1 Suramin Potently Inhibits Binding of the Mammalian High
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Human Stem Cells from Single Blastomeres Reveal Pathways of Embryonic Or Trophoblast Fate Specification Tamara Zdravkovic1,2,3,4,5,‡, Kristopher L
© 2015. Published by The Company of Biologists Ltd | Development (2015) 142, 4010-4025 doi:10.1242/dev.122846 STEM CELLS AND REGENERATION RESEARCH ARTICLE Human stem cells from single blastomeres reveal pathways of embryonic or trophoblast fate specification Tamara Zdravkovic1,2,3,4,5,‡, Kristopher L. Nazor6,‡, Nicholas Larocque1,2,3,4,5, Matthew Gormley1,2,3,4,5, Matthew Donne1,2,3,7, Nathan Hunkapillar1,2,3,4,5, Gnanaratnam Giritharan8, Harold S. Bernstein4,9, Grace Wei4,10, Matthias Hebrok10, Xianmin Zeng11, Olga Genbacev1,2,3,4,5, Aras Mattis4,12, Michael T. McMaster4,5,13, Ana Krtolica8,*, Diana Valbuena14, Carlos Simón14, Louise C. Laurent6,15, Jeanne F. Loring6 and Susan J. Fisher1,2,3,4,5,7,§ ABSTRACT INTRODUCTION For many reasons, relatively little is known about human Mechanisms of initial cell fate decisions differ among species. To gain preimplantation development. The small number of cells makes insights into lineage allocation in humans, we derived ten human embryos of any species difficult to study. In humans, the technical embryonic stem cell lines (designated UCSFB1-10) from single difficulties are compounded by other challenges. Genetic variation blastomeres of four 8-cell embryos and one 12-cell embryo from a among individuals could contribute to developmental differences, a single couple. Compared with numerous conventional lines from well-appreciated phenomenon in the mouse (Dackor et al., 2009), blastocysts, they had unique gene expression and DNA methylation which is difficult to assess in humans owing to the limited patterns that were, in part, indicative of trophoblast competence. At a availability of embryos that are donated for research. -

Homeobox Gene Expression Profile in Human Hematopoietic Multipotent
Leukemia (2003) 17, 1157–1163 & 2003 Nature Publishing Group All rights reserved 0887-6924/03 $25.00 www.nature.com/leu Homeobox gene expression profile in human hematopoietic multipotent stem cells and T-cell progenitors: implications for human T-cell development T Taghon1, K Thys1, M De Smedt1, F Weerkamp2, FJT Staal2, J Plum1 and G Leclercq1 1Department of Clinical Chemistry, Microbiology and Immunology, Ghent University Hospital, Ghent, Belgium; and 2Department of Immunology, Erasmus Medical Center, Rotterdam, The Netherlands Class I homeobox (HOX) genes comprise a large family of implicated in this transformation proces.14 The HOX-C locus transcription factors that have been implicated in normal and has been primarily implicated in lymphomas.15 malignant hematopoiesis. However, data on their expression or function during T-cell development is limited. Using degener- Hematopoietic cells are derived from stem cells that reside in ated RT-PCR and Affymetrix microarray analysis, we analyzed fetal liver (FL) in the embryo and in the adult bone marrow the expression pattern of this gene family in human multipotent (ABM), which have the unique ability to self-renew and thereby stem cells from fetal liver (FL) and adult bone marrow (ABM), provide a life-long supply of blood cells. T lymphocytes are a and in T-cell progenitors from child thymus. We show that FL specific type of hematopoietic cells that play a major role in the and ABM stem cells are similar in terms of HOX gene immune system. They develop through a well-defined order of expression, but significant differences were observed between differentiation steps in the thymus.16 Several transcription these two cell types and child thymocytes. -

An Ontogenetic Switch Drives the Positive and Negative Selection of B Cells
An ontogenetic switch drives the positive and negative selection of B cells Xijin Xua, Mukta Deobagkar-Lelea, Katherine R. Bulla, Tanya L. Crockforda, Adam J. Meadb, Adam P. Cribbsc, David Simsc, Consuelo Anzilottia, and Richard J. Cornalla,1 aMedical Research Council Human Immunology Unit, Weatherall Institute of Molecular Medicine, University of Oxford, OX3 9DS Oxford, United Kingdom; bMedical Research Council Molecular Haematology Unit, Weatherall Institute of Molecular Medicine, University of Oxford, OX3 9DS Oxford, United Kingdom; and cMedical Research Council, Weatherall Institute of Molecular Medicine, Centre for Computational Biology, Weatherall Institute of Molecular Medicine, University of Oxford, OX3 9DS Oxford, United Kingdom Edited by Michael Reth, University of Freiburg, Freiburg, Germany, and approved January 6, 2020 (received for review September 3, 2019) + Developing B cells can be positively or negatively selected by self- BM HSCs increased CD5 B-1a B cell development (15), while antigens, but the mechanisms that determine these outcomes are expression of let-7b in FL pro-B cells blocked the development of incompletely understood. Here, we show that a B cell intrinsic B-1 B cells (17). These findings support the notion of hard-wired switch between positive and negative selection during ontogeny differences during ontogeny, but possibly downstream of the HSC is determined by a change from Lin28b to let-7 gene expression. commitment stage. Ectopic expression of a Lin28b transgene in murine B cells restored Several lines of evidence also suggest that B-1 B cells can un- the positive selection of autoreactive B-1 B cells by self-antigen in dergo positive selection, which is linked to their B cell receptor adult bone marrow. -

Geminin Deletion Increases the Number of Fetal Hematopoietic Stem Cells by Affecting the Expression of Key Transcription Factors Dimitris Karamitros1,*, Alexandra L
© 2015. Published by The Company of Biologists Ltd | Development (2015) 142, 70-81 doi:10.1242/dev.109454 RESEARCH ARTICLE STEM CELLS AND REGENERATION Geminin deletion increases the number of fetal hematopoietic stem cells by affecting the expression of key transcription factors Dimitris Karamitros1,*, Alexandra L. Patmanidi1,*, Panoraia Kotantaki1, Alexandre J. Potocnik2, Tomi Bähr-Ivacevic3, Vladimir Benes3, Zoi Lygerou4, Dimitris Kioussis2,‡ and Stavros Taraviras1,‡ ABSTRACT hematological stress and challenges (Beerman et al., 2010; Balancing stem cell self-renewal and initiation of lineage specification Cheshier et al., 2007). The prevailing model of hematopoiesis programs is essential for the development and homeostasis of the supports the existence of long-term hematopoietic stem cells (LT- hematopoietic system. We have specifically ablated geminin in the HSCs), which can provide long-term multipotent reconstitution of developing murine hematopoietic system and observed profound the hematopoietic system, and of short-term hematopoietic stem defects in the generation of mature blood cells, leading to embryonic cells (ST-HSCs) or multipotent progenitors (MPPs), with the lethality. Hematopoietic stem cells (HSCs) accumulated in the fetal potential to generate all blood lineages but with reduced self- liver following geminin ablation, while committed progenitors were renewal capacity (Luc et al., 2007; Mebius et al., 2001; Morrison reduced. Genome-wide transcriptome analysis identified key HSC et al., 1995; Randall et al., 1996; Traver et al., 2001). transcription factors as being upregulated upon geminin deletion, Even though it remains unclear how the balance between self- revealing a gene network linked with geminin that controls fetal renewal of HSCs and fate commitment is controlled and how a hematopoiesis. -

C/Ebpα Is an Essential Collaborator in Hoxa9/Meis1-Mediated Leukemogenesis
C/EBPα is an essential collaborator in Hoxa9/Meis1-mediated leukemogenesis Cailin Collinsa, Jingya Wanga, Hongzhi Miaoa, Joel Bronsteina, Humaira Nawera, Tao Xua, Maria Figueroaa, Andrew G. Munteana, and Jay L. Hessa,b,1 aDepartment of Pathology, University of Michigan, Ann Arbor, MI 48109; and bIndiana University School of Medicine, Indianapolis, IN 46202 Edited* by Louis M. Staudt, National Institutes of Health, Bethesda, MD, and approved May 19, 2014 (received for review February 12, 2014) Homeobox A9 (HOXA9) is a homeodomain-containing transcrip- with Hoxa9. In addition, C/EBP recognition motifs are enriched tion factor that plays a key role in hematopoietic stem cell expan- at Hoxa9 binding sites. sion and is commonly deregulated in human acute leukemias. A C/EBPα is a basic leucine-zipper transcription factor that plays variety of upstream genetic alterations in acute myeloid leukemia a critical role in lineage commitment during hematopoietic dif- −/− (AML) lead to overexpression of HOXA9, almost always in associ- ferentiation (18). Whereas Cebpa mice show complete loss of ation with overexpression of its cofactor meis homeobox 1 (MEIS1). the granulocytic compartment, recent work shows that loss of α A wide range of data suggests that HOXA9 and MEIS1 play a syn- C/EBP in adult HSCs leads to both an increase in the number ergistic causative role in AML, although the molecular mechanisms of functional HSCs and an increase in their proliferative and leading to transformation by HOXA9 and MEIS1 remain elusive. In repopulating capacity (19, 20). Conversely, CEBPA overexpression can promote transdifferentiation of a variety of fibroblastic cells to this study, we identify CCAAT/enhancer binding protein alpha (C/ the myeloid lineage and can induce monocytic differentiation in EBPα) as a critical collaborator required for Hoxa9/Meis1-mediated α MLL-fusion protein-mediated leukemias (21, 22). -

Appendix 2. Significantly Differentially Regulated Genes in Term Compared with Second Trimester Amniotic Fluid Supernatant
Appendix 2. Significantly Differentially Regulated Genes in Term Compared With Second Trimester Amniotic Fluid Supernatant Fold Change in term vs second trimester Amniotic Affymetrix Duplicate Fluid Probe ID probes Symbol Entrez Gene Name 1019.9 217059_at D MUC7 mucin 7, secreted 424.5 211735_x_at D SFTPC surfactant protein C 416.2 206835_at STATH statherin 363.4 214387_x_at D SFTPC surfactant protein C 295.5 205982_x_at D SFTPC surfactant protein C 288.7 1553454_at RPTN repetin solute carrier family 34 (sodium 251.3 204124_at SLC34A2 phosphate), member 2 238.9 206786_at HTN3 histatin 3 161.5 220191_at GKN1 gastrokine 1 152.7 223678_s_at D SFTPA2 surfactant protein A2 130.9 207430_s_at D MSMB microseminoprotein, beta- 99.0 214199_at SFTPD surfactant protein D major histocompatibility complex, class II, 96.5 210982_s_at D HLA-DRA DR alpha 96.5 221133_s_at D CLDN18 claudin 18 94.4 238222_at GKN2 gastrokine 2 93.7 1557961_s_at D LOC100127983 uncharacterized LOC100127983 93.1 229584_at LRRK2 leucine-rich repeat kinase 2 HOXD cluster antisense RNA 1 (non- 88.6 242042_s_at D HOXD-AS1 protein coding) 86.0 205569_at LAMP3 lysosomal-associated membrane protein 3 85.4 232698_at BPIFB2 BPI fold containing family B, member 2 84.4 205979_at SCGB2A1 secretoglobin, family 2A, member 1 84.3 230469_at RTKN2 rhotekin 2 82.2 204130_at HSD11B2 hydroxysteroid (11-beta) dehydrogenase 2 81.9 222242_s_at KLK5 kallikrein-related peptidase 5 77.0 237281_at AKAP14 A kinase (PRKA) anchor protein 14 76.7 1553602_at MUCL1 mucin-like 1 76.3 216359_at D MUC7 mucin 7, -

Supplementary Materials
Supplementary Materials + - NUMB E2F2 PCBP2 CDKN1B MTOR AKT3 HOXA9 HNRNPA1 HNRNPA2B1 HNRNPA2B1 HNRNPK HNRNPA3 PCBP2 AICDA FLT3 SLAMF1 BIC CD34 TAL1 SPI1 GATA1 CD48 PIK3CG RUNX1 PIK3CD SLAMF1 CDKN2B CDKN2A CD34 RUNX1 E2F3 KMT2A RUNX1 T MIXL1 +++ +++ ++++ ++++ +++ 0 0 0 0 hematopoietic potential H1 H1 PB7 PB6 PB6 PB6.1 PB6.1 PB12.1 PB12.1 Figure S1. Unsupervised hierarchical clustering of hPSC-derived EBs according to the mRNA expression of hematopoietic lineage genes (microarray analysis). Hematopoietic-competent cells (H1, PB6.1, PB7) were separated from hematopoietic-deficient ones (PB6, PB12.1). In this experiment, all hPSCs were tested in duplicate, except PB7. Genes under-expressed or over-expressed in blood-deficient hPSCs are indicated in blue and red respectively (related to Table S1). 1 C) Mesoderm B) Endoderm + - KDR HAND1 GATA6 MEF2C DKK1 MSX1 GATA4 WNT3A GATA4 COL2A1 HNF1B ZFPM2 A) Ectoderm GATA4 GATA4 GSC GATA4 T ISL1 NCAM1 FOXH1 NCAM1 MESP1 CER1 WNT3A MIXL1 GATA4 PAX6 CDX2 T PAX6 SOX17 HBB NES GATA6 WT1 SOX1 FN1 ACTC1 ZIC1 FOXA2 MYF5 ZIC1 CXCR4 TBX5 PAX6 NCAM1 TBX20 PAX6 KRT18 DDX4 TUBB3 EPCAM TBX5 SOX2 KRT18 NKX2-5 NES AFP COL1A1 +++ +++ 0 0 0 0 ++++ +++ ++++ +++ +++ ++++ +++ ++++ 0 0 0 0 +++ +++ ++++ +++ ++++ 0 0 0 0 hematopoietic potential H1 H1 H1 H1 H1 H1 PB6 PB6 PB7 PB7 PB6 PB6 PB7 PB6 PB6 PB6.1 PB6.1 PB6.1 PB6.1 PB6.1 PB6.1 PB12.1 PB12.1 PB12.1 PB12.1 PB12.1 PB12.1 Figure S2. Unsupervised hierarchical clustering of hPSC-derived EBs according to the mRNA expression of germ layer differentiation genes (microarray analysis) Selected ectoderm (A), endoderm (B) and mesoderm (C) related genes differentially expressed between hematopoietic-competent (H1, PB6.1, PB7) and -deficient cells (PB6, PB12.1) are shown (related to Table S1). -

Single Cell Regulatory Landscape of the Mouse Kidney Highlights Cellular Differentiation Programs and Disease Targets
ARTICLE https://doi.org/10.1038/s41467-021-22266-1 OPEN Single cell regulatory landscape of the mouse kidney highlights cellular differentiation programs and disease targets Zhen Miao 1,2,3,8, Michael S. Balzer 1,2,8, Ziyuan Ma 1,2,8, Hongbo Liu1,2, Junnan Wu 1,2, Rojesh Shrestha 1,2, Tamas Aranyi1,2, Amy Kwan4, Ayano Kondo 4, Marco Pontoglio 5, Junhyong Kim6, ✉ Mingyao Li 7, Klaus H. Kaestner2,4 & Katalin Susztak 1,2,4 1234567890():,; Determining the epigenetic program that generates unique cell types in the kidney is critical for understanding cell-type heterogeneity during tissue homeostasis and injury response. Here, we profile open chromatin and gene expression in developing and adult mouse kidneys at single cell resolution. We show critical reliance of gene expression on distal regulatory elements (enhancers). We reveal key cell type-specific transcription factors and major gene- regulatory circuits for kidney cells. Dynamic chromatin and expression changes during nephron progenitor differentiation demonstrates that podocyte commitment occurs early and is associated with sustained Foxl1 expression. Renal tubule cells follow a more complex differentiation, where Hfn4a is associated with proximal and Tfap2b with distal fate. Mapping single nucleotide variants associated with human kidney disease implicates critical cell types, developmental stages, genes, and regulatory mechanisms. The single cell multi-omics atlas reveals key chromatin remodeling events and gene expression dynamics associated with kidney development. 1 Renal, Electrolyte, and Hypertension Division, Department of Medicine, University of Pennsylvania, Perelman School of Medicine, Philadelphia, PA, USA. 2 Institute for Diabetes, Obesity, and Metabolism, University of Pennsylvania, Perelman School of Medicine, Philadelphia, PA, USA. -
A KLF4/Pihl/EZH2/HMGA2 Regulatory Axis and Its Function in Promoting
Deng et al. Cell Death and Disease (2021) 12:485 https://doi.org/10.1038/s41419-021-03753-1 Cell Death & Disease ARTICLE Open Access A KLF4/PiHL/EZH2/HMGA2 regulatory axis and its function in promoting oxaliplatin-resistance of colorectal cancer Xuan Deng1, Fanyang Kong2,SiLi3,HaoqinJiang1,LiuDong1,XiaoXu1, Xinju Zhang1,HongYuan3,YingXu4, Yimin Chu4,HaixiaPeng4 andMingGuan 1 Abstract Long noncoding RNAs (lncRNAs) have emerged as a new class of regulatory molecules implicated in therapeutic resistance, yet the mechanisms underlying lncRNA-mediated oxaliplatin resistance in colorectal cancer (CRC) are poorly understood. In this study, lncRNA P53 inHibiting LncRNA (PiHL) was shown to be highly induced in oxaliplatin- resistant CRC cells and tumor tissues. In vitro and in vivo models clarified PiHL’s role in conferring resistance to oxaliplatin-induced apoptosis. PiHL antagonized chemosensitivity through binding with EZH2, repressing location of EZH2 to HMGA2 promoter, and downregulating methylation of histone H3 lysine 27 (H3K27me3) level in HMGA2 promoter, thus activating HMGA2 expression. Furthermore, HMGA2 upregulation induced by PiHL promotes PI3K/Akt phosphorylation, which resulted in increased oxaliplatin resistance. We also found that transcription factor KLF4 was downregulated in oxaliplatin-resistant cells, and KLF4 negatively regulated PiHL expression by binding to PiHL promoter. In vivo models further demonstrated that treatment of oxaliplatin-resistant CRC with locked nucleic acids targeting PiHL restored oxaliplatin response. Collectively, this study established lncRNA PiHL as a chemoresistance 1234567890():,; 1234567890():,; 1234567890():,; 1234567890():,; promoter in CRC, and targeting PiHL/EZH2/HMGA2/PI3K/Akt signaling axis represents a novel choice in the investigation of drug resistance. Introduction eventually cause cell cycle arrest and apoptosis2. -

HOXA10 Controls Osteoblastogenesis by Directly Activating Bone Regulatory and Phenotypic Genes
University of Massachusetts Medical School eScholarship@UMMS Open Access Articles Open Access Publications by UMMS Authors 2007-02-28 HOXA10 controls osteoblastogenesis by directly activating bone regulatory and phenotypic genes Mohammad Q. Hassan University of Massachusetts Medical School Et al. Let us know how access to this document benefits ou.y Follow this and additional works at: https://escholarship.umassmed.edu/oapubs Part of the Life Sciences Commons, and the Medicine and Health Sciences Commons Repository Citation Hassan MQ, Tare RS, Lee SH, Mandeville M, Weiner B, Montecino MA, Van Wijnen AJ, Stein JL, Stein GS, Lian JB. (2007). HOXA10 controls osteoblastogenesis by directly activating bone regulatory and phenotypic genes. Open Access Articles. https://doi.org/10.1128/MCB.01544-06. Retrieved from https://escholarship.umassmed.edu/oapubs/1334 This material is brought to you by eScholarship@UMMS. It has been accepted for inclusion in Open Access Articles by an authorized administrator of eScholarship@UMMS. For more information, please contact [email protected]. MOLECULAR AND CELLULAR BIOLOGY, May 2007, p. 3337–3352 Vol. 27, No. 9 0270-7306/07/$08.00ϩ0 doi:10.1128/MCB.01544-06 Copyright © 2007, American Society for Microbiology. All Rights Reserved. HOXA10 Controls Osteoblastogenesis by Directly Activating Bone Regulatory and Phenotypic Genesᰔ Mohammad Q. Hassan,1 Rahul Tare,1† Suk Hee Lee,1 Matthew Mandeville,1 Brian Weiner,1 Martin Montecino,2 Andre J. van Wijnen,1 Janet L. Stein,1 Gary S. Stein,1 and Jane B. Lian1* Department of Cell Biology and Cancer Center, University of Massachusetts Medical School, Worcester, Massachusetts 01655,1 and Departamento de Bioquimica y Biologia Molecular, Facultad de Ciencias Biologicas, Universidad de Concepcion, Concepcion, Chile2 Received 18 August 2006/Returned for modification 4 October 2006/Accepted 9 February 2007 HOXA10 is necessary for embryonic patterning of skeletal elements, but its function in bone formation beyond this early developmental stage is unknown. -

Figure S17 Figure S16
immune responseregulatingcellsurfacereceptorsignalingpathway ventricular cardiacmuscletissuedevelopment t cellactivationinvolvedinimmuneresponse intrinsic apoptoticsignalingpathway single organismalcelladhesion cholesterol biosyntheticprocess myeloid leukocytedifferentiation determination ofadultlifespan response tointerferongamma muscle organmorphogenesis endothelial celldifferentiation brown fatcelldifferentiation mitochondrion organization myoblast differentiation response toprotozoan amino acidtransport leukocyte migration cytokine production t celldifferentiation protein secretion response tovirus angiogenesis Scrt1 Tcf25 Dpf1 Sap30 Ing2 Zfp654 Sp9 Zfp263 Mxi1 Hes6 Zfp395 Rlf Ppp1r13l Snapc1 C030039L03Rik Hif1a Arrb1 Glis3 Rcor2 Hif3a Fbxo21 Dnajc21 Rest Sirt6 Foxj1 Kdm5b Ankzf1 Sos2 Plscr1 Jdp2 Rbbp8 Etv4 Msh5 Mafg Tsc22d3 Nupr1 Ddit3 Cebpg Zfp790 Atf5 Cebpb Atf3 Trim21 Irf9 Irf2 Tbx21 Stat2 Stat1 Zbp1 Irf1 aGOslimPos Ikzf3 Oasl1 Irf7 Trim30a Dhx58 Txk Rorc Rora Nr1d2 Setdb2 Vdr Vax2 Nr1d1 Foxs1 Eno1 Thap3 Nfkbil1 Edf1 Srebf1 Lbr Tead1 Zfp608 Pcx Ift57 Ssbp4 Stat3 Mxd1 Pml Ssh2 Chd7 Maf Cic Bcl3 Prkdc Mbd5 Ppfibp2 Foxp2 Tal2 Mlf1 Bcl6b Zfp827 Ikzf2 Phtf2 Bmyc Plagl2 Nfkb2 Nfkb1 Tox Nrip1 Utf1 Klf3 Plagl1 Nfkbib Spib Nfkbie Akna Rbpj Ncoa3 Id1 Tnp2 Gata3 Gata1 Pparg Id2 Epas1 Zfp280b Commons Pathway Erg GO MSigDB KEGG Hhex WikiPathways SetGene Databases Batf Aff3 Zfp266 gene modules other (hypergeometric TF, from Figure Trim24 Zbtb5 Foxo3 Aebp2 XPodNet -protein-proteininteractionsinthepodocyteexpandedbySTRING Ppp1r10 Dffb Trp53 Enrichment -
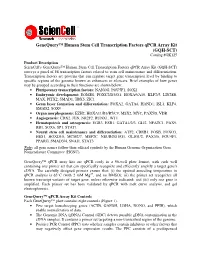
Genequery™ Human Stem Cell Transcription Factors Qpcr Array
GeneQuery™ Human Stem Cell Transcription Factors qPCR Array Kit (GQH-SCT) Catalog #GK125 Product Description ScienCell's GeneQuery™ Human Stem Cell Transcription Factors qPCR Array Kit (GQH-SCT) surveys a panel of 88 transcription factors related to stem cell maintenance and differentiation. Transcription factors are proteins that can regulate target gene transcription level by binding to specific regions of the genome known as enhancers or silencers. Brief examples of how genes may be grouped according to their functions are shown below: • Pluripotency transcription factors: NANOG, POU5F1, SOX2 • Embryonic development: EOMES, FOXC2/D3/O1, HOXA9/A10, KLF2/5, LIN28B, MAX, PITX2, SMAD1, TBX5, ZIC1 • Germ layer formation and differentiation: FOXA2, GATA6, HAND1, ISL1, KLF4, SMAD2, SOX9 • Organ morphogenesis: EZH2, HOXA11/B3/B5/C9, MSX2, MYC, PAX5/8, VDR • Angiogenesis: CDX2, JUN, NR2F2, RUNX1, WT1 • Hematopoiesis and osteogenesis: EGR3, ESR1, GATA1/2/3, GLI2, NFATC1, PAX9, RB1, SOX6, SP1, STAT1 • Neural stem cell maintenance and differentiation: ATF2, CREB1, FOSB, FOXO3, HES1, HOXD10, MCM2/7, MEF2C, NEUROD1/G1, OLIG1/2, PAX3/6, POU4F1, PPARG, SMAD3/4, SNAI1, STAT3 Note : all gene names follow their official symbols by the Human Genome Organization Gene Nomenclature Committee (HGNC). GeneQuery™ qPCR array kits are qPCR ready in a 96-well plate format, with each well containing one primer set that can specifically recognize and efficiently amplify a target gene's cDNA. The carefully designed primers ensure that: (i) the optimal annealing temperature in qPCR analysis is 65°C (with 2 mM Mg 2+ , and no DMSO); (ii) the primer set recognizes all known transcript variants of target gene, unless otherwise indicated; and (iii) only one gene is amplified.