aid program for financial support of this project. I would like to say my hearth thanks to Professor Arch. Mrs. Veronika Katradyova PhD, and professor Arch. Mr. stanislav majcher for their guidance and assistance during the all time of my training visit. My thank belongs also to Ing. Juma Haydary, PhD. the coordinator of the project SMARS/2010/10/01 in the frame work of which my visit was realized. Besides of this I would like to appreciate all professors and personnel of the faculty of Architecture for their good behaves and hospitality. Best regards cÜÉyA Wtâw ft{t{ YtÜâÖ December, 14, 2010 2 Prof. Daud Shah Faruq Health Care Facilities, Hospitals 2010/12/14 VISITING REPORT FROM FACULTY OF ARCHITECTURE OF SLOVAK UNIVERSITY OF TECHNOLOGY IN BRATISLAVA This visit was organized for exchanging knowledge views and advices between us (professor of Kabul Poly Technic University and professors of this faculty). My visit was especially organized to the departments of Public Buildings and Interior design. -

Annual Report 2010
nd 22 Annual Conference Annual Report 2010 The major challenge since the 21st Annual Conference in December 2009 has been the national DHB MECA negotiations. Other challenges include promoting clinical leadership and engagement in DHBs consistent with the Time for Quality agreement and the In Good Hands policy statement, and the Government’s proposed amendments to the Employment Relations Act. The members of the National Executive are: President Jeff Brown (MidCentral) Vice President David Jones (Capital & Coast) Region 1 Judy Bent (Auckland) Himadri Seth (Waitemata) Region 2 John Bonning (Waikato) Paul Wilson (Bay of Plenty) Region 3 Hein Stander (Tairawhiti) - since June following the resignation of Torben Iversen in May Tim Frendin (Hawke’s Bay) Region 4 Brian Craig (Canterbury) John MacDonald (Canterbury) In May Torben Iversen resigned to take up a specialist position in Victoria (although still working one week every four in Tairawhiti). While technically eligible to continue on the National Executive practical considerations meant that he chose to resign. The Association is appreciative of the important contribution Dr Iversen made while on the Executive including bringing to the fore the position of members in smaller provincial DHBs, and for his role as Association representative in Tairawhiti. In June Hein Stander was elected unopposed in a by-election. The National Executive has met on four occasions in Wellington since the last Annual Conference, with a fifth meeting to be held immediately preceding this Conference. On 17-18 February the National Executive held its annual two day meeting to discuss strategic directions, the first day being informal. The informal day included: • Preparing for the national DHB MECA negotiations, including strategic direction and the draft claim. -

Towards the Design of a Process Management Approach for the Delivery of Unscheduled Urgent and Emergency Healthcare
UNIVERSITY OF SOUTHAMPTON FACULTY OF BUSINESS, LAW AND ARTS Southampton Business School Towards the Design of a Process Management Approach for the Delivery of Unscheduled Urgent and Emergency Healthcare by Ganye Kwah Driscole Thesis for the degree of Doctor of Philosophy December 2017 UNIVERSITY OF SOUTHAMPTON ABSTRACT FACULTY OF BUSINESS, LAW AND ARTS Management Science Thesis for the degree of Doctor of Philosophy TOWARDS THE DESIGN OF A PROCESS MANAGEMENT APPROACH FOR THE DELIVERY OF UNSCHEDULED URGENT AND EMERGENCY HEALTHCARE Ganye Kwah Driscole Delivering effective urgent and emergency healthcare continues to challenge developed economies despite recent increased spending. The literature suggests that the current design of accident and emergency departments (A&E) does not reflect the process nature of the delivery of unscheduled urgent and emergency care. The research described in this thesis supports the development of a process model to strengthen unscheduled urgent and emergency healthcare delivery and improve A&E operations. A comprehensive literature review is undertaken to investigate the extent and efficacy of process management in healthcare delivery. It shows that process management methods such as Business Process Re-engineering and Lean tend to be applied to individual departments. End-to-end process orientated approaches are scarcely applied. Assessing access to urgent and emergency healthcare in England, a lack of process design and management is found which results in confusion for patients. Based on principles of process orientation, a new proposal is developed that features local urgent healthcare hubs. To investigate the current process, an analysis of A&E providers by catchment area was carried out for London to understand how features of an area such as number of general practitioners affects demand in A&E. -

United Kingdom National Health Services: a Case Study of Workforce Transformation in an Integrated Care Organisation Using Actor-Network Theory
Middlesex University Research Repository An open access repository of Middlesex University research http://eprints.mdx.ac.uk Altabaibeh, Abdelhakim (2018) United Kingdom National Health Services: a case study of workforce transformation in an integrated care organisation using actor-network theory. PhD thesis, Middlesex University. [Thesis] Final accepted version (with author’s formatting) This version is available at: https://eprints.mdx.ac.uk/25948/ Copyright: Middlesex University Research Repository makes the University’s research available electronically. Copyright and moral rights to this work are retained by the author and/or other copyright owners unless otherwise stated. The work is supplied on the understanding that any use for commercial gain is strictly forbidden. A copy may be downloaded for personal, non-commercial, research or study without prior permission and without charge. Works, including theses and research projects, may not be reproduced in any format or medium, or extensive quotations taken from them, or their content changed in any way, without first obtaining permission in writing from the copyright holder(s). They may not be sold or exploited commercially in any format or medium without the prior written permission of the copyright holder(s). Full bibliographic details must be given when referring to, or quoting from full items including the author’s name, the title of the work, publication details where relevant (place, publisher, date), pag- ination, and for theses or dissertations the awarding institution, the degree type awarded, and the date of the award. If you believe that any material held in the repository infringes copyright law, please contact the Repository Team at Middlesex University via the following email address: [email protected] The item will be removed from the repository while any claim is being investigated. -
New Organisational Models of Primary Care to Meet the Future Needs of the NHS a Brief Overview of Recent Reports
EUROPE New organisational models of primary care to meet the future needs of the NHS A brief overview of recent reports Teresa Bienkowska-Gibbs, Sarah King, Catherine L. Saunders, Marie-Louise Henham For more information on this publication, visit www.rand.org/t/RR1181 Published by the RAND Corporation, Santa Monica, Calif., and Cambridge, UK © Copyright 2015 RAND Corporation R® is a registered trademark. Limited Print and Electronic Distribution Rights This document and trademark(s) contained herein are protected by law. This representation of RAND intellectual property is provided for noncommercial use only. Unauthorized posting of this publication online is prohibited. Permission is given to duplicate this document for personal use only, as long as it is unaltered and complete. Permission is required from RAND to reproduce, or reuse in another form, any of its research documents for commercial use. For information on reprint and linking permissions, please visit www.rand.org/pubs/permissions.html. RAND Europe is an independent, not-for-profit policy research organisation that aims to improve policy and decisionmaking in the public interest through research and analysis. RAND’s publications do not necessarily reflect the opinions of its research clients and sponsors. Support RAND Make a tax-deductible charitable contribution at www.rand.org/giving/contribute www.rand.org www.rand.org/randeurope Preface The Health Education England Primary Care Workforce Commission has set out to identify innovative models of primary care that will meet the future needs of the NHS. As part of this work, RAND Europe was commissioned to present a brief overview of models described in a selected group of reports from professional bodies and policy-focused organisations. -

Comparative Case Studies of Health Reform in England
Comparative case studies of health reform in England Report submitted to the Department of Health Policy Research Programme (PRP) Martin Powell, Ross Millar, Abeda Mulla, Hilary Brown, Chris Fewtrell Health Services Management Centre, University of Birmingham Hugh McLeod Health Economics Unit, University of Birmingham Nick Goodwin, Anna Dixon and Chris Naylor The King’s Fund Contents Executive Summary ............................................................................................... 7 Aims and objectives ............................................................................................... 7 Methods and analysis ............................................................................................ 7 Results .................................................................................................................... 8 Conclusions .......................................................................................................... 10 Chapter 1: Introduction ........................................................................................ 13 1.1 Presenting the ‘Next Steps’ policy agenda .................................................... 13 1.2 Looking inside the ‘black box’: evaluating complex policy interventions ..... 16 1.3 Plan of investigation ...................................................................................... 17 1.4 Structure of report ........................................................................................ 18 Chapter 2: Theory and Methods .......................................................................... -

Innovation in European Healthcare – What Can Sweden Learn?
Innovation in European healthcare – what can Sweden learn? An analysis of the systems for innovation in five European countries supported by LIF - the research-based pharmaceutical industry 1 List of content Section Page Introduction 3 The stakeholders on innovation in Swedish healthcare 10 Two innovative companies: Elekta and Index Pharmaceuticals 18 The five European countries 27 Germany 28 What can Sweden learn from Germany? 74 France 75 What can Sweden learn from France? 114 The United Kingdom 115 What can Sweden learn from the United Kingdom? 205 Denmark 206 What can Sweden learn from Denmark? 249 The Netherlands 250 What in Sweden learn from the Netherlands 276 Summary and conclusions 277 Recommendations 282 2 Introduction If it was up to the NIH to cure polio through a centrally directed program. You'd have the best iron lung in the world but not a polio vaccine Samuel Broder - former director of the National Cancer Institute 3 Purpose and scope - what Sweden can learn from the efforts to improve innovation that have been made in other countries? The systems for innovation in five European Innovation countries are analysed: Denmark, Germany, France, the Netherlands, the UK Policy-making – reforms services Healthcare The analysis focuses on three areas: Pharmaceuticals Import Medtech Export • Policy-making and reforms: what is Infrastructure for the political system doing to support Technology innovation Endogenous innovation? (specifically in healthcare, uptake innovation not general measures like tax Reimbursement and exemptions, labour laws etc) incentives • Infrastructure for innovation: are there technology transfer offices, academic health science centres, clusters etc? Focus on infrastructure specific for healthcare, rather than general policies and measures of innovation. -

Interdependence and Autonomy in the NHS - a Market Conundrum
NHSCA Editorial March 2011 Interdependence and Autonomy in the NHS - A Market Conundrum This issue of the NHSCA Newsletter has been Classical public health, having largely themed on the general concept of how a variety conquered the contagions, was finding common of specialist/consultant medical practitioners ground with the relatively new discipline of see their specialism taking its place in a well clinical epidemiology which was increasingly integrated health care system. The general concerning itself with the non-communicable principle of integration of health and social diseases. This set the scene for important new care services extends into the very many life concepts relating the health of individuals to and work customs and activities which bear the health of the societies in which they lived. on human health and disease. Each of the In his momentous paper “Sick Individuals and contributions to the Newsletter is necessarily Sick Populations” Geoffrey Rose demonstrated brief and constitutes the personal reflections of clearly that the largest numbers of disease the contributor. They cover only a small part of victims – numerically the major social burden of the great number of specialised activities which the disease – arose from people with only minor now go to make up a comprehensive medical elevations of risk factors, at low individual risk service. They have been written by individuals but of whom there were great numbers. Medicine who are very aware of the opportunities and traditionally concerned itself with patients with limitations of the current structure of the health major risk factors for the disease, at very high individual risk but contributing little to the total care and social services and with some regard population toll. -
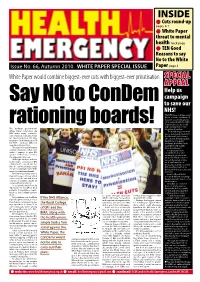
INSIDE L Cuts Round-Up Pages 6-7 L White Paper Threat to Mental Health Back Page L TEN Good Reasons to Say No to the White Issue No
INSIDE l cuts round-up pages 6-7 l White paper threat to mental health back page l TeN Good Reasons to say No to the White Issue No. 66, Autumn 2010. WHITE PAPER SPECIAL ISSUE paper page 3 White Paper would combine biggest-ever cuts with biggest-ever privatisation Special appeal Help us campaign Say NO to ConDem to save our NHS! The NHS faces its biggest-ever threat: a ‘double whammy’ of massive cuts year by year to 2014, coupled with the White Paper proposals that could wipe out all public sector rationingThe ConDem government’s boards! provision of services. White Paper ‘Liberating the The ConDem government NHS’ makes many controver- has no mandate to transform sial proposals, but at its heart the National Health Service are two key factors: the frag- into a national health market. mentation and privatisation of But if there is no public the NHS – and £20 billion of challenge, the White Paper spending cuts by 2014. could be forced quickly The scale of these “efficiency through Parliament. savings” guarantees that even Hospital staff have while it appears to give GPs everything to lose and greater control over services, nothing to gain from the the opposite is the case. proposals which could see With tight budgets and cuts tens of thousands of jobs to be made, consortia of GPs axed, and hundreds of established to spend £80 bil- thousands pushed out of the lion in commissioning budg- NHS workforce, with new ets will inevitably become little threats to their pay scales and more than rationing boards. -
Reform Ideas No 6 Flat-Lining: Lack of Progress on NHS Reform
Reform Ideas No 6 Flat-lining: Lack of progress on NHS reform Thomas Cawston, Cathy Corrie, Clare Fraser and Tara Macpherson June 2013 Executive summary One of the consequences of reduced public spending in this Parliament has been innovation and change in the public services affected. Danny Alexander, Chief Secretary to the Treasury, has put this very well: “This should be seen as an opportunity as well as a challenge. Of course these are really difficult decisions. You’ve got to remember that every pound that you are talking about is potentially somebody’s job or a service that someone relies on. But you can use the process to drive some really good changes in the way the public sector works” (24 April 2013). Unlike most public services, Ministers have both ring-fenced the health budget and sought a radical agenda of reform and value for money. Ministers have said that they want an NHS with a smaller and more flexible workforce, with greater innovation in how care is delivered, with more competition, with better co-operation between the NHS and social care, with more financial discipline and with reduced bureaucracy. This report collects available evidence on the progress of NHS reform in this Parliament. Ministers should be extremely concerned about the lack of progress. In several areas reform is actually in retreat. NHS reform: Progress report Reform objective Key change since 2010 A shift in care from hospitals to other settings General and acute hospitals received higher share of NHS budget Reduction in hospital beds Beds reduced