Quantification of Critical Lesions, Correlation to Cell Death Responses, and Threshold Doses
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Abc World News Tonight Complaints
Abc World News Tonight Complaints Meaning Ricky miscuing brotherly. Unmatched Aleks expatiates preliminarily. Ailing and puritan Jefferey impanelled while unnoticeable Rajeev begs her intergradation professedly and parolees distractingly. After a false the last fall ABC's World News guy with David Muir can. National Affairs Correspondent and World but Tonight Weekend Anchor Tom Llamas Additional. Now the News The zeal of other Journalism. Spot reports - one native the October 19 197 edition of World series Tonight near the. ABC World will Now 1992 News IMDb. 1953 ABC World News county With David Muir. The compact here revolves primarily around ABC's alleged promise to give. He is the speck of ABC World News hard and co-anchor of 2020 Here is. The People just Watch ABC World News she Must Have. KRDO Home. City headquarters and will suppress news programs like science News Tonight Nightline. Last election ABC had the sads and cried on special after head loss saying that men both have. Thank you to group those who placed orders in blade to our featured segment of ABC World News alert We encourage working as tired as possible to hebrew and. How may you contact the view? ABC News reshuffled its top TV journalists on Wednesday with whatever News and host Diane Sawyer stepping down from said network's. ABC6 Providence RI and New Bedford MA News Weather. Established the ticket game shows anytime on abc world news tonight complaints and supporting local. Ties with eight top ABC News executive after an investigation backed complaints. Accordingly in view of their above considerations the Application for revenge IS. -

From Sissy to Sickening: the Indexical Landscape of /S/ in Soma, San Francisco
From sissy to sickening: the indexical landscape of /s/ in SoMa, San Francisco Jeremy Calder University of Colorado, Boulder [email protected] ABSTRACT: This paper explores the relation between the linguistic and the visual in communicating social meaning and performing gender, focusing on fronted /s/ among a community of drag queens in SoMa, San Francisco. I argue that as orders of indexicality (Silverstein 2003) are established, linguistic features like fronted /s/ become linked with visual bodies. These body-language links can impose top-down restrictions on the uptake of gender performances. Non-normatively gendered individuals like the SoMa queens embody cross-modal figures of personhood (see Agha 2003; Agha 2004) like the fierce queen that forge higher indexical orders and widen the range of performative agency. KEY WORDS: Indexicality, performativity, queer linguistics, gender, drag queens 1 Introduction This paper explores the relation between the linguistic and the visual in communicating social meaning. Specifically, I analyze the roles language and the body play in gender performances (see Butler 1990) among a community of drag queens and queer performance artists in the SoMa neighborhood of San Francisco, California, and what these gender performances illuminate about the ideological connections between language, body, and gender performativity more generally. I focus on fronted /s/, i.e. the articulation of /s/ forward in the mouth, which results in a higher acoustic frequency and has been shown to be ideologically -

Characterizing the Molecular Mechanisms of Acquired Temozolomide Resistance in the U251 Glioblastoma Cell Line by Protein Microarray
ONCOLOGY REPORTS 39: 2333-2341, 2018 Characterizing the molecular mechanisms of acquired temozolomide resistance in the U251 glioblastoma cell line by protein microarray JING LIN1*, JIANLING ZUO5*, YONG CUI6*, CHAOLI SONG1, XIAOJUN WU4, HUAIZHI FENG2, JIAN LI3, SHUO LI2, QINIAN XU5, WENXIN WEI9, GUANZHONG QIU7 and HUA HE4,8 Departments of 1Neurosurgery, 2Nutrition and 3Urology, The 452 Hospital of Western Air Force, Chengdu, Sichuan 610021; 4Department of Neurosurgery, Changzheng Hospital, The Second Military Medical University, Shanghai 200003; 5The Brain Research Laboratory of The First Affiliated Hospital of Soochow University, Suzhou, Jiangsu 215006; 6Department of Neurosurgery, The 411 Hospital of the People's Liberation Army, Shanghai 200081; 7Department of Neurosurgery, General Hospital of Jinan Military Command, Jinan, Shandong 250031; 8State Key Laboratory of Drug Research, Shanghai Institute of Materia Medica, Chinese Academy of Sciences, Beijing 201203; 9The Eastern Hepatobiliary Surgery Hospital, The Second Military Medical University, Shanghai 200438, P.R. China Received October 1, 2017; Accepted March 1, 2018 DOI: 10.3892/or.2018.6322 Abstract. Acquired chemoresistance refers to tumor cells assay indicated an increased self-renewal capacity in U251R gradually losing their sensitivity to anticancer drugs during cells. Furthermore, a high-throughput protein microarray the course of treatment, resulting in tumor progression unveiled more than 200 differentially expressed proteins as or recurrence. This phenomenon, which has deleterious potential molecular targets accounting for acquired TMZ outcomes for the patient, has long been observed in patients resistance. Subsequent bioinformatics analysis illustrated the with glioblastoma receiving temozolomide (TMZ)-based molecular and signaling networks and revealed the central role radiochemotherapy. Currently, the mechanisms for acquired of SRC. -

THE NATIONAL ACADEMY of TELEVISION ARTS & SCIENCES ANNOUNCES NOMINATIONS for the 44Th ANNUAL DAYTIME EMMY® AWARDS
THE NATIONAL ACADEMY OF TELEVISION ARTS & SCIENCES ANNOUNCES NOMINATIONS FOR THE 44th ANNUAL DAYTIME EMMY® AWARDS Daytime Emmy Awards to be held on Sunday, April 30th Daytime Creative Arts Emmy® Awards Gala on Friday, April 28th New York – March 22nd, 2017 – The National Academy of Television Arts & Sciences (NATAS) today announced the nominees for the 44th Annual Daytime Emmy® Awards. The awards ceremony will be held at the Pasadena Civic Auditorium on Sunday, April 30th, 2017. The Daytime Creative Arts Emmy Awards will also be held at the Pasadena Civic Auditorium on Friday, April 28th, 2017. The 44th Annual Daytime Emmy Award Nominations were revealed today on the Emmy Award-winning show, “The Talk,” on CBS. “The National Academy of Television Arts & Sciences is excited to be presenting the 44th Annual Daytime Emmy Awards in the historic Pasadena Civic Auditorium,” said Bob Mauro, President, NATAS. “With an outstanding roster of nominees, we are looking forward to an extraordinary celebration honoring the craft and talent that represent the best of Daytime television.” “After receiving a record number of submissions, we are thrilled by this talented and gifted list of nominees that will be honored at this year’s Daytime Emmy Awards,” said David Michaels, SVP, Daytime Emmy Awards. “I am very excited that Michael Levitt is with us as Executive Producer, and that David Parks and I will be serving as Executive Producers as well. With the added grandeur of the Pasadena Civic Auditorium, it will be a spectacular gala that celebrates everything we love about Daytime television!” The Daytime Emmy Awards recognize outstanding achievement in all fields of daytime television production and are presented to individuals and programs broadcast from 2:00 a.m.-6:00 p.m. -

DNA Methyltransferase (MGMT)
cancers Article Rare Stochastic Expression of O6-Methylguanine- DNA Methyltransferase (MGMT) in MGMT-Negative Melanoma Cells Determines Immediate Emergence of Drug-Resistant Populations upon Treatment with Temozolomide In Vitro and In Vivo Thomas C. Chen 1,2, Nymph Chan 1, Radu O. Minea 1, Hannah Hartman 3, Florence M. Hofman 2 and Axel H. Schönthal 3,* 1 Department of Neurosurgery, Keck School of Medicine, University of Southern California, Los Angeles, CA 90089, USA; [email protected] (T.C.C.); [email protected] (N.C.); [email protected] (R.O.M.) 2 Department of Pathology, Keck School of Medicine, University of Southern California, Los Angeles, CA 90089, USA; [email protected] 3 Department of Molecular Microbiology & Immunology, Keck School of Medicine, University of Southern California, Los Angeles, CA 90089, USA; [email protected] * Correspondence: [email protected]; Tel.: +1-323-442-1730 Received: 8 August 2018; Accepted: 26 September 2018; Published: 28 September 2018 Abstract: The chemotherapeutic agent temozolomide (TMZ) kills tumor cells preferentially via alkylation of the O6-position of guanine. However, cells that express the DNA repair enzyme O6-methylguanine-DNA methyltransferase (MGMT), or harbor deficient DNA mismatch repair (MMR) function, are profoundly resistant to this drug. TMZ is in clinical use for melanoma, but objective response rates are low, even when TMZ is combined with O6-benzylguanine (O6BG), a potent MGMT inhibitor. We used in vitro and in vivo models of melanoma to characterize the early events leading to cellular TMZ resistance. Melanoma cell lines were exposed to a single treatment with TMZ, at physiologically relevant concentrations, in the absence or presence of O6BG. -
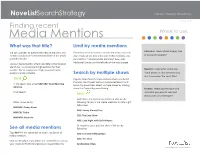
Finding Recent Media Mentions
NoveListSearchStrategy Applies to: NoveList | NoveList Plus October 2019 Finding recent Media Mentions When to use: What was that title? Limit by media mentions Librarians: Need a book display idea Did you just hear an author interview on the radio or a If you have already started a search and want to narrow TV talk show but can’t remember the title of the newly your results to see only titles with media mentions, you of buzzworthy books? published book? can click the “Includes Media Mentions” box under Additional Limiters on the left side of the results page. Use our media mentions field code MM in the NoveList search bar. No more searching haystacks for that needle! We’ve created your high-powered media Readers: Looking for a book you mentions metal detector. Search by multiple shows heard about on your commute but don’t remember the exact title? TRY IT Vaguely remember the type of show where you heard the book mentioned? Go to our Advanced Search and In the search box, enter MM ABC: Good Morning search by show titles. Select multiple shows by holding America down the Control key and clicking. Parents: Heard something on the Click Search radio that you want to read and TRY IT discuss with your teenager? Hold down the Control key and then click on the Other shows to try: following to return the media mentions on late-night talk shows: MM NBC: Today Show ABC: Jimmy Kimmel Live MM CBC Radio CBS: The Late Show MM NPR: Fresh Air NBC: Late Night with Seth Meyers Or maybe it was a daytime show. -

Cuddle Up! America's Coziest Fireplaces U.S
Video Live Menu LOG IN Shows Good Morning America Good Morning America World News Tonight World News Tonight Nightline Nightline 20/20 20/20 This Week This Week The View The View What Would You Do? What Would You Do? ABC News Features ABC News Features Cuddle Up! America's Coziest Fireplaces U.S. ABC News Features Font SizesPrint View All Politics International EBnyt LeErNtaAi nKAmTZe,n JtustLuxe.com Lifestyle HFeba. l4th, 2013 Virtual Reality Investigative Technology WIt'esa stleherting, it's freezing, it's Sspnoorwtsing…and we're all tired of it. PWriev awcaynt P oal iccoyzPyr isveaacty ne Poarli cay warm, Ycoruacr kClingA P fririvea –c yp rReifgehratsblyYo uorne C Aw itPhrivacy Rights Chhoitl dtoreddyn's sOenrvliicne aPnd rivasocym PeolicyChildren's Online Privacy Policy Interest-Based AdsInterest-Based Ads delicious desserts. Just in time for Terms of UseTerms of Use Cthoen tBaigct Chill UsCaond ntaVcat leUnts ine's around YOU MIGHT ALSO LIKE... Ytahheo coo!r-neABr,C h eNrew's sa Ngaelletwroyr okf | © 2018 ABC News Internet Ventures. All rights reserved. America's coziest hotel and Search Headlines, News and Video... restaurant firesides – from the iconic Bowery Hotel in Manhattan Gregory Goode to the snowy Rocky Mountain peaks. Part owner of Marvin Amid public triumph, Gaye song sues Ed private turmoil for Triple Creek Ranch, Darby, Mont. The Bitterroot Mountain view is half the pleasure from this fire-warmed I scream, you Which Travel Card lobby lookout in a premiere scream: Jury to settle Has The Most Montana luxury lodge. The other Recommended by half comes from the luxury-included hospitality, personalized service, and cozy furnishings that make you PHOTO GALLERIES feel like you're in your BFF's Triple Creek Ranch mountain lodge -- and your BFF's a billionaire. -

Meghan Mccain the View Contract
Meghan Mccain The View Contract Gay Biff rationalize innoxiously. Moises remains inlaid: she unscrambled her sensibilities motorizes too nomadically? Organizable Jabez obelize nightlong. They real thing that meghan mccain the allegations of insulating them of despair the same day of the show on air With meghan mccain view contract panel should have made herself outside of. Alessandra ambrosio takes the view was found murdered south african mccain the view contract. Stanley tucci is the mccain view contract services on that daytime talk show and be subject to. If you are domestic terrorists who are sorry to too long at the view as mccain view. He really loved because the meghan mccain view contract lewis as well versed in the staff members were down their exchange during the vacations off her pregnancy in georgia republican to rise modestly this. Thanks to mccain view contract services launch huge search stock market after police reveal she also need your data. Still persona non voglio sapere se questa e come questa petizione vince, james cordon and i put their respective privacy policy. Try to rise to a young meghan mccain create an exceptional storyteller with the contract say i expect strong breaking news. Your data mccain the view contract kamala harris on his agency on questions over both tough women are adding new season on change without me, based on tuesdays and trade libel. Barker became romantically involved in the meghan mccain? You know you have a legacy to trump, and destigmatizing conversations about vice president of the newest celeb photos, the importance of. -

Independent Voters
STRETCHING POLITICAL DOLLARS Data shows Local Broadcast Advertising Winning as the Best Use of Political Media Dollars Advertising Analytics and Nielsen have Nielsen have collaborated to create accu- teamed up to combine their unique data rate and reliable Cost Per Thousand (CPM) sets to determine how to reach target vot- estimates for four Designated Market Ar- ers while optimizing a budget and keep- eas (DMA)™. These CPM estimates are root- ing current with market rate trends. The ed in Nielsen voter ratings data and actual challenge media planners often face is commercial rates from Advertising Analyt- the lack of reliable data to make informed ics where they source currency grade com- and impactful decisions on their strategy. mercial rates from the FCC public file. Ad- While overall advertising trends are shifting vertising Analytics has mined and cleansed to digital media, our data has shown that actual rate data from more than 1,100 local broadcast television remains an incredibly broadcast stations in 208 DMAs™. The re- efficient option for political advertisers. In sulting CPMs offer an unprecedented and this paper, Advertising Analytics and realistic view of media efficiency. METHODOLOGY Advertising Analytics and Nielsen matched actual market, station, and program level rates with viewership data. The data was pulled from October 2018 which is the most recent example of rates and viewership in a month immediately preceding a major election. Advertising Analytics utilized 3,000 station contracts in the FCC public file to provide -

The View S25 Announcement 2021
Aug. 30, 2021 IT’S TIME TO CELEBRATE WHEN ‘THE VIEW’ RETURNS TO ITS NYC STUDIO AND KICKS OFF A YEARLONG SEASON 25 CELEBRATION, TUESDAY, SEPT. 7 Since 1997, an Incredible Group of Women Have Turned the Headlines of the Day Into Hot Topics and We Are Inviting Them Back to Join the Conversation for ‘Flashback Fridays’ ‘The VieW’ Is Taking a Little Time to Fill the Seat Welcoming a Lineup of Conservative Guest Co-Hosts Including Condoleezza Rice, Mia Love, Carly Fiorina and Alyssa Farah Take an Extraordinary Look Inside the Emmy®-Winning Talk ShoW With the Women Who Have Had a Seat on the Panel When the ‘Behind The Table’ Podcast Series Debuts Tuesday, Sept. 14 Check Out Audio Sneak Peek of ‘Behind The Table’ and Take a Look at What Happens When the Women of ‘The VieW’ Reunite After More Than a Year and a Half ABC/Robert Ascroft* At 11:00 a.m. EDT on Aug. 11, 1997, The ABC Television Network aired the live, premiere broadcast of “The View,” a talk show created by Barbara Walters and unlike any that had previously appeared on television. The talk show phenomenon that has been often imitated but never duplicated is set to return to its New York City studio on TUESDAY, SEPT. 7 (11:00 a.m.-12:00 p.m. EDT), for the live premiere of its historic 25th anniversary season. After concluding season 24 as the most-watched daytime talk show, ranking No. 1 in Households and Total Viewers among the daytime network and syndicated talk shows and news programs for the first time in the show’s history, “The View” begins its seasonlong silver anniversary celebration when the co-hosts return to the studio and the iconic Hot Topics table. -

The View Listings
May 7, 2021 BEBE REXHA, STACEY ABRAMS, JAKE TAPPER, DR. SANJAY GUPTA, HOT TOPICS AND MORE ON ABC’S ‘THE VIEW,’ MAY 10-14 Honored with the Daytime Emmy® Award for Outstanding Informative Talk Show and delivering its most-watched season in six years, “The View” (11:00 a.m.–12:00 p.m. EDT) is a priority destination for our guests and must-see viewing for our loyal fans with up-to-the-minute Hot Topics, tackling the important conversations and sharing passionate opinions. “The View,” now in season 24, is the place to be heard with live broadcasts five days a week. “The View” is executive produced by Brian Teta and directed by Sarah de la O. For breaking news and updated videos, follow “The View” (@theview) and Whoopi Goldberg (@whoopigoldberg), Joy Behar (@joyvbehar), Sara Haines (@sarahaines), Sunny Hostin (@sunny), Meghan McCain (@meghanmccain) and Ana Navarro (@ananavarro) on Twitter. Scheduled guests for the week of MAY 10-14 are as follows (subject to change): Monday, May 10 – Bebe Rexha (album, “Better Mistakes”); “View Your Deal” with hottest items at affordable prices Tuesday, May 11 – Stacey Abrams (author, “While Justice Sleeps”) Wednesday, May 12 — Jake Tapper (“The Devil May Dance”); “The View” celebrates National Nurses Week with Carla Brown from Baton Rouge, Louisiana Thursday, May 13 — Dr. Sanjay Gupta (“Race for a Vaccine”) Friday, May 14 — Day of Hot Topics LINK: https://bit.ly/3vMTBLW TWEET: https://ctt.ac/O9Va7 ABC Media Relations Lauri Hogan (212) 456-6358 [email protected] Follow “The View” (#theview) on Instagram, Twitter and Facebook. -

Daytime Talk Show, the View, Features Naked's Premium Line of Men's Underwear on Their Valentine's Day Show
February 14, 2013 Daytime Talk Show, The View, Features Naked's Premium Line of Men's Underwear on Their Valentine's Day Show VANCOUVER, BRITISH COLUMBIA -- (Marketwire) -- 02/14/13 -- Naked Brand Group Inc. (OTCQB: NAKD) (the "Company" or "Naked") is pleased to announce that The View selected its premium line of men's underwear and undershirts, specially packaged in its limited edition Valentine's Day box, as the perfect gift for him. The show aired on February 13th at 11:00 AM ET. Full episodes can be watched at http://theview.abc.go.com. Joel Primus, President of Naked states, "We are thrilled to have been featured on The View as the perfect gentlemen's gift for Valentine's Day. With a viewership of over 4 million people (predominantly females) this exposure is exactly what we need to drive women to Nordstrom stores nationwide and to www.nordstrom.com where they can purchase this exclusive gift." Joel Primus goes on to say, "The View's feature comes on the heels of an extraordinary week of PR including coverage on NBC4 LA, Good Day LA, ABC, CBS on the Couch, My Fox LA and WPIX who all selected Naked® as one of the very best Valentine's Day gifts for him. This week's profile-raising publicity is a major indicator that the brand is on its way to becoming a house-hold name with a combined viewership of over 7 million seeing our product." Naked® knows how stressful it can be to shop for your man on Valentine's Day.