4671.Full.Pdf
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Human and Mouse CD Marker Handbook Human and Mouse CD Marker Key Markers - Human Key Markers - Mouse
Welcome to More Choice CD Marker Handbook For more information, please visit: Human bdbiosciences.com/eu/go/humancdmarkers Mouse bdbiosciences.com/eu/go/mousecdmarkers Human and Mouse CD Marker Handbook Human and Mouse CD Marker Key Markers - Human Key Markers - Mouse CD3 CD3 CD (cluster of differentiation) molecules are cell surface markers T Cell CD4 CD4 useful for the identification and characterization of leukocytes. The CD CD8 CD8 nomenclature was developed and is maintained through the HLDA (Human Leukocyte Differentiation Antigens) workshop started in 1982. CD45R/B220 CD19 CD19 The goal is to provide standardization of monoclonal antibodies to B Cell CD20 CD22 (B cell activation marker) human antigens across laboratories. To characterize or “workshop” the antibodies, multiple laboratories carry out blind analyses of antibodies. These results independently validate antibody specificity. CD11c CD11c Dendritic Cell CD123 CD123 While the CD nomenclature has been developed for use with human antigens, it is applied to corresponding mouse antigens as well as antigens from other species. However, the mouse and other species NK Cell CD56 CD335 (NKp46) antibodies are not tested by HLDA. Human CD markers were reviewed by the HLDA. New CD markers Stem Cell/ CD34 CD34 were established at the HLDA9 meeting held in Barcelona in 2010. For Precursor hematopoetic stem cell only hematopoetic stem cell only additional information and CD markers please visit www.hcdm.org. Macrophage/ CD14 CD11b/ Mac-1 Monocyte CD33 Ly-71 (F4/80) CD66b Granulocyte CD66b Gr-1/Ly6G Ly6C CD41 CD41 CD61 (Integrin b3) CD61 Platelet CD9 CD62 CD62P (activated platelets) CD235a CD235a Erythrocyte Ter-119 CD146 MECA-32 CD106 CD146 Endothelial Cell CD31 CD62E (activated endothelial cells) Epithelial Cell CD236 CD326 (EPCAM1) For Research Use Only. -

Characterization of FLT3-Itdmut Acute Myeloid Leukemia
Travaglini et al. Blood Cancer Journal (2020) 10:85 https://doi.org/10.1038/s41408-020-00352-9 Blood Cancer Journal ARTICLE Open Access Characterization of FLT3-ITDmut acute myeloid leukemia: molecular profiling of leukemic precursor cells Serena Travaglini1, Daniela Francesca Angelini 2, Valentina Alfonso1, Gisella Guerrera2,SerenaLavorgna1, Mariadomenica Divona1, Anna Maria Nardozza1, Maria Irno Consalvo1, Emiliano Fabiani1,MarcoDeBardi 2, Benedetta Neri3,FabioForghieri4, Francesco Marchesi5, Giovangiacinto Paterno1, Raffaella Cerretti1, Eva Barragan 6, Valentina Fiori7,SabrinaDominici7, Maria Ilaria Del Principe1, Adriano Venditti 1, Luca Battistini2, William Arcese1, Francesco Lo-Coco1, Maria Teresa Voso 1,2 and Tiziana Ottone1,2 Abstract Acute myeloid leukemia (AML) with FLT3-ITD mutations (FLT3-ITDmut) remains a therapeutic challenge, with a still high relapse rate, despite targeted treatment with tyrosine kinase inhibitors. In this disease, the CD34/CD123/CD25/CD99+ leukemic precursor cells (LPCs) phenotype predicts for FLT3-ITD-positivity. The aim of this study was to characterize the distribution of FLT3-ITD mutation in different progenitor cell subsets to shed light on the subclonal architecture of FLT3-ITDmut AML. Using high-speed cell sorting, we sequentially purified LPCs and CD34+ progenitors in samples from patients with FLT3-ITDmut AML (n = 12). A higher FLT3-ITDmut load was observed within CD34/CD123/CD25/CD99+ LPCs, as compared to CD34+ progenitors (CD123+/−,CD25−,CD99low/−)(p = 0.0005) and mononuclear cells (MNCs) (p < 0.0001). This was associated with significantly increased CD99 mean fluorescence intensity in LPCs. 1234567890():,; 1234567890():,; 1234567890():,; 1234567890():,; Significantly higher FLT3-ITDmut burden was also observed in LPCs of AML patients with a small FLT3-ITDmut clones at diagnosis. -

Single-Cell RNA Sequencing Demonstrates the Molecular and Cellular Reprogramming of Metastatic Lung Adenocarcinoma
ARTICLE https://doi.org/10.1038/s41467-020-16164-1 OPEN Single-cell RNA sequencing demonstrates the molecular and cellular reprogramming of metastatic lung adenocarcinoma Nayoung Kim 1,2,3,13, Hong Kwan Kim4,13, Kyungjong Lee 5,13, Yourae Hong 1,6, Jong Ho Cho4, Jung Won Choi7, Jung-Il Lee7, Yeon-Lim Suh8,BoMiKu9, Hye Hyeon Eum 1,2,3, Soyean Choi 1, Yoon-La Choi6,10,11, Je-Gun Joung1, Woong-Yang Park 1,2,6, Hyun Ae Jung12, Jong-Mu Sun12, Se-Hoon Lee12, ✉ ✉ Jin Seok Ahn12, Keunchil Park12, Myung-Ju Ahn 12 & Hae-Ock Lee 1,2,3,6 1234567890():,; Advanced metastatic cancer poses utmost clinical challenges and may present molecular and cellular features distinct from an early-stage cancer. Herein, we present single-cell tran- scriptome profiling of metastatic lung adenocarcinoma, the most prevalent histological lung cancer type diagnosed at stage IV in over 40% of all cases. From 208,506 cells populating the normal tissues or early to metastatic stage cancer in 44 patients, we identify a cancer cell subtype deviating from the normal differentiation trajectory and dominating the metastatic stage. In all stages, the stromal and immune cell dynamics reveal ontological and functional changes that create a pro-tumoral and immunosuppressive microenvironment. Normal resident myeloid cell populations are gradually replaced with monocyte-derived macrophages and dendritic cells, along with T-cell exhaustion. This extensive single-cell analysis enhances our understanding of molecular and cellular dynamics in metastatic lung cancer and reveals potential diagnostic and therapeutic targets in cancer-microenvironment interactions. 1 Samsung Genome Institute, Samsung Medical Center, Seoul 06351, Korea. -

CD29 Identifies IFN-Γ–Producing Human CD8+ T Cells With
+ CD29 identifies IFN-γ–producing human CD8 T cells with an increased cytotoxic potential Benoît P. Nicoleta,b, Aurélie Guislaina,b, Floris P. J. van Alphenc, Raquel Gomez-Eerlandd, Ton N. M. Schumacherd, Maartje van den Biggelaarc,e, and Monika C. Wolkersa,b,1 aDepartment of Hematopoiesis, Sanquin Research, 1066 CX Amsterdam, The Netherlands; bLandsteiner Laboratory, Oncode Institute, Amsterdam University Medical Center, University of Amsterdam, 1105 AZ Amsterdam, The Netherlands; cDepartment of Research Facilities, Sanquin Research, 1066 CX Amsterdam, The Netherlands; dDivision of Molecular Oncology and Immunology, Oncode Institute, The Netherlands Cancer Institute, 1066 CX Amsterdam, The Netherlands; and eDepartment of Molecular and Cellular Haemostasis, Sanquin Research, 1066 CX Amsterdam, The Netherlands Edited by Anjana Rao, La Jolla Institute for Allergy and Immunology, La Jolla, CA, and approved February 12, 2020 (received for review August 12, 2019) Cytotoxic CD8+ T cells can effectively kill target cells by producing therefore developed a protocol that allowed for efficient iso- cytokines, chemokines, and granzymes. Expression of these effector lation of RNA and protein from fluorescence-activated cell molecules is however highly divergent, and tools that identify and sorting (FACS)-sorted fixed T cells after intracellular cytokine + preselect CD8 T cells with a cytotoxic expression profile are lacking. staining. With this top-down approach, we performed an un- + Human CD8 T cells can be divided into IFN-γ– and IL-2–producing biased RNA-sequencing (RNA-seq) and mass spectrometry cells. Unbiased transcriptomics and proteomics analysis on cytokine- γ– – + + (MS) analyses on IFN- and IL-2 producing primary human producing fixed CD8 T cells revealed that IL-2 cells produce helper + + + CD8 Tcells. -

Blood Flow Guides Sequential Support of Neutrophil Arrest and Diapedesis
RESEARCH ARTICLE Blood flow guides sequential support of neutrophil arrest and diapedesis by PILR-b 1 and PILR-a Yu-Tung Li, Debashree Goswami†, Melissa Follmer, Annette Artz, Mariana Pacheco-Blanco, Dietmar Vestweber* Vascular Cell Biology, Max Planck Institute of Molecular Biomedicine, Mu¨ nster, Germany Abstract Arrest of rapidly flowing neutrophils in venules relies on capturing through selectins and chemokine-induced integrin activation. Despite a long-established concept, we show here that gene inactivation of activating paired immunoglobulin-like receptor (PILR)-b1 nearly halved the efficiency of neutrophil arrest in venules of the mouse cremaster muscle. We found that this receptor binds to CD99, an interaction which relies on flow-induced shear forces and boosts chemokine-induced b2-integrin-activation, leading to neutrophil attachment to endothelium. Upon arrest, binding of PILR-b1 to CD99 ceases, shifting the signaling balance towards inhibitory PILR-a. This enables integrin deactivation and supports cell migration. Thus, flow-driven shear forces guide sequential signaling of first activating PILR-b1 followed by inhibitory PILR-a to prompt neutrophil arrest and then transmigration. This doubles the efficiency of selectin-chemokine driven neutrophil arrest by PILR-b1 and then supports transition to migration by PILR-a. DOI: https://doi.org/10.7554/eLife.47642.001 *For correspondence: [email protected] Present address: †Center for Global Infectious Disease Introduction Research, Seattle Childrens Host defense against pathogens depends on the recruitment of leukocytes to sites of infections Research Institute, Seattle, (Ley et al., 2007). Selectins capture leukocytes to the endothelial cell surface by binding to glyco- United States conjugates (McEver, 2015). -
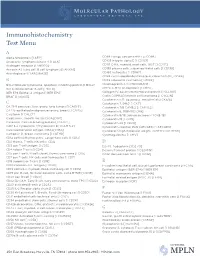
IHC Test Menu
Immunohistochemistry Test Menu A Alpha fetoprotein [I AFP] CD99 Ewings sarcoma PNET [I CD99] Anaplastic lymphoma kinase -1 [I ALK] CD103 Integrin alpha E [I CD103] Androgen receptor [I ANDRO]* CD117 C-Kit, myeloid, mast cells, GIST [I CD117] Annexin A1, hairy cell, B cell lymphoma [I ANXA1] CD138 plasma cells, subset epithelial cells [I CD138] Anti-Arginase-1 [I ARGINASE] CD163 histiocytes [I CD163] CDK4 cyclin-depdendent kinase-4, clone DCS-31 [I CDK4] B CDX2 colorectal carcinoma [I CDX2] BCL2 follicular lymphoma, apoptosis inhibiting protein [I BCL2] Chromogranin A [I CHROGRAN] BCL6 follicle center B-cell [I BCL6] CMYC C-MYC oncoprotein [I CMYC] BER EP4 Epithelial antigen [I BER EP4] Collagen IV, basement membrane protein [I CLLGIV] BRAF [I V600E] Cyclin D1/PRAD1 mantle cell lymphoma [I CYCLIN] Cytokeratin 5/6, squamous, mesothelial [I CK5/6] C Cytokeratin 7, 54kD [I CK7] CA 19-9 pancreas, liver, ovary, lung tumors [I CA19 9] Cytokeratin 7/8 CAM5.2 [I CAM 5.2] CA 125 epitheliod malignancies ovary, breast [I CA125] Cytokeratin 8, 35BH11 [I CK8] Calcitonin [I CALCT] Cytokeratin 8/18, adenocarcinoma [I CK8/18] Caldesmon, smooth muscle [I CALDSM] Cytokeratin 19 [I CK19] Calretinin; Calcium binding protein [I CALRT] Cytokeratin 20 [I CK20] CAM 5.2 Cytokeratin 7/Cytokeratin 8 [I CAM 5.2] Cytokeratin cocktail, PAN (AE1/AE3) [I AE1/AE3] Carcinoembryonic antigen (CEA) [I CEA] Cytokeratin high molecular weight; 34BE12 [I CK HMW] Cathepsin D, breast carcinoma [I CATHD] Cytomegalovirus [I CMV] CD1a cortical thymocyctes, Langerhans cells [I CD1a] -

WO 2018/067991 Al 12 April 2018 (12.04.2018) W !P O PCT
(12) INTERNATIONAL APPLICATION PUBLISHED UNDER THE PATENT COOPERATION TREATY (PCT) (19) World Intellectual Property Organization International Bureau (10) International Publication Number (43) International Publication Date WO 2018/067991 Al 12 April 2018 (12.04.2018) W !P O PCT (51) International Patent Classification: achusetts 021 15 (US). THE BROAD INSTITUTE, A61K 51/10 (2006.01) G01N 33/574 (2006.01) INC. [US/US]; 415 Main Street, Cambridge, Massachu C07K 14/705 (2006.01) A61K 47/68 (2017.01) setts 02142 (US). MASSACHUSETTS INSTITUTE OF G01N 33/53 (2006.01) TECHNOLOGY [US/US]; 77 Massachusetts Avenue, Cambridge, Massachusetts 02139 (US). (21) International Application Number: PCT/US2017/055625 (72) Inventors; and (71) Applicants: KUCHROO, Vijay K. [IN/US]; 30 Fairhaven (22) International Filing Date: Road, Newton, Massachusetts 02149 (US). ANDERSON, 06 October 2017 (06.10.2017) Ana Carrizosa [US/US]; 110 Cypress Street, Brookline, (25) Filing Language: English Massachusetts 02445 (US). MADI, Asaf [US/US]; c/o The Brigham and Women's Hospital, Inc., 75 Francis (26) Publication Language: English Street, Boston, Massachusetts 021 15 (US). CHIHARA, (30) Priority Data: Norio [US/US]; c/o The Brigham and Women's Hospital, 62/405,835 07 October 2016 (07.10.2016) US Inc., 75 Francis Street, Boston, Massachusetts 021 15 (US). REGEV, Aviv [US/US]; 15a Ellsworth Ave, Cambridge, (71) Applicants: THE BRIGHAM AND WOMEN'S HOSPI¬ Massachusetts 02139 (US). SINGER, Meromit [US/US]; TAL, INC. [US/US]; 75 Francis Street, Boston, Mass c/o The Broad Institute, Inc., 415 Main Street, Cambridge, (54) Title: MODULATION OF NOVEL IMMUNE CHECKPOINT TARGETS CD4 FIG. -

Immunohistochemistry Stain Offerings
immunohistochemistry stain offerings TRUSTED PATHOLOGISTS. INVALUABLE ANSWERS.™ MARCHMAY 20172021 www.aruplab.com/ap-ihcaruplab.com/ap-ihc InformationInformation in this brochurein this brochure is current is current as of as May of March 2021. 2017. All content All content is subject is subject to tochange. change. Please contactPlease ARUPcontact ClientARUP Services Client Services at 800-522-2787 at (800) 522-2787 with any with questions any questions or concerns.or concerns. ARUP LABORATORIES As a nonprofit, academic institution of the University of Utah and its Department We believe in of Pathology, ARUP believes in collaborating, sharing and contributing to laboratory science in ways that benefit our clients and their patients. collaborating, Our test menu is one of the broadest in the industry, encompassing more sharing and than 3,000 tests, including highly specialized and esoteric assays. We offer comprehensive testing in the areas of genetics, molecular oncology, pediatrics, contributing pain management, and more. to laboratory ARUP’s clients include many of the nation’s university teaching hospitals and children’s hospitals, as well as multihospital groups, major commercial science in ways laboratories, and group purchasing organizations. We believe that healthcare should be delivered as close to the patient as possible, which is why we support that provide our clients’ efforts to be the principal healthcare provider in the communities they serve by offering highly complex assays and accompanying consultative support. the best value Offering analytics, consulting, and decision support services, ARUP provides for the patient. clients with the utilization management tools necessary to prosper in this time of value-based care. -

Diagnostic Accuracy of a Panel of Immunohistochemical and Molecular Markers to Distinguish Merkel Cell Carcinoma from Other Neuroendocrine Carcinomas
Modern Pathology (2019) 32:499–510 https://doi.org/10.1038/s41379-018-0155-y ARTICLE Diagnostic accuracy of a panel of immunohistochemical and molecular markers to distinguish Merkel cell carcinoma from other neuroendocrine carcinomas 1,2,3 4 1 3 3 Thibault Kervarrec ● Anne Tallet ● Elodie Miquelestorena-Standley ● Roland Houben ● David Schrama ● 5 2 6 7 8 Thilo Gambichler ● Patricia Berthon ● Yannick Le Corre ● Ewa Hainaut-Wierzbicka ● Francois Aubin ● 9 10 11 12 12 Guido Bens ● Flore Tabareau-Delalande ● Nathalie Beneton ● Gaëlle Fromont ● Flavie Arbion ● 13 2 2,14 1,2 Emmanuelle Leteurtre ● Antoine Touzé ● Mahtab Samimi ● Serge Guyétant Received: 14 July 2018 / Revised: 2 September 2018 / Accepted: 3 September 2018 / Published online: 22 October 2018 © United States & Canadian Academy of Pathology 2018 Abstract Merkel cell carcinoma is a rare neuroendocrine carcinoma of the skin mostly induced by Merkel cell polyomavirus integration. Cytokeratin 20 (CK20) positivity is currently used to distinguish Merkel cell carcinomas from other neuroendocrine carcinomas. However, this distinction may be challenging in CK20-negative cases and in cases without a 1234567890();,: 1234567890();,: primary skin tumor. The objectives of this study were first to evaluate the diagnostic accuracy of previously described markers for the diagnosis of Merkel cell carcinoma and second to validate these markers in the setting of difficult-to- diagnose Merkel cell carcinoma variants. In a preliminary set (n = 30), we assessed optimal immunohistochemical patterns (CK20, thyroid transcription factor 1 [TTF-1], atonal homolog 1 [ATOH1], neurofilament [NF], special AT-rich sequence- binding protein 2 [SATB2], paired box protein 5, terminal desoxynucleotidyl transferase, CD99, mucin 1, and Merkel cell polyomavirus-large T antigen) and Merkel cell polyomavirus load thresholds (real-time PCR). -

Death CD99 Signals Caspase-Independent T Cell
CD99 Signals Caspase-Independent T Cell Death Rolf D. Pettersen, Ghislaine Bernard, Mette Kløvstad Olafsen, Monique Pourtein and Sverre O. Lie This information is current as of September 24, 2021. J Immunol 2001; 166:4931-4942; ; doi: 10.4049/jimmunol.166.8.4931 http://www.jimmunol.org/content/166/8/4931 Downloaded from References This article cites 90 articles, 52 of which you can access for free at: http://www.jimmunol.org/content/166/8/4931.full#ref-list-1 Why The JI? Submit online. http://www.jimmunol.org/ • Rapid Reviews! 30 days* from submission to initial decision • No Triage! Every submission reviewed by practicing scientists • Fast Publication! 4 weeks from acceptance to publication *average by guest on September 24, 2021 Subscription Information about subscribing to The Journal of Immunology is online at: http://jimmunol.org/subscription Permissions Submit copyright permission requests at: http://www.aai.org/About/Publications/JI/copyright.html Email Alerts Receive free email-alerts when new articles cite this article. Sign up at: http://jimmunol.org/alerts The Journal of Immunology is published twice each month by The American Association of Immunologists, Inc., 1451 Rockville Pike, Suite 650, Rockville, MD 20852 Copyright © 2001 by The American Association of Immunologists All rights reserved. Print ISSN: 0022-1767 Online ISSN: 1550-6606. CD99 Signals Caspase-Independent T Cell Death1 Rolf D. Pettersen,2* Ghislaine Bernard,‡ Mette Kløvstad Olafsen,* Monique Pourtein,‡ and Sverre O. Lie† Death signaling by Fas and TNF receptors plays a major role in the control of activated mature T cells. However, the nature of the death receptors, which may be used by the immune system to control T cells that have not acquired susceptibility to Fas ligand or TNF, is not established. -

A Leukemia-Associated CD34/CD123/CD25/CD99-Positive Immunophenotype Identifies FLT3-Mutated Clones in Acute Myeloid Leukemia
Author Manuscript Published OnlineFirst on May 8, 2015; DOI: 10.1158/1078-0432.CCR-14-3186 Author manuscripts have been peer reviewed and accepted for publication but have not yet been edited. A Leukemia-Associated CD34/CD123/CD25/CD99-positive Immunophenotype Identifies FLT3-mutated Clones in Acute Myeloid Leukemia Daniela F. Angelini1*, Tiziana Ottone,2-3* Gisella Guerrera,1 Serena Lavorgna,2-3 Michela Cittadini,2-3 Francesco Buccisano,2 Marco De Bardi,1 Francesca Gargano,1 Luca Maurillo,2 Mariadomenica Divona,2 Nélida I. Noguera,3-4 Maria Irno Consalvo2, Giovanna Borsellino,1 Giorgio Bernardi,5 Sergio Amadori,2 Adriano Venditti,2 Luca Battistini,1 and Francesco Lo-Coco 2-3 1 Neuroimmunology and Flow Cytometry Units, Fondazione Santa Lucia-I.R.C.C.S., Rome, Italy. 2 Department of Biomedicine and Prevention, University of Tor Vergata, Rome, Italy. 3 Laboratorio di Neuro-Oncoematologia, Fondazione Santa Lucia I.R.C.C.S, Rome, Italy. 4 Department of Chemical Biochemistry (Hematology), National University of Rosario, Argentina. 5 Experimental Neuroscience, Fondazione Santa Lucia, I.R.C.C.S., 00179 Rome,Italy. *D.F.A. and T.O. Contributed equally to this study Running title: Immunophenotype of FLT3-ITD mutated cells Keywords: Acute Myeloid Leukemia, Multiparametric Flow Cytometry, FLT3-ITD, Leukemia Associated Immunophenotype, Minimal Residual Disease, Financial support: This study was partially supported by the Associazione Italiana per la Ricerca sul Cancro (IG 11586) to F.L.C. and Associazione Italiana contro le Leucemie (AIL). Corresponder author: Francesco Lo-Coco, M.D. Department of Biomedicine and Prevention, University Tor Vergata, Via Montpellier 1, 00133 Rome, Italy [email protected] Conflict of interest: The authors declare no conflict of interest Word count: 3933 Total number of figure: 6 1 Downloaded from clincancerres.aacrjournals.org on September 27, 2021. -

Immunoreactivity of CD99 in Non-Hodgkin's Lymphoma
CORE Metadata, citation and similar papers at core.ac.uk Provided by PubMed Central J Korean Med Sci 2005; 20: 952-6 Copyright � The Korean Academy ISSN 1011-8934 of Medical Sciences Immunoreactivity of CD99 in Non-Hodgkin’s Lymphoma : Unexpected Frequent Expression in ALK-positive Anaplastic Large Cell Lymphoma To verify the spectrum of CD99-expressing lymphoid malignancy, an immunohisto- Chang Ohk Sung, Young H. Ko, chemical study for CD99 was carried out in 182 cases of non-Hodgkin's lymphoma, Sanghui Park, Kihyun Kim*, including 21 lymphoblastic lymphomas, 11 small lymphocytic lymphomas, 9 mantle Wonseog Kim* cell lymphomas, 12 follicular lymphomas, 37 diffuse large B cell lymphomas, 18 Departments of Pathology and Hematooncology*, Burkitt's lymphomas, 28 NK/T-cell lymphomas, 8 angioimmunoblastic T-cell lym- Samsung Medical Center, Sungkyunkwan University phomas, 23 peripheral T-cell lymphomas, unspecified, and 15 systemic anaplastic School of Medicine, Seoul, Korea large cell lymphomas. CD99 was positive in all T-lymphoblastic lymphomas and in 60% of B-lymphoblastic lymphomas. Majority of T and NK cell lymphomas were negative for CD99, except anaplastic large cell lymphomas (ALCLs). Eight of 15 Received : 28 February 2005 cases (54%) of ALCLs reacted with anti CD99 antibody. Seven of 10 (70%) ALK Accepted : 24 June 2005 positive ALCLs expressed CD99, whereas only 1 of 5 (20%) ALK negative ALCLs were positive. Of the mature B-cell lymphomas, 5.4% (2/37) of diffuse large B cell lymphomas and 11.1% (2/18) of Burkitt's lymphomas expressed CD99. In conclu- Address for correspondence sion, CD99 is infrequently expressed in mature B and T cell lymphomas, except Young-Hyeh Ko, M.D.