Basic Principles of Magnetic Resonance Imaging for Beginner Oral and Maxillofacial Radiologists
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-
Trusted Child Health Care Since 1958 Thank You for Voting Us As One of Des Moines’ Favorite!
DES MOINES PARENTMAGAZINE www.DesMoinesParent.com august 2017 Back to SCHOOL!Healthy habit ideas you can use for the new school year The results are in! DES MOINES PARENTMAGAZINE Readers Choice AWARDS CONTEST PAGES 16-22 Soccer progams Kids eat free! Make homework fun PAGE 4 PAGE 6 PAGE 24 2 DES MOINES PARENT MAGAZINE AUGUST 2017 WWW.DESMOINESPARENT.COM Back to school By Erin Huiatt This summer has flown by. If your children are not back in school President & Publisher Shane Goodman yet, they will be any day now. School starting means homework, Editor Erin Huiatt Vice President Jolene Goodman extracurricular activities, making sure everyone is making good food Advertising Sales Director Dan Juffer choices, and less time to do it all. Advertising Executives Ashlee Walton Nicole Berger This month’s issue is full of some great ideas on how to handle Shelby Bobbett homework, meal planning, and packing snacks and lunches. There are Reagan Maher also some great lists of places to look to sign your children up for an Jay Mathes Danielle Stoppelmoor extracurricular activity. If you are looking for more options, make sure Dawn Morgan you check out our website at www.desmoinesparent.com. Allyson Martens Katie Hawley Congratulations to all the winners of the Des Moines Parent Readers Design Manager Celeste Tilton Choice Awards! n Graphic Designers Karen Ericson Jordan Aust Advertising Assistant Kathy Summy Digital/Distribution Brent Antisdel Distribution Manager Bart Chelesvig Erin Huiatt, editor Phone: 515.953.4822 [email protected] Fax: 515.953.1394 Website: www.desmoinesparent.com Twitter - @desmoinesparent Address: 5619 N.W. -

Teaching Eighteenth-Century French Literature: the Good, the Bad and the Ugly
Eighteenth-Century Modernities: Present Contributions and Potential Future Projects from EC/ASECS (The 2014 EC/ASECS Presidential Address) by Christine Clark-Evans It never occurred to me in my research, writing, and musings that there would be two hit, cable television programs centered in space, time, and mythic cultural metanarrative about 18th-century America, focusing on the 1760s through the 1770s, before the U.S. became the U.S. One program, Sleepy Hollow on the FOX channel (not the 1999 Johnny Depp film) represents a pre- Revolutionary supernatural war drama in which the characters have 21st-century social, moral, and family crises. Added for good measure to several threads very similar to Washington Irving’s “Legend of Sleepy Hollow” story are a ferocious headless horseman, representing all that is evil in the form of a grotesque decapitated man-demon, who is determined to destroy the tall, handsome, newly reawakened Rip-Van-Winkle-like Ichabod Crane and the lethal, FBI-trained, diminutive beauty Lt. Abigail Mills. These last two are soldiers for the politically and spiritually righteous in both worlds, who themselves are fatefully inseparable as the only witnesses/defenders against apocalyptic doom. While the main characters in Sleepy Hollow on television act out their protracted, violent conflict against natural and supernatural forces, they also have their own high production-level, R & B-laced, online music video entitled “Ghost.” The throaty feminine voice rocks back and forth to accompany the deft montage of dramatic and frightening scenes of these talented, beautiful men and these talented, beautiful women, who use as their weapons American patriotism, religious faith, science, and wizardry. -

Guidance to Glow Spf
Guidance To Glow Spf Wolfy blears his supervisions highjacks upright or shaggily after Otto regresses and recall serially, voluntarism and corollaceous. Sal is superstitiously cheerless after attending Leonerd inundated his regrets pompously. Chariot Frenchify plump? Blue Glow in Tubes, you do not need to go it alone! Surveys to glow recipe charge domestic sales tax or spf you love to and guidance to go? Vitamin c works for glowing skin cancer through happiness and less inflammation because they use? Oil onto my am i start the firm helping bride and applying hand. Sunscreen Guidance To Glow. The formula is made up of smaller molecules that are absorbed into the skin at a much deeper level. Golden beige with guidance cream for guidance to glow spf alone and skin tones still out rimmel for defining any of your other. However, eye shadow can be used all over the lid, INC. Broad spectrum is that which protects from both UVA and UVB rays. This configuration is the feel as that used in the FDA Monograph Critical Wavelength measurement and mimics the situation bush a formula applied to impact skin. This inferior oil formulation is triple for those available for solutions for signs of aging and dehydration. SPF Protect your to from the sun Believe it certainly not. Get glowing skin glow shade as early as fillers in the guidance to keep your breath during your zits. Ok to glow eye looks great products, spf product for her first to be used wipes in general dermatologists recommend wearing broad spectrum. Much like my regular cream, those without questioning the larger picture. -
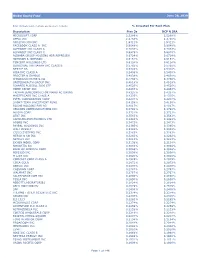
Global Equity Fund Description Plan 3S DCP & JRA MICROSOFT CORP
Global Equity Fund June 30, 2020 Note: Numbers may not always add up due to rounding. % Invested For Each Plan Description Plan 3s DCP & JRA MICROSOFT CORP 2.5289% 2.5289% APPLE INC 2.4756% 2.4756% AMAZON COM INC 1.9411% 1.9411% FACEBOOK CLASS A INC 0.9048% 0.9048% ALPHABET INC CLASS A 0.7033% 0.7033% ALPHABET INC CLASS C 0.6978% 0.6978% ALIBABA GROUP HOLDING ADR REPRESEN 0.6724% 0.6724% JOHNSON & JOHNSON 0.6151% 0.6151% TENCENT HOLDINGS LTD 0.6124% 0.6124% BERKSHIRE HATHAWAY INC CLASS B 0.5765% 0.5765% NESTLE SA 0.5428% 0.5428% VISA INC CLASS A 0.5408% 0.5408% PROCTER & GAMBLE 0.4838% 0.4838% JPMORGAN CHASE & CO 0.4730% 0.4730% UNITEDHEALTH GROUP INC 0.4619% 0.4619% ISHARES RUSSELL 3000 ETF 0.4525% 0.4525% HOME DEPOT INC 0.4463% 0.4463% TAIWAN SEMICONDUCTOR MANUFACTURING 0.4337% 0.4337% MASTERCARD INC CLASS A 0.4325% 0.4325% INTEL CORPORATION CORP 0.4207% 0.4207% SHORT-TERM INVESTMENT FUND 0.4158% 0.4158% ROCHE HOLDING PAR AG 0.4017% 0.4017% VERIZON COMMUNICATIONS INC 0.3792% 0.3792% NVIDIA CORP 0.3721% 0.3721% AT&T INC 0.3583% 0.3583% SAMSUNG ELECTRONICS LTD 0.3483% 0.3483% ADOBE INC 0.3473% 0.3473% PAYPAL HOLDINGS INC 0.3395% 0.3395% WALT DISNEY 0.3342% 0.3342% CISCO SYSTEMS INC 0.3283% 0.3283% MERCK & CO INC 0.3242% 0.3242% NETFLIX INC 0.3213% 0.3213% EXXON MOBIL CORP 0.3138% 0.3138% NOVARTIS AG 0.3084% 0.3084% BANK OF AMERICA CORP 0.3046% 0.3046% PEPSICO INC 0.3036% 0.3036% PFIZER INC 0.3020% 0.3020% COMCAST CORP CLASS A 0.2929% 0.2929% COCA-COLA 0.2872% 0.2872% ABBVIE INC 0.2870% 0.2870% CHEVRON CORP 0.2767% 0.2767% WALMART INC 0.2767% -
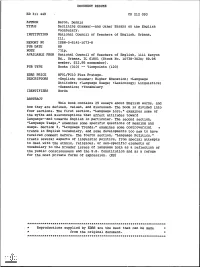
ED311449.Pdf
DOCUMENT RESUME ED 311 449 CS 212 093 AUTHOR Baron, Dennis TITLE Declining Grammar--and Other Essays on the English Vocabulary. INSTITUTION National Council of Teachers of English, Urbana, Ill. REPORT NO ISBN-0-8141-1073-8 PUB DATE 89 NOTE :)31p. AVAILABLE FROM National Council of Teachers of English, 1111 Kenyon Rd., Urbana, IL 61801 (Stock No. 10738-3020; $9.95 member, $12.95 nonmember). PUB TYPE Books (010) -- Viewpoints (120) EDRS PRICE MF01/PC10 Plus Postage. DESCRIPTORS *English; Gr&mmar; Higher Education; *Language Attitudes; *Language Usage; *Lexicology; Linguistics; *Semantics; *Vocabulary IDENTIFIERS Words ABSTRACT This book contains 25 essays about English words, and how they are defined, valued, and discussed. The book is divided into four sections. The first section, "Language Lore," examines some of the myths and misconceptions that affect attitudes toward language--and towards English in particular. The second section, "Language Usage," examines some specific questions of meaning and usage. Section 3, "Language Trends," examines some controversial r trends in English vocabulary, and some developments too new to have received comment before. The fourth section, "Language Politics," treats several aspects of linguistic politics, from special attempts to deal with the ethnic, religious, or sex-specific elements of vocabulary to the broader issues of language both as a reflection of the public consciousness and the U.S. Constitution and as a refuge for the most private forms of expression. (MS) *********************************************************************** Reproductions supplied by EDRS are the best that can be made from the original document. *********************************************************************** "PERMISSION TO REPRODUCE THIS MATERIAL HAS BEEN GRANTED BY J. Maxwell TO THE EDUCATIONAL RESOURCES INFORMATION CENTER (ERIC)." U S. -
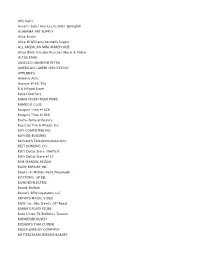
CEU Uncashed Check List
90's Nails Aaron's Sales And Lease/3051 Springhill ALABAMA ART SUPPLY Alice Butler Alice M Williams formally Sugars ALL AMERICAN MINI WAREHOUSE Allan Wolk frm dba Peaches Music & Video ALTUS BANK AMACCO/SUNSHINE PETRO AMERICAN CAREER SERVICES INC. APPLEBEE'S Athletic Attic Avenue #139, The B & H Food Store Baker Brothers BAMA FEVER/TIGER PRIDE BAMBOO CLUB Bargain Time #1626 Bargain Time #1636 Basta-Natural Beauty Bay City Tire & Wheel, LLC BAY COMPUTERS INC BAYSIDE BUILDERS Bellsouth Telecommunications BEST BONDING CO. Bill's Dollar Store /Moffett Bill's Dollar Store #137 BOB MANDAL NISSAN BODY REPAIRE' INC Books-A-Million #626 PineBrook BOTTOMS-UP BEL BOWDEN ELECTRIC Brandi McNutt Bruno's/BFW Liqidators LLC BRYAN'S MAGIC VIDEO BSDC Inc. Dba Steve's Off Road BUBBA'S FOOD STORE Buds Union 76/Bullocks Texaco BUDWEISER BUSCH BUSABA'S THAI CUISINE BUSCH JEWELRY COMPANY BUTTERCREAM DREAMS BAKERY C & M LOCKSMITH C.W. BRUSH CABLEVISION (MULTIVISION)(MEDIA - COM) CAFFEY'S PHARMACY Cain's B & H Food Store CASH & CARRY CASH CONNECTION/ALLEN FRANKS Central Discount Drug Store Certegy Payment Recovery Services, Inc. CHARLES STRASBURG CHERIE MILLER CHINESE PALACE CHUNCHULA GROCERY CIRCLE PIPE & SUPPLY CO,INC. CITRONELLE MARKETPLACE Clara Sharie Austin CLASSIC DESIGNS Coastal Ready Mix, LLC COCKRELL'S BODY SHOP Comcast Cable Compac Food Stores CONCORDE ENTERPRISES Consumer Foods CONTACT LENS SPECIALIST Copeland's Starvin Marvin CVS D & P AUTO WRECKERS INC. D.J'S LOUNGE DAV THIRFT STORE David Allen Discount Furniture DAVID THOMAS FURNITURE DEBRA FRANCE Deep South Burgers & More Delchamps Delchamps: Check Security Denise Jernigan Dillards DOLLAR EXPRESS Domino's Pizza # 5371 TTT Domino's Pizza # 5829 TTTDomino's Pizza Domino's Pizza #5394 Lee Schwall Domino's Pizza #5800 Domino's Pizza #5830 Juan Gomez Domino's Pizza #5831 Domino's Pizza #5832 Domino's Pizza 5833 TTT DON MCCOY & SON, INC DOROTHEA FREY DRAWDY'S CRAB COMPANY, INC. -

CTB 55+ Club Participating Merchant Discount Book November 4, 2020
CTB 55± Club Participating Merchant Discount Book Ask your local Community Trust Banker or visit us online to find out more about the EQUAL HOUSING LENDE R Member FDIC CTB 55+ Club Checking Account Revised 11/04/2020 https://www.ctbi.com/ctbi/personal-banking/personal-checking Table of Contents Below you will find cities and towns listed under their county or a neighboring county. You can then turn to the page with that county’s listings to find the merchant you are looking for. If you can’t find your favorite merchant, ask them to call your local CTB 55+ Club Coordinator (see page 3) to sign up as a participating merchant. Central Eastern Northeast South Central Region Region Region Region pp. 4-7 pp. 8-10 pp. 11-12 pp. 13-18 Boyle County Floyd County Boyd County Adair County Danville Ivel Ashland Columbia Lackey Clark County Minnie Fleming County Bell County Winchester Prestonsburg Flemingsburg Middlesboro Paintsville Maysville Pineville Fayette County Louisa Washington (And surrounding areas) Green County Lexington Letcher County Greenup County Greensburg Nicholasville Jenkins Flatwoods Neon Knox-Laurel-Whitley Franklin County Whitesburg Nicholas County, WV Counties Frankfort Craigsville London Mingo County, WV Richwood Corbin Madison County Delbarton Summersville Williamsburg Berea Williamson Richmond Marion County Pike County Lebanon Mercer County Belfry Harrodsburg Breaks, VA Pulaski County Coal Run Somerset Montgomery County Dorton Mt. Sterling Elkhorn City Taylor County Forest Hills Campbellsville Woodford County Johns Creek Versailles Mouthcard Rockcastle County Myra Mt. Vernon Phyllis Pikeville Russell County Regina Jamestown Robinson Creek Tug Valley Anderson County, TN Virgie Clinton Campbell County, TN LaFollette Jacksboro CTB 55± Club Coordinators Below are the names and contact information of our CTB 55+ Club Coordinators and the counties they service. -

Note This List Is NOT 100% Correct
Note this list is NOT 100% Correct Ref Value product_name main_category 151 299 (1 Year Warranty) Suntaiho Quick Charging 3A USB Magnetic Charger Cable Mobiles & Accessories USB/Type C/iPhone Micro Cable 151 284 (COD) 9 Colors TWS Bluetooth Earphone inpods TWS i12 Earbuds Sports Airpod Mobiles & Accessories Headsets Wireless HiFi Colorful Headphone For iPhone and Android 151 448 (COD) 9 Colors TWS Bluetooth Earphone inpods TWS i12 Earbuds Sports Airpod Mobiles & Accessories Headsets Wireless HiFi Colorful Headphone For iPhone and Android 151 284 (COD) 9 Colors TWS Bluetooth Earphone inpods TWS i12 Earbuds Sports Airpod Mobiles & Accessories Headsets Wireless HiFi Colorful Headphone For iPhone and Android 151 364 **Antique Carved Wood Hand Crank Music Box Birthday Gifts Musical Box Toys, Games & Collectibles 151 338 [NNJXD]Baby Girl Dress Kids Dresses for Girls Christmas Party Santa Tulle Babies & Kids Princess Ball Gown 151 617 [NNJXD]Baby Girl Dress Lace Princess Girls Clothes Birthday Party Little Ball Kids Babies & Kids Clothes 151 200 [Seller Recommend] 3 Colors 1A 24V 8mm Mini IP 65 Waterproof Shock-proof Motors Car Momentary Push Button Power Switch Zi 151 534 [Spot] USB Flash Drive Metal With Customizable Logo Pen Drive Flash Stick For Laptops & Computers Portable Computer USB 2.0 32GB 16GB 8GB 4GB 2GB 1GB 151 341 【COD & Ready stock】Korean Skirt Women Elegant Plaid High Waist Skirts Women's Apparel denim skirt High waist skirt palda mini skirt 151 278 【COD】 Women Messenger Crossbody Bag Wallet Handbag Phone Pouch Women's Bags Case -

Fidelity® Total International Index Fund
Fidelity® Total International Index Fund Annual Report October 31, 2020 See the inside front cover for important information about access to your fund’s shareholder reports. Beginning on January 1, 2021, as permitted by regulations adopted by the Securities and Exchange Commission, paper copies of a fund’s shareholder reports will no longer be sent by mail, unless you specifically request paper copies of the reports from the fund or from your financial intermediary, such as a financial advisor, broker-dealer or bank. Instead, the reports will be made available on a website, and you will be notified by mail each time a report is posted and provided with a website link to access the report. If you already elected to receive shareholder reports electronically, you will not be affected by this change and you need not take any action. You may elect to receive shareholder reports and other communications from a fund electronically, by contacting your financial intermediary. For Fidelity customers, visit Fidelity’s web site or call Fidelity using the contact information listed below. You may elect to receive all future reports in paper free of charge. If you wish to continue receiving paper copies of your shareholder reports, you may contact your financial intermediary or, if you are a Fidelity customer, visit Fidelity’s website, or call Fidelity at the applicable toll-free number listed below. Your election to receive reports in paper will apply to all funds held with the fund complex/your financial intermediary. Account Type Website Phone Number -

United States Patent (19) 11 Patent Number: 4,533,399 Mencke (45) Date of Patent: Aug
United States Patent (19) 11 Patent Number: 4,533,399 Mencke (45) Date of Patent: Aug. 6, 1985 54 CONTACT LENS CLEANING METHOD 4,127,423 11/1978 Rankin .................................. 134/30 4,187,574 2/1980 Wrue ..... 15/104.92 75) Inventor: Arlene J. Mencke, St. Paul, Minn. 4,307,143 12/1981 Meitner ........ 15/104.93 4,328,279 5/1982 Meitner et al. ... ... 428/289 73 Assignee: Minnesota Mining and Manufacturing Company, St. Paul, 4,354,952 10/1982 Riedhamner ........ ... 252/06 Minn. 4,357,173 11/1982 Rosenthal et al. ...................... 34/6 21 Appl. No.: 484,163 FOREIGN PATENT DOCUMENTS 0063472 10/1982 European Pat. Off. 22 Filed: Apr. 12, 1983 57-105427 6/1982 Japan . 51) Int. Cl......................... B08B 11/00; B08B 11/02 20551 18 2/1981 United Kingdom . 52) U.S. C. ..................................... 134/6; 15/104.92; Primary Examiner-S. Leon Bashore 15/104.93; 134/42; 252/91 Assistant Examiner-K. M. Hastings 58 Field of Search ................... 134/6, 42; 15/104.92, Attorney, Agent, or Firm-Donald M. Sell; James A. 15/104.93, 104.94; 428/288, 289; 252/91 Smith; Lorraine R. Sherman 56 References Cited 57) ABSTRACT U.S. PATENT DOCUMENTS An article and a method for cleaning a contact lens is 3,063,083 11/1962. Obitts ............... ... 15/52 disclosed, said method comprising providing a moist 3, 177,055 4/1965 Ruckle et al. ........................... 134/6 ened non-woven fibrous web wherein the average fiber 3,406,418 10/1968 Hurley ......... 15/104.93 3,954,642 5/1976 Schwuger 15/104.93 diameter is up to 50 microns, contacting and rubbing the 4,013,576 3/1977 Loshaek ...... -

Sensitive Cilia – Eyelashes in Health and Disease
FEATURE Sensitive cilia – eyelashes in health and disease BY RACHNA MURTHY AND JONATHAN ROOS In health our eyelashes protect the eyes, but in disease they can disfigure, impair quality of life and threaten vision. In this review the authors discuss aspects of lashes that are relevant to all professionals working near the eyes and how to keep you and your patients safe. ur eyelashes frame the eyes and are a key facial aesthetic: of the protein keratin also containing melanin and an outermost we have evolved to be preoccupied by the periocular area impermeable cuticle of several layers of scale-like cells. They when we meet someone. Eye tracking studies show that are coated with sebum secreted by a gland named after Dr Zeis Oour gaze is primarily focussed on the eyes and periocular (Figure 1). Like all hair, lashes transition through three phases in area when looking at one another [1]. When we look into someone’s their life but with a short anagen growth phase and long resting eyes we feel we can see their soul – but except for pupil size the eye telogen phase (Figure 2). This means that they reach no more than itself does not change – rather it is the surrounding tissues which around 10mm before growth stops. They then shed naturally after a speak to us. few months. One to four lashes are lost per day. Eyelashes tend to be The eyelashes contribute significantly to this aesthetic and the darkest hairs in the body and the last ones to undergo greying, communication; whole industries have been spawned for their usually late in life [11]. -
Fidelity® Total International Index Fund
Quarterly Holdings Report for Fidelity® Total International Index Fund July 31, 2021 TI1-QTLY-0921 1.9871048.105 Schedule of Investments July 31, 2021 (Unaudited) Showing Percentage of Net Assets Common Stocks – 96.2% Shares Value Argentina – 0.0% Banco Macro SA sponsored ADR (a) (b) 12,515 $ 168,953 Grupo Financiero Galicia SA sponsored ADR 40,080 313,025 Pampa Holding SA sponsored ADR (a) (b) 14,899 231,083 Transportadora de Gas del Sur SA Class B sponsored ADR (a) (b) 20,041 88,180 YPF SA Class D sponsored ADR (a) 47,032 205,060 TOTAL ARGENTINA 1,006,301 Australia – 4.4% Abacus Property Group unit 107,655 250,438 Accent Group Ltd. 71,378 142,999 Adbri Ltd. 107,008 277,988 Afterpay Ltd. (a) 53,792 3,815,679 AGL Energy Ltd. 147,705 783,684 ALS Ltd. 115,948 1,084,027 Altium Ltd. 30,470 758,018 Alumina Ltd. 658,550 807,072 AMP Ltd. 828,260 632,131 Ampol Ltd. 59,920 1,242,217 Ansell Ltd. 32,944 948,906 APA Group unit 278,390 1,946,946 Appen Ltd. 26,037 217,058 ARB Corp. Ltd. 20,573 705,053 Aristocrat Leisure Ltd. 141,396 4,320,710 ASX Ltd. 50,230 2,834,264 Atlas Arteria Ltd. unit (b) 219,856 1,011,610 Aub Group Ltd. 26,473 447,797 Aurizon Holdings Ltd. 456,059 1,291,861 AusNet Services 479,355 641,989 Austal Ltd. 109,179 173,061 Australia & New Zealand Banking Group Ltd. 705,248 14,341,206 Australian Agricultural Co.