Contact Lens Fitting: a Guide and Methodology of Contact Lens Fitting
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Case Report Descemet Stripping Endothelial Keratoplasty in a Patient with Keratoglobus and Chronic Hydrops Secondary to a Spontaneous Descemet Membrane Tear
Hindawi Publishing Corporation Case Reports in Ophthalmological Medicine Volume 2013, Article ID 697403, 5 pages http://dx.doi.org/10.1155/2013/697403 Case Report Descemet Stripping Endothelial Keratoplasty in a Patient with Keratoglobus and Chronic Hydrops Secondary to a Spontaneous Descemet Membrane Tear Anton M. Kolomeyer1 and David S. Chu1,2 1 The Institute of Ophthalmology and Visual Science, New Jersey Medical School, University of Medicine and Dentistry of New Jersey, Newark,NJ07103,USA 2 Metropolitan Eye Research and Surgery Institute, 540 Bergen Boulevard, Suite D, Palisades Park, NJ 07650, USA Correspondence should be addressed to David S. Chu; [email protected] Received 4 March 2013; Accepted 7 April 2013 Academic Editors: S. M. Johnson and S. Machida Copyright © 2013 A. M. Kolomeyer and D. S. Chu. This is an open access article distributed under the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited. Purpose. To report the use of Descemet stripping endothelial keratoplasty (DSEK) in a patient with keratoglobus and chronic hydrops. Case Report. We describe a case of a 28-year-old man with bilateral keratoglobus and chronic hydrops in the right eye secondary to spontaneous Descemet membrane tear. The patient presented with finger counting (CF) vision, itching, foreign body sensation, and severe photophobia in the right eye. Peripheral corneal thinning with central corneal protrusion and Descemet mem- brane tear spanning from 4 to 7 o’clock was noted on slit lamp examination. The right eye cornea was 15 mm in the horizontal diam- eter. -

Corneal Ectasia
Corneal Ectasia Secretary for Quality of Care Anne L. Coleman, MD, PhD Academy Staff Nicholas P. Emptage, MAE Nancy Collins, RN, MPH Doris Mizuiri Jessica Ravetto Flora C. Lum, MD Medical Editor: Susan Garratt Design: Socorro Soberano Approved by: Board of Trustees September 21, 2013 Copyright © 2013 American Academy of Ophthalmology® All rights reserved AMERICAN ACADEMY OF OPHTHALMOLOGY and PREFERRED PRACTICE PATTERN are registered trademarks of the American Academy of Ophthalmology. All other trademarks are the property of their respective owners. This document should be cited as follows: American Academy of Ophthalmology Cornea/External Disease Panel. Preferred Practice Pattern® Guidelines. Corneal Ectasia. San Francisco, CA: American Academy of Ophthalmology; 2013. Available at: www.aao.org/ppp. Preferred Practice Pattern® guidelines are developed by the Academy’s H. Dunbar Hoskins Jr., MD Center for Quality Eye Care without any external financial support. Authors and reviewers of the guidelines are volunteers and do not receive any financial compensation for their contributions to the documents. The guidelines are externally reviewed by experts and stakeholders before publication. Corneal Ectasia PPP CORNEA/EXTERNAL DISEASE PREFERRED PRACTICE PATTERN DEVELOPMENT PROCESS AND PARTICIPANTS The Cornea/External Disease Preferred Practice Pattern® Panel members wrote the Corneal Ectasia Preferred Practice Pattern® guidelines (“PPP”). The PPP Panel members discussed and reviewed successive drafts of the document, meeting in person twice and conducting other review by e-mail discussion, to develop a consensus over the final version of the document. Cornea/External Disease Preferred Practice Pattern Panel 2012–2013 Robert S. Feder, MD, Co-chair Stephen D. McLeod, MD, Co-chair Esen K. -

WSPOS Worldwide Webinar 16: Amblyopia - How and When
Answers to Audience Questions - WSPOS Worldwide Webinar 16: Amblyopia - How and When WWW 16 Panellists Anna Horwood Celeste Mansilla David Granet Krista Kelly Lionel Kowal Susan Cotter Yair Morad Anna Horwood (AH), Celeste Mansilla (CM), Krista Kelly (KK), Lionel Kowal (LK), Susan Cotter (SC), Yair Morad (YM) 1. How do you maintain attained iso visual acuity after successful amblyopia treatment? AH: Intermittent monitoring. If they have regressed previously, I might carry on very intermittent occlusion (an hour or two a week) until I was sure it was stable. CM: With gradual and controlled reduction of the treatment, for example: if the patient had 1 hour of patch per day, I leave it with 1 hour 3 times a week during a month. I do a check and if the visual acuity was maintained, I lower patches to 2 times a week. I keep checking and going down like this until I suspend the treatment. If at any time I detect worsening visual acuity, I return to the previous treatment. SC: Best way is attainment of normal binocular vision. I do not worry about ansiometropic amblyopes who have random dot stereopsis post-treatment. If have constant unilateral strabismus, I can do some limited part-time patching, decreasing patching dosage over time given no regression of VA. YM: repeat examination every 6 months. If I see regression, I will prescribe patching for 30 min a day. 2. How do you plan for very dense amblyopes? AH: I very rarely see them because, with screening, they are picked up early and usually do well. -

Infantile Aphakia and Successful Fitting of Pediatric Contact Lenses; a Case Presentation Authors: Virji N, Patel A, Libassi D
Infantile aphakia and successful fitting of pediatric contact lenses; a case presentation Authors: Virji N, Patel A, Libassi D An eleven month old male presents with bilateral aphakia secondary to congenital cataracts. The patient is currently successfully wearing B&L Silsoft Pediatric contact lenses, with good prognosis for vision in both eyes. I. Case History -Patient demographics: African American male, DOB 8/18/2009 -Chief complaint: patient presents with bilateral aphakia secondary to bilateral congenital cataract extraction -Ocular, medical history: S/P CE with anterior vitrectomy OD 09/22/2009, followed by OS 09/29/09. (+) squinting, rubs eyes, light sensitivity -Medications: none -Other salient information: patient has been seen by SUNY Contact Lens clinic since 2 months old, 10/14/2009 II. Pertinent findings -Clinical: Keratometry readings 41.00/41.25 @ 005 OD, 38.50/41.00 @ 046 Axial length, immeasurable Horizontal corneal diameter 8mm OD/OS Fundus exam WNL OU -Others: surgical dates: successful CE OU, September 2009 III. Differential diagnosis -Primary/leading: Idiopathic -Others: Posterior lenticonus, persistent hyperplastic primary vitreous, anterior segment dysgenesis, and posterior pole tumors, trauma, intrauterine infection (rubella), maternal hypoglycemia, trisomy (eg, Down, Edward, and Patau syndromes), myotonic dystrophy, infectious diseases (eg, toxoplasmosis, rubella, cytomegalovirus, and herpes simplex [TORCH]), and prematurity. (5) IV. Diagnosis and discussion -Elaborate on the condition: Bilateral infantile cataracts are one of the major treatable causes of visual impairment in children. (2) Hubel and Weisel’s research on the critical period of visual development determined that if infantile cataracts are removed within the critical period and appropriate correction is worn, vision is greatly improved. -

Strabismus, Amblyopia & Leukocoria
Strabismus, Amblyopia & Leukocoria [ Color index: Important | Notes: F1, F2 | Extra ] EDITING FILE Objectives: ➢ Not given. Done by: Jwaher Alharbi, Farrah Mendoza. Revised by: Rawan Aldhuwayhi Resources: Slides + Notes + 434 team. NOTE: F1& F2 doctors are different, the doctor who gave F2 said she is in the exam committee so focus on her notes Amblyopia ● Definition Decrease in visual acuity of one eye without the presence of an organic cause that explains that decrease in visual acuity. He never complaints of anything and his family never noticed any abnormalities ● Incidence The most common cause of visual loss under 20 years of life (2-4% of the general population) ● How? Cortical ignorance of one eye. This will end up having a lazy eye ● binocular vision It is achieved by the use of the two eyes together so that separate and slightly dissimilar images arising in each eye are appreciated as a single image by the process of fusion. It’s importance 1. Stereopsis 2. Larger field If there is no coordination between the two eyes the person will have double vision and confusion so as a compensatory mechanism for double vision the brain will cause suppression. The visual pathway is a plastic system that continues to develop during childhood until around 6-9 years of age. During this time, the wiring between the retina and visual cortex is still developing. Any visual problem during this critical period, such as a refractive error or strabismus can mess up this developmental wiring, resulting in permanent visual loss that can't be fixed by any corrective means when they are older Why fusion may fail ? 1. -
Intraocular Lenses and Spectacle Correction
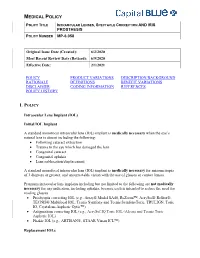
MEDICAL POLICY POLICY TITLE INTRAOCULAR LENSES, SPECTACLE CORRECTION AND IRIS PROSTHESIS POLICY NUMBER MP-6.058 Original Issue Date (Created): 6/2/2020 Most Recent Review Date (Revised): 6/9/2020 Effective Date: 2/1/2021 POLICY PRODUCT VARIATIONS DESCRIPTION/BACKGROUND RATIONALE DEFINITIONS BENEFIT VARIATIONS DISCLAIMER CODING INFORMATION REFERENCES POLICY HISTORY I. POLICY Intraocular Lens Implant (IOL) Initial IOL Implant A standard monofocal intraocular lens (IOL) implant is medically necessary when the eye’s natural lens is absent including the following: Following cataract extraction Trauma to the eye which has damaged the lens Congenital cataract Congenital aphakia Lens subluxation/displacement A standard monofocal intraocular lens (IOL) implant is medically necessary for anisometropia of 3 diopters or greater, and uncorrectable vision with the use of glasses or contact lenses. Premium intraocular lens implants including but not limited to the following are not medically necessary for any indication, including aphakia, because each is intended to reduce the need for reading glasses. Presbyopia correcting IOL (e.g., Array® Model SA40, ReZoom™, AcrySof® ReStor®, TECNIS® Multifocal IOL, Tecnis Symfony and Tecnis SymfonyToric, TRULIGN, Toric IO, Crystalens Aspheric Optic™) Astigmatism correcting IOL (e.g., AcrySof IQ Toric IOL (Alcon) and Tecnis Toric Aspheric IOL) Phakic IOL (e.g., ARTISAN®, STAAR Visian ICL™) Replacement IOLs MEDICAL POLICY POLICY TITLE INTRAOCULAR LENSES, SPECTACLE CORRECTION AND IRIS PROSTHESIS POLICY NUMBER -

Megalocornea Jeffrey Welder and Thomas a Oetting, MS, MD September 18, 2010
Megalocornea Jeffrey Welder and Thomas A Oetting, MS, MD September 18, 2010 Chief Complaint: Visual disturbance when changing positions. History of Present Illness: A 60-year-old man with a history of simple megalocornea presented to the Iowa City Veterans Administration Healthcare System eye clinic reporting visual disturbance while changing head position for several months. He noticed that his vision worsened with his head bent down. He previously had cataract surgery with an iris-sutured IOL due to the large size of his eye, which did not allow for placement of an anterior chamber intraocular lens (ACIOL) or scleral-fixated lens. Past Medical History: Megalocornea Medications: None Family History: No known history of megalocornea Social History: None contributory Ocular Exam: • Visual Acuity (with correction): • OD 20/100 (cause unknown) • OS 20/20 (with upright head position) • IOP: 18mmHg OD, 17mmHg OS • External Exam: normal OU • Pupils: No anisocoria and no relative afferent pupillary defect • Motility: Full OU. • Slit lamp exam: megalocornea (>13 mm in diameter) and with anterior mosaic dystrophy. Iris-sutured posterior chamber IOLs (PCIOLs), stable OD, but pseudophacodonesis OS with loose inferior suture evident. • Dilated funduscopic exam: Normal OU Clinical Course: The patient’s iris-sutured IOL had become loose (tilted and de-centered) in his large anterior chamber, despite several sutures that had been placed in the past, resulting now in visual disturbance with movement. FDA and IRB approval was obtained to place an Artisan iris-clip IOL (Ophtec®). He was taken to the OR where his existing IOL was removed using Duet forceps and scissors. The Artisan IOL was placed using enclavation iris forceps. -

Professional Fitting and Information Guide
CLARITI 1 DAY CONTACT LENS PROFESSIONAL FITTING AND INFORMATION GUIDE Clariti 1 Day (somofilcon A) Clariti 1 Day Toric (somofilcon A) Clariti 1 Day Multifocal (somofilcon A) Clariti 1 Day Multifocal Toric (somofilcon A) Soft (hydrophilic) Contact Lenses for Daily Wear Single Use Only with UV Blocker IMPORTANT: This Professional Fitting and Information Guide contain important information and instructions. Please read carefully and keep this information for future use. CAUTION: Federal law (USA) restricts this device to sale by or on the order of a licensed Eye Care Professional. Part Number: PFG01003 Page 1 of 22 Revision: A Revision Date: August 2016 CLARITI 1 DAY CONTACT LENS Table of Contents INTRODUCTION ........................................................................................................................... 3 PRODUCT DESCRIPTION ............................................................................................................ 3 LENS PARAMETERS AVAILABLE ............................................................................................ 4 TRANSMITTANCE CURVES ....................................................................................................... 5 INDICATIONS (USES) .................................................................................................................. 6 CONTRAINDICATIONS, WARNINGS, PRECAUTIONS AND ADVERSE EFFECTS ............ 7 FITTING GUIDELINES ................................................................................................................ -

Solved/Unsolved
Supplementary Materials: Supplementary table 1. Demographic details for the 54 individual patients (solved/unsolved) and their clinical features including cataract type, details of ocular co-morbidities, systemic features and whether cataract was the presenting feature (non-isolated cataract patients only). Abbreviations: yes (Y), no (N), not applicable (N/A). Age at Famil Ag M/ Age at Cataract Cataract Cataract Systemic Consanguinit Patient ID Gene Confirmed genetic diagnosis Ethnicity diagnosi Ocular co-morbidities FH y ID e F surgery type RE type LE presenting sign features y s (days) Aniridia, nystagmus, 23 years Posterior Posterior 1-1 1 PAX6 Aniridia White British 25 F - glaucoma, foveal N N N Y 4 months subcapsular subcapsular hypoplasia Cleft palate, epilepsy, high Aphakia Aphakia Macular atrophy, myopia, 7 years 9 7 years 8 arched palate, 2-1 2 COL11A1 Stickler syndrome, type II Not Stated 34 F (post- (post- lens subluxation, vitreous N N N months months flattened surgical) surgical) anomaly maxilla, short stature (5'2ft) Anterior segment dysgenesis, pupillary abnormalities including 12 years Posterior Posterior ectopic pupils, ectropion 3-1 3 CPAMD8 Anterior segment dysgenesis 8 Other, Any other 27 F - N N Y N 5 months subcapsular subcapsular UVAE and irodensis, nystagmus, dysplastic optic discs, large corneal diameters Gyrate atrophy of choroid and 23 years 29 years 1 Posterior Posterior Retinal dystrophy, Bipolar 4-1 4 OAT White British 42 F N N N retina 7 months month subcapsular subcapsular exotropia disorder 1 year 6 1 year -

Feasibility and Outcome of Descemet Membrane Endothelial Keratoplasty in Complex Anterior Segment and Vitreous Disease
CLINICAL SCIENCE Feasibility and Outcome of Descemet Membrane Endothelial Keratoplasty in Complex Anterior Segment and Vitreous Disease Julia M. Weller, MD, Theofilos Tourtas, MD, and Friedrich E. Kruse, MD escemet membrane endothelial keratoplasty (DMEK), Purpose: Descemet membrane endothelial keratoplasty (DMEK) is Da technique for posterior lamellar keratoplasty, involves becoming the method of choice for treating Fuchs endothelial a graft consisting only of the thin Descemet membrane with dystrophy and pseudophakic bullous keratopathy. We investigated adherent corneal endothelial cells. Introduced in 2006 by whether DMEK can serve as a routine procedure in endothelial Melles et al,1 DMEK is becoming more popular as several decompensation even in complex preoperative situations. studies show its superiority to Descemet stripping automated Methods: Of a total of 1184 DMEK surgeries, 24 consecutive eyes endothelial keratoplasty (DSAEK), regarding visual function 2,3 with endothelial decompensation and complex preoperative situa- and the time of visual rehabilitation after DMEK. However, tions were retrospectively analyzed and divided into 5 groups: group because DMEK grafts are thinner than DSAEK grafts, it is fi 1: irido-corneo-endothelial syndrome (n = 3), group 2: aphakia, more dif cult to handle them and typically takes surgeons subluxated posterior chamber intraocular lens or anterior chamber longer to learn. intraocular lens (n = 6), group 3: DMEK after trabeculectomy (n = In difficult situations, most surgeons prefer DSAEK or 4), group 4: DMEK with simultaneous intravitreal injection (n = 6), penetrating keratoplasty to DMEK because of its possible and group 5: DMEK after vitrectomy (n = 5). Main outcome intraoperative complications. For example, if corneal edema 4 parameters were best-corrected visual acuity, central corneal thick- is advanced, Ham et al recommend performing DSAEK first ness, endothelial cell density, rebubbling rate, and graft failure rate. -

Glaucoma-Related Adverse Events in the Infant Aphakia Treatment Study 1-Year Results
CLINICAL SCIENCES ONLINE FIRST Glaucoma-Related Adverse Events in the Infant Aphakia Treatment Study 1-Year Results Allen D. Beck, MD; Sharon F. Freedman, MD; Michael J. Lynn, MS; Erick Bothun, MD; Daniel E. Neely, MD; Scott R. Lambert, MD; for the Infant Aphakia Treatment Study Group Objectives: To report the incidence of glaucoma and glau- sistent fetal vasculature and 1.6 times higher for each coma suspects in the IATS, and to evaluate risk factors for month of age younger at cataract surgery. the development of a glaucoma-related adverse event in patients in the IATS in the first year of follow-up. Conclusions: Modern surgical techniques do not elimi- nate the early development of glaucoma following con- Methods: A total of 114 infants between 1 and 6 months genital cataract surgery with or without an intraocular of age with a unilateral congenital cataract were as- lens implant. Younger patients with or without persis- signed to undergo cataract surgery either with or with- tent fetal vasculature seem more likely to develop a glau- out an intraocular lens implant. Standardized defini- coma-related adverse event in the first year of follow- tions of glaucoma and glaucoma suspect were created and up. Vigilance for the early development of glaucoma is used in the IATS. needed following congenital cataract surgery, especially when surgery is performed during early infancy or for a Results: Of these 114 patients, 10 (9%) developed glau- child with persistent fetal vasculature. Five-year fol- coma and 4 (4%) had glaucoma suspect, for a total of 14 low-up data for the IATS will likely reveal more glaucoma- patients (12%) with a glaucoma-related adverse event in related adverse events. -

Analysis of the Variety of Eye Impairments in Glaucoma Cases in Children and Adults
https://doi.org/10.5272/jimab.2017234.1804 Journal of IMAB Journal of IMAB - Annual Proceeding (Scientific Papers). 2017 Oct-Dec;23(4) ISSN: 1312-773X https://www.journal-imab-bg.org Original article ANALYSIS OF THE VARIETY OF EYE IMPAIRMENTS IN GLAUCOMA CASES IN CHILDREN AND ADULTS Tsvetomir Dimitrov Clinical Department of Ophthalmology, First General Hospital for Active Treatment Sofia AD, Sofia, Bulgaria ABSTRACT: the causes for the occurrence of glaucoma remain Glaucoma is a disease, which results in definitive vi- unclarified. There are multiple theories for the occurrence sion reduction. The aim of this study is an analysis of the of the disease, which may be systematized in the follow- differences in eye impairments in connection with the pro- ing way: gression of glaucoma in different age groups (children and 1. The increased intraocular pressure (IOP) impairs adults). A documentary method of investigation of scien- the nerve cells of the retina and of optic nerve due to me- tific sources, based on clinical practice, is applied. The chanical compression. methodology of the study comprises investigation of causes 2. The increased intraocular pressure (IOP) com- and manifestations of the disease and its typology. The spe- presses the blood vessels, which feed the retina and optic cific variety in the manifestation of glaucoma is established nerve, and the compression causes changes related to the in children and adults. Excavation of the optic nerve oc- disturbed blood supply. curs in the adult persons, because the eyeball is already 3. The presence of low blood pressure and high IOP thickened, and collagen is dense.