Module #5. Optional Training Psychotropic Medications And
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Report of the Advisory Group to Recommend Priorities for the IARC Monographs During 2020–2024
IARC Monographs on the Identification of Carcinogenic Hazards to Humans Report of the Advisory Group to Recommend Priorities for the IARC Monographs during 2020–2024 Report of the Advisory Group to Recommend Priorities for the IARC Monographs during 2020–2024 CONTENTS Introduction ................................................................................................................................... 1 Acetaldehyde (CAS No. 75-07-0) ................................................................................................. 3 Acrolein (CAS No. 107-02-8) ....................................................................................................... 4 Acrylamide (CAS No. 79-06-1) .................................................................................................... 5 Acrylonitrile (CAS No. 107-13-1) ................................................................................................ 6 Aflatoxins (CAS No. 1402-68-2) .................................................................................................. 8 Air pollutants and underlying mechanisms for breast cancer ....................................................... 9 Airborne gram-negative bacterial endotoxins ............................................................................. 10 Alachlor (chloroacetanilide herbicide) (CAS No. 15972-60-8) .................................................. 10 Aluminium (CAS No. 7429-90-5) .............................................................................................. 11 -

HIGHLIGHTS of PRESCRIBING INFORMATION These Highlights Do
HIGHLIGHTS OF PRESCRIBING INFORMATION • Metabolic Changes: Atypical antipsychotic drugs have been associated with These highlights do not include all the information needed to use metabolic changes that may increase cardiovascular/cerebrovascular risk. CLOZARIL safely and effectively. See full prescribing information for These metabolic changes include: CLOZARIL. o Hyperglycemia and Diabetes Mellitus: Monitor for symptoms of CLOZARIL® (clozapine) tablets, for oral use hyperglycemia including polydipsia, polyuria, polyphagia, and Initial U.S. Approval: 1989 weakness. Monitor glucose regularly in patients with diabetes or at risk for diabetes. (5.9) WARNING: SEVERE NEUTROPENIA; ORTHOSTATIC o Dyslipidemia: Undesirable alterations in lipids have occurred in HYPOTENSION, BRADYCARDIA, AND SYNCOPE; SEIZURE; patients treated with atypical antipsychotics. (5.9) MYOCARDITIS AND CARDIOMYOPATHY; INCREASED o Weight Gain: Significant weight gain has occurred. Monitor weight MORTALITY IN ELDERLY PATIENTS WITH DEMENTIA- gain. (5.9) RELATED PSYCHOSIS • Neuroleptic Malignant Syndrome (NMS): Immediately discontinue and See full prescribing information for complete boxed warning. monitor closely. Assess for co-morbid conditions. (5.10) • Fever: Evaluate for infection and for neutropenia, NMS. (5.11) • Pulmonary Embolism (PE): Consider PE if respiratory distress, chest pain, • Severe Neutropenia: CLOZARIL can cause severe neutropenia, which or deep-vein thrombosis occur. (5.12) can lead to serious and fatal infections. Patients initiating and • Anticholinergic Toxicity: Use cautiously in presence of specific conditions continuing treatment with CLOZARIL must have a baseline blood (e.g., narrow angle glaucoma, use of anticholinergic drugs). (5.13) absolute neutrophil count (ANC) measured before treatment initiation • Interference with Cognitive and Motor Performance: Advise caution when and regular ANC monitoring during treatment (2.1, 5.1). -

ADHD Parents Medication Guide Revised July 2013
ADHD Parents Medication Guide Revised July 2013 Attention-Deficit/Hyperactivity Disorder Prepared by: American Academy of Child & Adolescent Psychiatry and American Psychiatric Association Supported by the Elaine Schlosser Lewis Fund Physician: ___________________________________________________ Address: ___________________________________________________ ___________________________________________________ ___________________________________________________ Phone: ___________________________________________________ Email: ___________________________________________________ ADHD Parents Medication Guide – July 2013 2 Introduction Attention-Deficit/Hyperactivity Disorder (ADHD) is a neurodevelopmental disorder characterized by difficulty paying attention, excessive activity, and impulsivity (acting before you think). ADHD is usually identified when children are in grade school but can be diagnosed at any time from preschool to adulthood. Recent studies indicate that almost 10 percent of children between the ages of 4 to 17 are reported by their parents as being diagnosed with ADHD. So in a classroom of 30 children, two to three children may have ADHD.1,2,3,4,5 Short attention spans and high levels of activity are a normal part of childhood. For children with ADHD, these behaviors are excessive, inappropriate for their age, and interfere with daily functioning at home, school, and with peers. Some children with ADHD only have problems with attention; other children only have issues with hyperactivity and impulsivity; most children with ADHD have problems with all three. As they grow into adolescence and young adulthood, children with ADHD may become less hyperactive yet continue to have significant problems with distraction, disorganization, and poor impulse control. ADHD can interfere with a child’s ability to perform in school, do homework, follow rules, and develop and maintain peer relationships. When children become adolescents, ADHD can increase their risk of dropping out of school or having disciplinary problems. -

22 Psychiatric Medications for Monitoring in Primary Care
22 Psychiatric Medications for Monitoring in Primary Care Medication Warnings, Precautions, and Adverse Events Comments Class: SSRI Fluvoxamine Boxed Warnings: Suicidality Used much less than SSRIs in the group of eight Indications: Warnings and Precautions: Similar to other SSRIs medications for prescribing, probably because it has no Adult: OCD Adverse Events: Similar to other SSRIs FDA indication for MDD or any anxiety disorder. Still Child/Adolescent: OCD (10-17 years) somewhat popular as a medication for OCD. Uses: Anxiety, OCD Monitoring: Same as other SSRIs Citalopram Boxed Warning: Suicidality. Escitalopram, one of the SSRIs in the group of Indications: Warnings and Precautions: Similar to other SSRIs medications for prescribing, is an active metabolite of Adult: MDD Adverse Events: Similar to other SSRIs citalopram. Escitalopram reportedly has fewer AEs and Child/Adolescent: None less interaction with hepatic metabolic enzymes than Uses: Anxiety, MDD, OCD citalopram but is otherwise essentially identical. Citalopram offers no advantage other than price, as Monitoring: Same as other SSRIs escitalopram is branded until 2012. Paroxetine Boxed Warnings: Suicidality. Paroxetine used much less than the SSRIs for Indications: Warnings and Precautions: Similar to other SSRIs prescribing, probably because of its nonlinear kinetics. Adult: MDD, OCD, Panic Disorder, Generalized Anxiety Adverse Events: Similar to other SSRIs A study of children and adolescents showed doubling Disorder, Social Anxiety Disorder, Posttraumatic Stress Disorder the dose of paroxetine from 10 mg/day to 20 mg/day Child/Adolescent: None resulted in a 7-fold increase in blood levels (Findling et Uses: Anxiety, MDD, OCD al, 1999). Thus, once metabolic enzymes are saturated, paroxetine levels can increase dramatically with dose Monitoring: Same as other SSRIs increases and decrease dramatically with dose decreases, sometimes leading to adverse events. -

Drugs That Can Cause Delirium (Anticholinergic / Toxic Metabolites)
Drugs that can Cause Delirium (anticholinergic / toxic metabolites) Deliriants (drugs causing delirium) Prescription drugs . Central acting agents – Sedative hypnotics (e.g., benzodiazepines) – Anticonvulsants (e.g., barbiturates) – Antiparkinsonian agents (e.g., benztropine, trihexyphenidyl) . Analgesics – Narcotics (NB. meperidine*) – Non-steroidal anti-inflammatory drugs* . Antihistamines (first generation, e.g., hydroxyzine) . Gastrointestinal agents – Antispasmodics – H2-blockers* . Antinauseants – Scopolamine – Dimenhydrinate . Antibiotics – Fluoroquinolones* . Psychotropic medications – Tricyclic antidepressants – Lithium* . Cardiac medications – Antiarrhythmics – Digitalis* – Antihypertensives (b-blockers, methyldopa) . Miscellaneous – Skeletal muscle relaxants – Steroids Over the counter medications and complementary/alternative medications . Antihistamines (NB. first generation) – diphenhydramine, chlorpheniramine). Antinauseants – dimenhydrinate, scopolamine . Liquid medications containing alcohol . Mandrake . Henbane . Jimson weed . Atropa belladonna extract * Requires adjustment in renal impairment. From: K Alagiakrishnan, C A Wiens. (2004). An approach to drug induced delirium in the elderly. Postgrad Med J, 80, 388–393. Delirium in the Older Person: A Medical Emergency. Island Health www.viha.ca/mhas/resources/delirium/ Drugs that can cause delirium. Reviewed: 8-2014 Some commonly used medications with moderate to high anticholinergic properties and alternative suggestions Type of medication Alternatives with less deliriogenic -

Headshop Highs & Lows
HeadshopHeadshop HighsHighs && LowsLows AA PresentationPresentation byby DrDr DesDes CorriganCorrigan HeadshopsHeadshops A.K.A.A.K.A. ““SmartSmart ShopsShops””,, ““HempHemp ShopsShops””,, ““HemporiaHemporia”” oror ““GrowshopsGrowshops”” RetailRetail oror OnlineOnline OutletsOutlets sellingselling PsychoactivePsychoactive Plants,Plants, ‘‘LegalLegal’’ && ““HerbalHerbal”” HighsHighs asas wellwell asas DrugDrug ParaphernaliaParaphernalia includingincluding CannabisCannabis growinggrowing equipment.equipment. Headshops supply Cannabis Paraphernalia HeadshopsHeadshops && SkunkSkunk--typetype (( HighHigh Strength)Strength) CannabisCannabis 1.1. SaleSale ofof SkunkSkunk--typetype seedsseeds 2.2. AdviceAdvice onon SinsemillaSinsemilla TechniqueTechnique 3.3. SaleSale ofof HydroponicsHydroponics && IntenseIntense LightingLighting .. CannabisCannabis PotencyPotency expressedexpressed asas %% THCTHC ContentContent ¾¾ IrelandIreland ¾¾ HerbHerb 6%6% HashHash 4%4% ¾¾ UKUK ¾¾ HerbHerb** 1212--18%18% HashHash 3.4%3.4% ¾¾ NetherlandsNetherlands ¾¾ HerbHerb** 20%20% HashHash 37%37% * Skunk-type SkunkSkunk--TypeType CannabisCannabis && PsychosisPsychosis ¾¾ComparedCompared toto HashHash smokingsmoking controlscontrols ¾¾ SkunkSkunk useuse -- 77 xx riskrisk ¾¾ DailyDaily SkunkSkunk useuse -- 1212 xx riskrisk ¾¾ DiDi FortiForti etet alal .. Br.Br. J.J. PsychiatryPsychiatry 20092009 CannabinoidsCannabinoids ¾¾ PhytoCannabinoidsPhytoCannabinoids-- onlyonly inin CannabisCannabis plantsplants ¾¾ EndocannabinoidsEndocannabinoids –– naturallynaturally occurringoccurring -

BNSSG Shared Care Guidance Please Complete All Sections
NHS Bristol North Bristol NHS Trust NHS North Somerset University Hospitals Bristol NHS Foundation Trust NHS South Gloucestershire Weston Area Health NHS Trust BNSSG Shared Care Guidance Please complete all sections AMBER 3 month Section 1: Heading Avon & Wiltshire Mental Health Partnership NHS Trust Trust(s) Speciality / Department Mental Health Agreement for Lithium Drug (please prescribe by brand name and specify formulation: Priadel, Camcolit®, Liskonum®, Li-Liquid® ) 1. The management of acute manic or hypomanic episodes. 2. The management of episodes of recurrent depressive disorders where treatment with other antidepressants has Indication been unsuccessful. 3. The prophylaxis against bipolar affective disorders. 4. Control of aggressive behaviour or intentional self harm. Section 2: Treatment Schedule Dosage is adjusted based on serum-lithium concentration. Lithium levels must be taken 12 hours post dose, otherwise clinical value is lost. Lithium has a narrow therapeutic range necessitating blood levels between 0.4-1.2mmol/L. The lower end of this range is used for elderly and infirmed patients and the upper end for younger patients, particularly those being treated for an episode of mania. Clinicians should aim for levels of 0.6-0.8 mmol/L, with higher levels possibly being of benefit for patients with predominantly manic symptoms. Usual dose and frequency of Rarely 1.2mmol/L may be used. administration The starting dose is usually 400mg at night (200mg in the elderly), adjusted to achieve the desired serum-lithium concentration. Bloods should be taken 12 hours post dose. For tablet preparations dose is usually given as a single dose at night; for liquid preparations, the dose may be spilt to twice a day. -

The Effects of Antipsychotic Treatment on Metabolic Function: a Systematic Review and Network Meta-Analysis
The effects of antipsychotic treatment on metabolic function: a systematic review and network meta-analysis Toby Pillinger, Robert McCutcheon, Luke Vano, Katherine Beck, Guy Hindley, Atheeshaan Arumuham, Yuya Mizuno, Sridhar Natesan, Orestis Efthimiou, Andrea Cipriani, Oliver Howes ****PROTOCOL**** Review questions 1. What is the magnitude of metabolic dysregulation (defined as alterations in fasting glucose, total cholesterol, low density lipoprotein (LDL) cholesterol, high density lipoprotein (HDL) cholesterol, and triglyceride levels) and alterations in body weight and body mass index associated with short-term (‘acute’) antipsychotic treatment in individuals with schizophrenia? 2. Does baseline physiology (e.g. body weight) and demographics (e.g. age) of patients predict magnitude of antipsychotic-associated metabolic dysregulation? 3. Are alterations in metabolic parameters over time associated with alterations in degree of psychopathology? 1 Searches We plan to search EMBASE, PsycINFO, and MEDLINE from inception using the following terms: 1 (Acepromazine or Acetophenazine or Amisulpride or Aripiprazole or Asenapine or Benperidol or Blonanserin or Bromperidol or Butaperazine or Carpipramine or Chlorproethazine or Chlorpromazine or Chlorprothixene or Clocapramine or Clopenthixol or Clopentixol or Clothiapine or Clotiapine or Clozapine or Cyamemazine or Cyamepromazine or Dixyrazine or Droperidol or Fluanisone or Flupehenazine or Flupenthixol or Flupentixol or Fluphenazine or Fluspirilen or Fluspirilene or Haloperidol or Iloperidone -
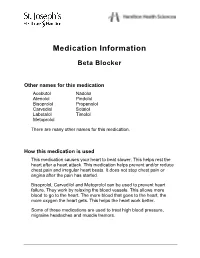
Beta Blocker
Medication Information Beta Blocker Other names for this medication Acebutol Nadolol Atenolol Pindolol Bisoprolol Propanolol Carvediol Sotalol Labetalol Timolol Metoprolol There are many other names for this medication. How this medication is used This medication causes your heart to beat slower. This helps rest the heart after a heart attack. This medication helps prevent and/or reduce chest pain and irregular heart beats. It does not stop chest pain or angina after the pain has started. Bisoprolol, Carvedilol and Metoprolol can be used to prevent heart failure. They work by relaxing the blood vessels. This allows more blood to go to the heart. The more blood that goes to the heart, the more oxygen the heart gets. This helps the heart work better. Some of these medications are used to treat high blood pressure, migraine headaches and muscle tremors. Beta Blocker How to take this medication Take this medication exactly as directed by your doctor or health care provider. It must be taken regularly, even if you feel well. Do not suddenly stop taking this medication without checking with your doctor or health care provider first. Suddenly stopping this medication can cause: • chest pain • irregular heart beats • high blood pressure. When it is time to stop taking this medication your doctor or health care provider may slowly decrease the amount. If you miss a dose of this medication, take it as soon as possible. However, if it is almost time for the next dose, skip the missed dose and go back to your regular time. Do not take 2 doses at one time. -

Psychiatric Medications in Behavioral Healthcarev5
Copyright © The University of South Florida, 2012 Psychiatric Medications in Behavioral Healthcare An Important Notice None of the pages in this tutorial are meant to be a replacement for professional help. The science of medicine is constantly changing, and these changes alter treatment and drug therapies as a result of what is learned through research and clinical experience. The author has relied on resources believed to be reliable at the time material was developed. However, there is always the possibility of human error or changes in medical science and neither the authors nor the University of South Florida can guarantee that all the information in this program is in every respect accurate or complete and they are not responsible for any errors or omissions or for the results obtained from the use of such information. Each person that reads this program is encouraged to confirm the information with other sources and understand that it not be interpreted as medical or professional advice. All medical information needs to be carefully reviewed with a health care provider. Course Objectives At the completion of this program participants should be able to: • Identify at 5 categories of medications used to treat the symptoms of psychiatric disorders, the therapeutic effects of medications in each category, and the side effects associated with medications in each category. • Identify at least 5 medications and the benefits of those medications as compared to the medications. • Identify at least 5 reasons that a person may stop taking medications or not take medications as prescribed. • Demonstrate your learned understanding of psychiatric medications by passing the combined post‐ tests. -

(12) United States Patent (10) Patent No.: US 9,642,912 B2 Kisak Et Al
USOO9642912B2 (12) United States Patent (10) Patent No.: US 9,642,912 B2 Kisak et al. (45) Date of Patent: *May 9, 2017 (54) TOPICAL FORMULATIONS FOR TREATING (58) Field of Classification Search SKIN CONDITIONS CPC ...................................................... A61K 31f S7 (71) Applicant: Crescita Therapeutics Inc., USPC .......................................................... 514/171 Mississauga (CA) See application file for complete search history. (72) Inventors: Edward T. Kisak, San Diego, CA (56) References Cited (US); John M. Newsam, La Jolla, CA (US); Dominic King-Smith, San Diego, U.S. PATENT DOCUMENTS CA (US); Pankaj Karande, Troy, NY (US); Samir Mitragotri, Santa Barbara, 5,602,183 A 2f1997 Martin et al. CA (US); Wade A. Hull, Kaysville, UT 5,648,380 A 7, 1997 Martin 5,874.479 A 2, 1999 Martin (US); Ngoc Truc-ChiVo, Longueuil 6,328,979 B1 12/2001 Yamashita et al. (CA) 7,001,592 B1 2/2006 Traynor et al. 7,795,309 B2 9/2010 Kisak et al. (73) Assignee: Crescita Therapeutics Inc., 8,343,962 B2 1/2013 Kisak et al. Mississauga (CA) 8,513,304 B2 8, 2013 Kisak et al. 8,535,692 B2 9/2013 Pongpeerapat et al. (*) Notice: Subject to any disclaimer, the term of this 9,308,181 B2* 4/2016 Kisak ..................... A61K 47/12 patent is extended or adjusted under 35 2002fOOO6435 A1 1/2002 Samuels et al. 2002fOO64524 A1 5, 2002 Cevc U.S.C. 154(b) by 204 days. 2005, OO 14823 A1 1/2005 Soderlund et al. This patent is Subject to a terminal dis 2005.00754O7 A1 4/2005 Tamarkin et al. -

The Psychoactive Effects of Psychiatric Medication: the Elephant in the Room
Journal of Psychoactive Drugs, 45 (5), 409–415, 2013 Published with license by Taylor & Francis ISSN: 0279-1072 print / 2159-9777 online DOI: 10.1080/02791072.2013.845328 The Psychoactive Effects of Psychiatric Medication: The Elephant in the Room Joanna Moncrieff, M.B.B.S.a; David Cohenb & Sally Porterc Abstract —The psychoactive effects of psychiatric medications have been obscured by the presump- tion that these medications have disease-specific actions. Exploiting the parallels with the psychoactive effects and uses of recreational substances helps to highlight the psychoactive properties of psychi- atric medications and their impact on people with psychiatric problems. We discuss how psychoactive effects produced by different drugs prescribed in psychiatric practice might modify various disturb- ing and distressing symptoms, and we also consider the costs of these psychoactive effects on the mental well-being of the user. We examine the issue of dependence, and the need for support for peo- ple wishing to withdraw from psychiatric medication. We consider how the reality of psychoactive effects undermines the idea that psychiatric drugs work by targeting underlying disease processes, since psychoactive effects can themselves directly modify mental and behavioral symptoms and thus affect the results of placebo-controlled trials. These effects and their impact also raise questions about the validity and importance of modern diagnosis systems. Extensive research is needed to clarify the range of acute and longer-term mental, behavioral, and physical effects induced by psychiatric drugs, both during and after consumption and withdrawal, to enable users and prescribers to exploit their psychoactive effects judiciously in a safe and more informed manner.