Complement and Cancer—A Dysfunctional Relationship?
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Complement Component 3 (C3) Concentrations in Cancer Patients: a Systematic Review and Meta-Analysis
Complement Component 3 (C3) Concentrations in Cancer Patients: A Systematic Review and Meta-Analysis Zipeng Yang South China Agricultural University Zi-Guo Yuan ( [email protected] ) Anqun Yang Dapeng New District Nan'ao Peolple's Hospital of Shenzhen, Guangdong Province, China Xiu-Xiang Zhang South China Agricultural University College of Agriculture Xiaohu Wang Guangdong Academy of Agricultural Sciences, Guangzhou, Guangdong Province Miao Yu Dongfeng Xiyuan District, Stomatological Hospital Aliated to Guangzhou Medical University, Guangzhou Yasser S.Mahmmod Zagazig University Jorge A Hernandez University of Florida Zhaowen Ren South China Agricultural University Xirui Zhang South China Agricultural University Wei Cong Shandong University Research article Keywords: Complement Component 3, Cancer Patients, Meta-Analysis Posted Date: March 26th, 2020 DOI: https://doi.org/10.21203/rs.3.rs-18256/v1 License: This work is licensed under a Creative Commons Attribution 4.0 International License. Read Full License Page 1/17 Abstract Background The aim of this study was to investigate the association between the serum complement component 3 “C3” level and the patients with different types of cancer. Our study nding would ultimately provide reliable scientic conclusions to guide clinical practice. Methods PubMed, Embase, The Chorane Library and Google Scholar were systematically searched to identify all studies on serum C3 concentrations in cancer patients published as of September 2019. Additionally, we conducted a clinical study on serum C3 in lung cancer patients and healthy people. The levels of serum complement C3 in 84 lung cancer patients and 30 healthy people were examined by ELISA. We used standardized mean differences (SMD) to report the pooled estimation, and I² statistics were calculated to examine the heterogeneity. -

Edinburgh Research Explorer
Edinburgh Research Explorer International Union of Basic and Clinical Pharmacology. LXXXVIII. G protein-coupled receptor list Citation for published version: Davenport, AP, Alexander, SPH, Sharman, JL, Pawson, AJ, Benson, HE, Monaghan, AE, Liew, WC, Mpamhanga, CP, Bonner, TI, Neubig, RR, Pin, JP, Spedding, M & Harmar, AJ 2013, 'International Union of Basic and Clinical Pharmacology. LXXXVIII. G protein-coupled receptor list: recommendations for new pairings with cognate ligands', Pharmacological reviews, vol. 65, no. 3, pp. 967-86. https://doi.org/10.1124/pr.112.007179 Digital Object Identifier (DOI): 10.1124/pr.112.007179 Link: Link to publication record in Edinburgh Research Explorer Document Version: Publisher's PDF, also known as Version of record Published In: Pharmacological reviews Publisher Rights Statement: U.S. Government work not protected by U.S. copyright General rights Copyright for the publications made accessible via the Edinburgh Research Explorer is retained by the author(s) and / or other copyright owners and it is a condition of accessing these publications that users recognise and abide by the legal requirements associated with these rights. Take down policy The University of Edinburgh has made every reasonable effort to ensure that Edinburgh Research Explorer content complies with UK legislation. If you believe that the public display of this file breaches copyright please contact [email protected] providing details, and we will remove access to the work immediately and investigate your claim. Download date: 02. Oct. 2021 1521-0081/65/3/967–986$25.00 http://dx.doi.org/10.1124/pr.112.007179 PHARMACOLOGICAL REVIEWS Pharmacol Rev 65:967–986, July 2013 U.S. -

A Computational Approach for Defining a Signature of Β-Cell Golgi Stress in Diabetes Mellitus
Page 1 of 781 Diabetes A Computational Approach for Defining a Signature of β-Cell Golgi Stress in Diabetes Mellitus Robert N. Bone1,6,7, Olufunmilola Oyebamiji2, Sayali Talware2, Sharmila Selvaraj2, Preethi Krishnan3,6, Farooq Syed1,6,7, Huanmei Wu2, Carmella Evans-Molina 1,3,4,5,6,7,8* Departments of 1Pediatrics, 3Medicine, 4Anatomy, Cell Biology & Physiology, 5Biochemistry & Molecular Biology, the 6Center for Diabetes & Metabolic Diseases, and the 7Herman B. Wells Center for Pediatric Research, Indiana University School of Medicine, Indianapolis, IN 46202; 2Department of BioHealth Informatics, Indiana University-Purdue University Indianapolis, Indianapolis, IN, 46202; 8Roudebush VA Medical Center, Indianapolis, IN 46202. *Corresponding Author(s): Carmella Evans-Molina, MD, PhD ([email protected]) Indiana University School of Medicine, 635 Barnhill Drive, MS 2031A, Indianapolis, IN 46202, Telephone: (317) 274-4145, Fax (317) 274-4107 Running Title: Golgi Stress Response in Diabetes Word Count: 4358 Number of Figures: 6 Keywords: Golgi apparatus stress, Islets, β cell, Type 1 diabetes, Type 2 diabetes 1 Diabetes Publish Ahead of Print, published online August 20, 2020 Diabetes Page 2 of 781 ABSTRACT The Golgi apparatus (GA) is an important site of insulin processing and granule maturation, but whether GA organelle dysfunction and GA stress are present in the diabetic β-cell has not been tested. We utilized an informatics-based approach to develop a transcriptional signature of β-cell GA stress using existing RNA sequencing and microarray datasets generated using human islets from donors with diabetes and islets where type 1(T1D) and type 2 diabetes (T2D) had been modeled ex vivo. To narrow our results to GA-specific genes, we applied a filter set of 1,030 genes accepted as GA associated. -

The 'C3ar Antagonist' SB290157 Is a Partial C5ar2 Agonist
bioRxiv preprint doi: https://doi.org/10.1101/2020.08.01.232090; this version posted August 3, 2020. The copyright holder for this preprint (which was not certified by peer review) is the author/funder, who has granted bioRxiv a license to display the preprint in perpetuity. It is made available under aCC-BY-NC-ND 4.0 International license. The ‘C3aR antagonist’ SB290157 is a partial C5aR2 agonist Xaria X. Li1, Vinod Kumar1, John D. Lee1, Trent M. Woodruff1* 1School of Biomedical Sciences, The University of Queensland, St Lucia, 4072 Australia. * Correspondence: Prof. Trent M. Woodruff School of Biomedical Sciences, The University of Queensland, St Lucia, 4072 Australia. Ph: +61 7 3365 2924; Fax: +61 7 3365 1766; E-mail: [email protected] Keywords: Complement C3a, C3aR, SB290157, C5aR1, C5aR2 1 bioRxiv preprint doi: https://doi.org/10.1101/2020.08.01.232090; this version posted August 3, 2020. The copyright holder for this preprint (which was not certified by peer review) is the author/funder, who has granted bioRxiv a license to display the preprint in perpetuity. It is made available under aCC-BY-NC-ND 4.0 International license. Abbreviations used in this article: BRET, bioluminescence resonance energy transfer; BSA, bovine serum albumin; C3aR, C3a receptor C5aR1, C5a receptor 1; CHO-C3aR, Chinese hamster ovary cells stably expressing C3aR; CHO-C5aR1, Chinese hamster ovary cells stably expressing C5aR1; DMEM, Dulbecco's Modified Eagle's Medium; ERK1/2, extracellular signal-regulated kinase 1/2; FBS, foetal bovine serum; HEK293, human embryonic kidney 293 cells; HMDM, human monocyte-derived macrophage; i.p., intraperitoneal; i.v., intravenous; rhC5a, recombinant human C5a; RT, room temperature; S.E.M. -

BD Biosciences New RUO Reagents - November 2020
BD Biosciences New RUO reagents - November 2020 Reactivity Description Format Clone Size Cat. number Hu CD133 FITC W6B3C1 100µg 567029 Hu CD133 FITC W6B3C1 25µg 567033 Hu CD39 PE A1/CD39 100Tst 567156 Hu CD39 PE A1/CD39 25Tst 567157 Hu KIR2DL1/S1/S3/S5 PE HP-MA4 100Tst 567158 Hu KIR2DL1/S1/S3/S5 PE HP-MA4 25Tst 567159 Hu IL-22 Alexa Fluor® 647 MH22B2 100µg 567160 Hu IL-22 Alexa Fluor® 647 MH22B2 25µg 567161 Hu CD99 R718 TU12 50µg 751651 Hu CD161 R718 DX12 50µg 751652 Hu CD116 R718 HGMCSFR-M1 50µg 751653 Hu HLA-G R718 87G 50µg 751670 Hu CD27 R718 O323 50µg 751686 Hu CD80 (B7-1) R718 2D10.4 50µg 751737 Hu Integrin αvβ5 R718 ALULA 50µg 751738 Hu CD266 (Tweak-R) R718 ITEM-4 50µg 751739 Hu ErbB3 (HER-3) R718 SGP1 50µg 751799 Hu TCR Vβ5.1 R718 LC4 50µg 751816 Hu CD123 (IL-3Ra) R718 6H6 50µg 751844 Hu CD1a R718 SK9 50µg 751847 Hu CD20 R718 L27 50µg 751849 Hu Disial GD2 R718 14.G2A 50µg 751851 Reactivity Description Format Clone Size Cat. number Hu CD71 R718 L01.1 50µg 751853 Hu CD278 (ICOS) R718 DX29 50µg 751854 Hu B7-H4 R718 MIH43 50µg 751857 Hu CD53 R718 HI29 50µg 751858 Hu CD197 (CCR7) R718 2-L1-A 50µg 751859 Hu CD197 (CCR7) R718 3D12 50µg 751861 Hu CD31 R718 L133.1 50µg 751863 Hu EGF Receptor R718 EMAB-134 50µg 751864 Hu CD8b R718 2ST8.5H7 50µg 751867 Hu CD31 R718 MBC 78.2 50µg 751869 Hu CD162 R718 KPL-1 50µg 751873 Hu CD24 R718 ML5 50µg 751874 Hu CD159C (NKG2C) R718 134591 50µg 751876 Hu CD169 (Siglec-1) R718 7-239 50µg 751877 Hu CD16b R718 CLB-GRAN11.5 50µg 751880 Hu IgM R718 UCH-B1 50µg 751881 Hu CD275 R718 2D3/B7-H2 50µg 751883 Hu CD307e -

Neutrophil Chemoattractant Receptors in Health and Disease: Double-Edged Swords
Cellular & Molecular Immunology www.nature.com/cmi REVIEW ARTICLE Neutrophil chemoattractant receptors in health and disease: double-edged swords Mieke Metzemaekers1, Mieke Gouwy1 and Paul Proost 1 Neutrophils are frontline cells of the innate immune system. These effector leukocytes are equipped with intriguing antimicrobial machinery and consequently display high cytotoxic potential. Accurate neutrophil recruitment is essential to combat microbes and to restore homeostasis, for inflammation modulation and resolution, wound healing and tissue repair. After fulfilling the appropriate effector functions, however, dampening neutrophil activation and infiltration is crucial to prevent damage to the host. In humans, chemoattractant molecules can be categorized into four biochemical families, i.e., chemotactic lipids, formyl peptides, complement anaphylatoxins and chemokines. They are critically involved in the tight regulation of neutrophil bone marrow storage and egress and in spatial and temporal neutrophil trafficking between organs. Chemoattractants function by activating dedicated heptahelical G protein-coupled receptors (GPCRs). In addition, emerging evidence suggests an important role for atypical chemoattractant receptors (ACKRs) that do not couple to G proteins in fine-tuning neutrophil migratory and functional responses. The expression levels of chemoattractant receptors are dependent on the level of neutrophil maturation and state of activation, with a pivotal modulatory role for the (inflammatory) environment. Here, we provide an overview -

Complement Component 4 Genes Contribute Sex-Specific Vulnerability in Diverse Illnesses
bioRxiv preprint doi: https://doi.org/10.1101/761718; this version posted September 9, 2019. The copyright holder for this preprint (which was not certified by peer review) is the author/funder, who has granted bioRxiv a license to display the preprint in perpetuity. It is made available under aCC-BY-ND 4.0 International license. Complement component 4 genes contribute sex-specific vulnerability in diverse illnesses Nolan Kamitaki1,2, Aswin Sekar1,2, Robert E. Handsaker1,2, Heather de Rivera1,2, Katherine Tooley1,2, David L. Morris3, Kimberly E. Taylor4, Christopher W. Whelan1,2, Philip Tombleson3, Loes M. Olde Loohuis5,6, Schizophrenia Working Group of the Psychiatric Genomics Consortium7, Michael Boehnke8, Robert P. Kimberly9, Kenneth M. Kaufman10, John B. Harley10, Carl D. Langefeld11, Christine E. Seidman1,12,13, Michele T. Pato14, Carlos N. Pato14, Roel A. Ophoff5,6, Robert R. Graham15, Lindsey A. Criswell4, Timothy J. Vyse3, Steven A. McCarroll1,2 1 Department of Genetics, Harvard Medical School, Boston, Massachusetts 02115, USA 2 Stanley Center for Psychiatric Research, Broad Institute of MIT and Harvard, Cambridge, Massachusetts 02142, USA 3 Department of Medical and Molecular Genetics, King’s College London, London WC2R 2LS, UK 4 Rosalind Russell / Ephraim P Engleman Rheumatology Research Center, Division of Rheumatology, UCSF School of Medicine, San Francisco, California 94143, USA 5 Department of Human Genetics, David Geffen School of Medicine, University of California, Los Angeles, California 90095, USA 6 Center for Neurobehavioral Genetics, Semel Institute for Neuroscience and Human Behavior, University of California, Los Angeles, California 90095, USA 7 A full list of collaborators is in Supplementary Information. -
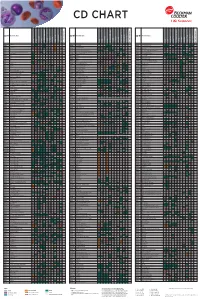
Flow Reagents Single Color Antibodies CD Chart
CD CHART CD N° Alternative Name CD N° Alternative Name CD N° Alternative Name Beckman Coulter Clone Beckman Coulter Clone Beckman Coulter Clone T Cells B Cells Granulocytes NK Cells Macrophages/Monocytes Platelets Erythrocytes Stem Cells Dendritic Cells Endothelial Cells Epithelial Cells T Cells B Cells Granulocytes NK Cells Macrophages/Monocytes Platelets Erythrocytes Stem Cells Dendritic Cells Endothelial Cells Epithelial Cells T Cells B Cells Granulocytes NK Cells Macrophages/Monocytes Platelets Erythrocytes Stem Cells Dendritic Cells Endothelial Cells Epithelial Cells CD1a T6, R4, HTA1 Act p n n p n n S l CD99 MIC2 gene product, E2 p p p CD223 LAG-3 (Lymphocyte activation gene 3) Act n Act p n CD1b R1 Act p n n p n n S CD99R restricted CD99 p p CD224 GGT (γ-glutamyl transferase) p p p p p p CD1c R7, M241 Act S n n p n n S l CD100 SEMA4D (semaphorin 4D) p Low p p p n n CD225 Leu13, interferon induced transmembrane protein 1 (IFITM1). p p p p p CD1d R3 Act S n n Low n n S Intest CD101 V7, P126 Act n p n p n n p CD226 DNAM-1, PTA-1 Act n Act Act Act n p n CD1e R2 n n n n S CD102 ICAM-2 (intercellular adhesion molecule-2) p p n p Folli p CD227 MUC1, mucin 1, episialin, PUM, PEM, EMA, DF3, H23 Act p CD2 T11; Tp50; sheep red blood cell (SRBC) receptor; LFA-2 p S n p n n l CD103 HML-1 (human mucosal lymphocytes antigen 1), integrin aE chain S n n n n n n n l CD228 Melanotransferrin (MT), p97 p p CD3 T3, CD3 complex p n n n n n n n n n l CD104 integrin b4 chain; TSP-1180 n n n n n n n p p CD229 Ly9, T-lymphocyte surface antigen p p n p n -

Molecular Characterization of Clonal Human Renal Forming Cells Cohen-Zontag Osnat , Gershon Rotem , Harari-Steinberg Orit , Kant
bioRxiv preprint doi: https://doi.org/10.1101/2020.03.05.978254; this version posted March 6, 2020. The copyright holder for this preprint (which was not certified by peer review) is the author/funder. All rights reserved. No reuse allowed without permission. Molecular characterization of clonal human renal forming cells Cohen-Zontag Osnat1,7,*, Gershon Rotem1,7,*, Harari-Steinberg Orit1,7,*, Kanter Itamar4, Omer Dorit1,7 , Pleniceanu Oren1,7, Tam Gal4, Oriel Sarit4, Ben-Hur Herzl8,9 , Katz Guy1,3,5,7, Zohar Dotan2,7, Kalisky Tomer4,#, Dekel Benjamin1, 6,7,#,^, Pode- Shakked Naomi1,3,7,#. 1Pediatric Stem Cell Research Institute, Edmond and Lily Safra Children's Hospital, Sheba Medical Center, Tel-Hashomer, Israel 2Dept of Urology, Sheba Medical Center, Tel-Hashomer, Israel 3The Talpiot Medical Leadership Program, Sheba Medical Center, Tel-Hashomer, Israel 4Faculty of Engineering and Bar-Ilan Institute of Nanotechnology and Advanced Materials (BINA), Bar-Ilan University, Ramat Gan, Israel. 5The Joseph Buchman Gynecology and Maternity Center, Sheba Medical Center, Tel- Hashomer, Israel 6Division of Pediatric Nephrology, Edmond and Lily Safra Children's Hospital, Sheba Medical Center, Tel-Hashomer, Israel 7Sackler Faculty of Medicine, Tel-Aviv University, Tel-Aviv, Israel 8L.E.M. Laboratory of Early Detection, Nes Ziona, Israel 9Department of Obstetrics and Gynecology, Assaf Harofeh Medical Center, Tzrifin, Israel *These first authors contributed equally to this work #These senior authors contributed equally to this work ^Correspondence: Benjamin Dekel MD, PhD Pediatric Stem Cell Research Institute Edmond & Lily Safra Children's Hospital, Sheba Medical Center E-mails: [email protected] or [email protected] bioRxiv preprint doi: https://doi.org/10.1101/2020.03.05.978254; this version posted March 6, 2020. -

Human Kidney Clonal Proliferation Disclose Lineage-Restricted Precursor Characteristics
www.nature.com/scientificreports OPEN Human kidney clonal proliferation disclose lineage‑restricted precursor characteristics Osnat Cohen‑Zontag1,7,10, Rotem Gershon1,7,10, Orit Harari‑Steinberg1,7,10, Itamar Kanter4, Dorit Omer1,7, Oren Pleniceanu1,7, Gal Tam4, Sarit Oriel4, Herzel Ben‑Hur8,9, Guy Katz1,3,5,7, Zohar Dotan2,7, Tomer Kalisky4,11, Benjamin Dekel1,6,7,11* & Naomi Pode‑Shakked1,3,7,11 In‑vivo single cell clonal analysis in the adult mouse kidney has previously shown lineage‑restricted clonal proliferation within varying nephron segments as a mechanism responsible for cell replacement and local regeneration. To analyze ex‑vivo clonal growth, we now preformed limiting dilution to generate genuine clonal cultures from one single human renal epithelial cell, which can give rise to up to 3.4 * 106 cells, and analyzed their characteristics using transcriptomics. A comparison between clonal cultures revealed restriction to either proximal or distal kidney sub‑lineages with distinct cellular and molecular characteristics; rapidly amplifying de‑diferentiated clones and a stably proliferating cuboidal epithelial‑appearing clones, respectively. Furthermore, each showed distinct molecular features including cell‑cycle, epithelial‑mesenchymal transition, oxidative phosphorylation, BMP signaling pathway and cell surface markers. In addition, analysis of clonal versus bulk cultures show early clones to be more quiescent, with elevated expression of renal developmental genes and overall reduction in renal identity markers, but with an overlapping expression of nephron segment identifers and multiple identity. Thus, ex‑vivo clonal growth mimics the in‑vivo situation displaying lineage‑restricted precursor characteristics of mature renal cells. These data suggest that for reconstruction of varying renal lineages with human adult kidney based organoid technology and kidney regeneration ex‑vivo, use of multiple heterogeneous precursors is warranted. -

High-Throughput Proteomic Profiling of the Fish Liver Following Bacterial
Causey et al. BMC Genomics (2018) 19:719 https://doi.org/10.1186/s12864-018-5092-0 RESEARCH ARTICLE Open Access High-throughput proteomic profiling of the fish liver following bacterial infection Dwight R Causey1, Moritz A N Pohl1, David A Stead2, Samuel A M Martin1, Christopher J Secombes1 and Daniel J Macqueen1* Abstract Background: High-throughput proteomics was used to determine the role of the fish liver in defense responses to bacterial infection. This was done using a rainbow trout (Oncorhynchus mykiss) model following infection with Aeromonas salmonicida, the causative agent of furunculosis. The vertebrate liver has multifaceted functions in innate immunity, metabolism, and growth; we hypothesize this tissue serves a dual role in supporting host defense in parallel to metabolic adjustments that promote effectiveimmunefunction.Whilepaststudieshavereported mRNA responses to A. salmonicida in salmonids, the impact of bacterial infection on the liver proteome remains uncharacterized in fish. Results: Rainbow trout were injected with A. salmonicida or PBS (control) and liver extracted 48 h later for analysis on a hybrid quadrupole-Orbitrap mass spectrometer. A label-free method was used for protein abundance profiling, which revealed a strong innate immune response along with evidence to support parallel rewiring of metabolic and growth systems. 3076 proteins were initially identified against all proteins (n = 71,293 RefSeq proteins) annotated in a single high-quality rainbow trout reference genome, of which 2433 were maintained for analysis post-quality filtering. Among the 2433 proteins, 109 showed significant differential abundance following A. salmonicida challenge, including many upregulated complement system and acute phase response proteins, in addition to molecules with putative functions that may support metabolic re-adjustments. -

Investigation of the Underlying Hub Genes and Molexular Pathogensis in Gastric Cancer by Integrated Bioinformatic Analyses
bioRxiv preprint doi: https://doi.org/10.1101/2020.12.20.423656; this version posted December 22, 2020. The copyright holder for this preprint (which was not certified by peer review) is the author/funder. All rights reserved. No reuse allowed without permission. Investigation of the underlying hub genes and molexular pathogensis in gastric cancer by integrated bioinformatic analyses Basavaraj Vastrad1, Chanabasayya Vastrad*2 1. Department of Biochemistry, Basaveshwar College of Pharmacy, Gadag, Karnataka 582103, India. 2. Biostatistics and Bioinformatics, Chanabasava Nilaya, Bharthinagar, Dharwad 580001, Karanataka, India. * Chanabasayya Vastrad [email protected] Ph: +919480073398 Chanabasava Nilaya, Bharthinagar, Dharwad 580001 , Karanataka, India bioRxiv preprint doi: https://doi.org/10.1101/2020.12.20.423656; this version posted December 22, 2020. The copyright holder for this preprint (which was not certified by peer review) is the author/funder. All rights reserved. No reuse allowed without permission. Abstract The high mortality rate of gastric cancer (GC) is in part due to the absence of initial disclosure of its biomarkers. The recognition of important genes associated in GC is therefore recommended to advance clinical prognosis, diagnosis and and treatment outcomes. The current investigation used the microarray dataset GSE113255 RNA seq data from the Gene Expression Omnibus database to diagnose differentially expressed genes (DEGs). Pathway and gene ontology enrichment analyses were performed, and a proteinprotein interaction network, modules, target genes - miRNA regulatory network and target genes - TF regulatory network were constructed and analyzed. Finally, validation of hub genes was performed. The 1008 DEGs identified consisted of 505 up regulated genes and 503 down regulated genes.