Innovation & Patient-Centered Care
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-
2017 Match Day Results by Program
Class of 2017 Match Results Anesthesiology New York Presbyterian Hospital-Columbia University Medical Center University of Illinois College of Medicine-Chicago University of Texas Medical School-Houston Icahn School of Medicine/St Luke's-Roosevelt Hospital Center (New York) University of Florida College of Medicine-Shands Hospital New York Presbyterian Hospital-Weill Cornell Medical Center Einstein/Montefiore Medical Center (New York) New York Presbyterian Hospital-Columbia University Medical Center Dermatology University at Buffalo School of Medicine (New York) University of Buffalo School of Medicine (New York) Cleveland Clinic Foundation (OH) Emergency Medicine Einstein/Montefiore Medical Center (New York) University of Massachusetts Medical School Staten Island University Hospital (New York) Stanford University Programs (California) Stony Brook Teaching Hospitals (New York) New York Hospital Medical Center Queens (New York) Eastern Virginia Medical School University of Washington Affiliated Hospitals Icahn School of Medicine/St Luke's-Roosevelt Hospital Center (New York) University of Connecticut School of Medicine Rhode Island Hospital/Brown University Wake Forest Baptist Medical Center (North Carolina) Icahn School of Medicine/St Luke's-Roosevelt Hospital Center (New York) Einstein/Montefiore Medical Center (New York) Oregon Health and Science University Dartmouth-Hitchcock Medical Center (New Hampshire) Einstein/Montefiore Medical Center (New York) University of Washington Affiliated Hospitals Einstein/Montefiore Medical Center -

2019 Community Health Needs Assessment Survey
COMMUNITY HEALTH NEEDS ASSESSMENT 2019 To all New Yorkers: As New York City’s public health care system, our goal is to empower you to live your healthiest life. Clinical care starts with you and your health care team, but we recognize that many factors impact your health beyond medical care alone – a safe home environment, space to be physically active, access to fresh food, even exposure to daily stress and poor social well-being can impact your health outcomes. To assess and prioritize the greatest health needs of the neighborhoods and communities we serve, NYC Health + Hospitals conducted a comprehensive and inclusive process to complete this Community Health Needs Assessment for 2019. The findings represent the voices of the patients we serve, clinical experts and community partners, and are backed by quantitative data analysis. Recognizing that the health needs of patients coming through our hospital doors may not represent the wider health needs of the community, we embarked on an extensive stakeholder engagement process led by OneCity Health, who built new relationships with community stakeholders through the Delivery System Reform Incentive Payment (DSRIP) program. For the first time, we conducted a system-wide assessment to identify priorities that need to be addressed city-wide and will allow us to maximize our resources in response. We believe that we should reliably deliver high-quality services and that patients should have a consistent experience at our facilities. Since our 2016 assessment, we have worked tirelessly to address significant health needs of the community and to make it easier for our patients to access our services: • We opened and renovated dozens of community-based health centers to expand access to primary and preventive care. -

Skinny and 119 Pounds, but with the Health Hallmarks of Obesity - the New York Times 7/22/16, 2:42 PM
Skinny and 119 Pounds, but With the Health Hallmarks of Obesity - The New York Times 7/22/16, 2:42 PM http://nyti.ms/2aeHHnQ Skinny and 119 Pounds, but With the Health Hallmarks of Obesity A small group of thin patients who develop disorders typically tied to obesity pose a medical mystery and a potential opportunity for scientists. By GINA KOLATA JULY 22, 2016 Claire Walker Johnson of Queens was a medical mystery. No matter how much she ate, she never gained weight. And yet Ms. Johnson, with a long narrow face, had the conditions many obese people develop — Type 2 diabetes, high blood pressure, high cholesterol and, most strikingly, a liver buried in fat. She and a very small group of very thin people like her have given scientists surprising clues to one of the most important questions about obesity: Why do fat people often develop serious and sometimes life-threatening medical conditions? The answer, it turns out, has little to do with the fat itself. It’s about each person’s ability to store it. With that understanding, scientists are now working on drug treatments to protect people from excess unstored fat and spare them from dire medical conditions. The need is clear. One in three Americans and one in four adults worldwide have at least three conditions associated with obesity such as diabetes, high cholesterol and high blood pressure — a combination of disorders that doubles their risk of heart attacks and strokes. In addition, 2 percent to 3 percent of adults http://www.nytimes.com/2016/07/26/health/skinny-fat.html?_r=0 Page 1 of 7 Skinny and 119 Pounds, but With the Health Hallmarks of Obesity - The New York Times 7/22/16, 2:42 PM in America, or at least five million people, have a grave accumulation of fat in their livers caused by obesity that can lead to liver failure. -
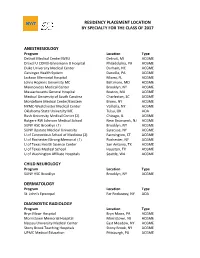
Residency Placement Location by Specialty for the Class of 2017
RESIDENCY PLACEMENT LOCATION BY SPECIALTY FOR THE CLASS OF 2017 ANESTHESIOLOGY Program Location Type Detroit Medical Center/WSU Detroit, MI ACGME Drexel U COM/Hahnemann U Hospital Philadelphia, PA ACGME Duke University Medical Center Durham, NC ACGME Geisinger Health System Danville, PA ACGME Jackson Memorial Hospital Miami, FL ACGME Johns Hopkins University MC Baltimore, MD ACGME Maimonides Medical Center Brooklyn, NY ACGME Massachusetts General Hospital Boston, MA ACGME Medical University of South Carolina Charleston, SC ACGME Montefiore Medical Center/Einstein Bronx, NY ACGME NYMC-Westchester Medical Center Valhalla, NY ACGME Oklahoma State University MC Tulsa, OK AOA Rush University Medical Center (2) Chicago, IL ACGME Rutgers-RW Johnson Medical School New Brunswick, NJ ACGME SUNY HSC Brooklyn (3) Brooklyn, NY ACGME SUNY Upstate Medical University Syracuse, NY ACGME U of Connecticut School of Medicine (2) Farmington, CT ACGME U of Rochester/Strong Memorial (3) Rochester, NY ACGME U of Texas Health Science Center San Antonio, TX ACGME U of Texas Medical School Houston, TX ACGME U of Washington Affiliate Hospitals Seattle, WA ACGME CHILD NEUROLOGY Program Location Type SUNY HSC Brooklyn Brooklyn, NY ACGME DERMATOLOGY Program Location Type St. John’s Episcopal Far Rockaway, NY AOA DIAGNOSTIC RADIOLOGY Program Location Type Bryn Mawr Hospital Bryn Mawr, PA ACGME Morristown Memorial Hospital Morristown, NJ ACGME Nassau University Medical Center East Meadow, NY ACGME Stony Brook Teaching Hospitals Stony Brook, NY ACGME UPMC Medical Education -

Cornell University Official Publication
CORNELL UNIVERSITY OFFICIAL PUBLICATION Volume XXVIII Number I Announcement of The Medical College for 1936-37 at 1300 York Avenue, New York City and the first year, also, at Ithaca, N. Y. Ithaca, New York Published by the University July 1, 1936 Printed by W. F. Humphrey Press Inc. Geneva, N. Y. CONTENTS PAGE Calendar _ 5 Board of Trustees . 6 New York Hospital-Cornell Medical College Association . 7 Medical College Council . 7 Officers of Administration . .8 and . Executive Faculty Committees of the Faculty . 9 and Faculty Teaching Staff. 10 New York Hospital Staff . 27 Bellevue Hospital, Staff of Second Division . 38 Memorial Hospital Staff 40 General Statement . 43 Requirements for Admission .... 48 Admission to Advanced Standing . 49 Requirements for Promotion and Graduation ......50 General Information:. .52 Fees, Scholarships, Loans, Prizes. 52 Educational Policy and Description of Courses: . 56 Summary of Hours in Medical Course . 58 Anatomy .... 59 Applied Pathology and Bacteriology . 67 Bacteriology 64 Biochemistry . 62 Legal Medicine 83 Medicine and Medical Specialties. 67 72 Obstetrics and Gynecology 64 Pathology . Pediatrics 74 Pharmacology 66 Physiology 63 Psychiatry. 75 81 Public Health and Preventive Medicine 3 PAGE and Surgery Surgical Specialties ... 77 . ... 82 Radiology . Schedule of Courses . ..... 84 Special Students . .....88 The Graduate School . .... 89 The Ithaca Division: of 91 Faculty Medicine at Ithaca . 92 University Calendar . 92 General Statement . Plan of Instruction 94 Anatomy . 94 Histology and Embryology 96 Physiology and Biochemistry . 97 Summarized Statement . ... 99 General Information . 100 Schedule of Instruction . 102 Combined A.B. and M.D. Degrees . 102 Graduate Work at Ithaca .... 104 Internship Appointments ..... ... 106 Register of Students, 1936-1937 . -

Wendy Chung: Genetic Sleuth Is Advocate for Families
Spectrum | Autism Research News https://www.spectrumnews.org PROFILES Wendy Chung: Genetic sleuth is advocate for families BY DEBORAH RUDACILLE 21 JULY 2011 Triple threat: Colleagues say that Wendy Chung combines strengths in teaching, research and patient care with a finely tuned ethical sensibility. A few months ago, a young woman walked into Wendy Chung's office with a notebook and a flash drive. She said, "Here's my medical history, here's my genome, now you figure out what caused all this." This is exactly the kind of challenge that Chung relishes. A skilled genetic detective, she is adept at tracing an individual's symptoms to a particular genetic anomaly, teasing out its molecular ramifications and identifying the associated syndrome. According to those who know her well, that analytical bent is accompanied by a rare sensitivity. "I've known a lot of brilliant doctors and though she's at the top of the brilliance list, she also has a humanistic philosophy that animates everything she does," says Hamilton Cain, the father of one of Chung's patients. "She's not only thinking on all cylinders, but also feeling on all cylinders. She really connects with patients and their stories and their lives." Chung, who began her research career studying diabetes and obesity, is director of the clinical 1 / 4 Spectrum | Autism Research News https://www.spectrumnews.org genetics program at Columbia University Medical Center in New York as well as the university's fellowship program in clinical and molecular genetics. Two years ago, she moved into the autism field, accepting an invitation to serve as the principal investigator of the Simons Variation in Individuals Project (VIP), launched by the Simons Foundation, SFARI.org's parent organization. -

Storm Over Gender Gap Moves Into a Gray Area
وزارة اﻟﺗرﺑﯾﺔ واﻟﺗﻌﻠﯾم اﻟﻌﺎﻟﻲ اﻣﺗﺣﺎﻧﺎت ﺷﮭﺎدة اﻟﺛﺎﻧوﯾﺔ اﻟﻌﺎﻣﺔ دورة ﺳﻨﺔ ۲۰۰٥ اﻟﻌﺎدﯾﺔ اﻟﻣدﯾرﯾﺔ اﻟﻌﺎﻣﺔ ﻟﻠﺗرﺑﯾﺔ ﻓﺮﻋﺎ اﻟﻌﻠﻮم اﻟﻌﺎﻣﺔ وﻋﻠﻮم اﻟﺤﯿﺎة داﺋرة اﻻﻣﺗﺣﺎﻧﺎت ﻣﺳﺎﺑﻘﺔ ﻓﻲ: اﻟﻠﻐﺔ اﻻﻧﻛﻠﯾزﯾﺔ اﻻﺳم: اﻟﻣدة: ﺳﺎﻋﺗﺎن وﻧﺻف اﻟرﻗم: Part One: Reading (Score: 11/20) The writer in this article highlights the essential role of the hormone leptin in controlling obesity. Read it carefully, then answer the questions that follow. Obesity Control 1 New studies on mice suggest that the hormone leptin can fundamentally change the brain’s circuitry in areas that control appetite. Leptin acts during a critical period early in life, possibly influencing how much animals eat as adults. And later in life, responding to how much fat is on an animal’s body, it can again alter brain circuitry that controls how much is eaten. Researchers say the findings are a surprise and help explain why weight control is so hard for some people. 2 Scientists knew that leptin is released by fat cells and that it tells the brain how much fat is on the body. They knew that animals lacking leptin become incredibly obese and that a few humans who, because of genetic mutations do not make the hormone, are also immensely fat. 3 Leptin injections immediately made animals and the handful of patients with leptin deficiencies lose their appetites. Their weight returned to normal. 4 But it was thought that leptin acted like most other hormones by attaching itself to brain cells and directly altering their activities. 5 Some investigators did not expect that leptin could actually change connections in the brain, strengthening circuits that inhibit eating and weakening those that spur appetite. -

2019 Greater Bridgeport Region Bridgeport Hospital and St. Vincent's Medical Center Collaborative Community Health Needs Asse
2019 Greater Bridgeport Region Bridgeport Hospital and St. Vincent’s Medical Center Collaborative Community Health Needs Assessment and Implementation Plan By the Health Improvement Alliance This document is a special section of the Fairfield County Community Wellbeing Index 2019, a core program of DataHaven (ctdatahaven.org), in partnership with Fairfield County’s Community Foundation and a Community Health Needs Assessment for the towns served by all Fairfield County hospitals including Bridgeport Hospital and St. Vincent’s Medical Center 1 | Page ABOUT THIS REPORT This document is a special section of the Fairfield County Community Wellbeing Index 2019 (Appendix A), a comprehensive report about Fairfield County and the towns within it. The Community Index was produced by DataHaven in partnership with Fairfield County’s Community Foundation and many other regional partners, including the Health Improvement Alliance (HIA), a coalition serving towns in the Greater Bridgeport region. This document serves as the Community Health Needs Assessment for the six towns in the HIA area (Bridgeport, Easton, Fairfield, Monroe, Stratford, and Trumbull). The Community Health Needs Assessment documents the process that the HIA used to conduct the regional health assessment and health improvement activities. You may find the full Community Wellbeing Index attached to this section, or posted on the DataHaven, Fairfield County’s Community Foundation, Bridgeport Hospital, St. Vincent’s Medical Center, or any of the town health department websites. The Community Health Needs Assessment and Community Health Improvement Plan were approved by the Board of Trustees for St. Vincent’s Medical Center in June 13, 2019 and the Board of Trustees for Bridgeport Hospital in July 9, 2019. -

Standpoints on Psychiatric Deinstitutionalization Alix Rule Submitted in Partial Fulfillment of the Requirements for the Degre
Standpoints on Psychiatric Deinstitutionalization Alix Rule Submitted in partial fulfillment of the requirements for the degree of Doctor of Philosophy in the Graduate School of Arts and Sciences COLUMBIA UNIVERSITY 2018 © 2018 Alix Rule All rights reserved ABSTRACT Standpoints on Psychiatric Deinstitutionalization Alix Rule Between 1955 and 1985 the United States reduced the population confined in its public mental hospitals from around 600,000 to less than 110,000. This dissertation provides a novel analysis of the movement that advocated for psychiatric deinstitutionalization. To do so, it reconstructs the unfolding setting of the movement’s activity historically, at a number of levels: namely, (1) the growth of private markets in the care of mental illness and the role of federal welfare policy; (2) the contested role of states as actors in driving the process by which these developments effected changes in the mental health system; and (3) the context of relevant events visible to contemporaries. Methods of computational text analysis help to reconstruct this social context, and thus to identify the closure of key opportunities for movement action. In so doing, the dissertation introduces an original method for compiling textual corpora, based on a word-embedding model of ledes published by The New York Times from 1945 to the present. The approach enables researchers to achieve distinct, but equally consistent, actor-oriented descriptions of the social world spanning long periods of time, the forms of which are illustrated here. Substantively, I find that by the early 1970s, the mental health system had disappeared from public view as a part of the field of general medicine — and with it a target around which the existing movement on behalf of the mentally ill might have effectively reorganized itself. -

Your Unpublished Thesis, Submitted for a Degree at Williams College and Administered by the Williams College Libraries, Will Be Made Available for Research Usc
WILLIAMS COLLEGE LIBRARIES COPYRICiHT ASSIGNMENT AND INSTRUCTIONS FOR A STUDENT THESIS Your unpublished thesis, submitted for a degree at Williams College and administered by the Williams College Libraries, will be made available for research usc. You may, through this form, provide instructions regarding copyright, access, dissemination and reproduction of' your thesis. The College has the right in all cases to maintain and preserve theses both in hardcopy and electronic format, and to make such copies as the Libraries require !'or their research and archival functions. _The f~1culty advisor/s to the student writing the thesis claims joint authorship in this work. -~ 1/wc have included in this thesis copyrighted material for which 1/we have not received permission from the copyright holdcr/s. If' you do not secure copyright permissions by the time your thesis is submitted, you will still be allowed to submit. However, if the necessary copyright permissions arc not received, c-posting of your thesis may be affected. Copyrighted material may include images (tables, drawings, photographs, figures, maps, graphs, etc.), sound files, video material, data sets, and large portions of text. l. COI'YRICiiiT An author by law owns the copyright to his/her work, whether or not a copyright symbol and elate arc placed on the piece. Please choose one of the options below with respect to the cupyright in your the,; is. 1/wc choose not to retain the copyright to the thesis, and hereby assign the copyright to Williams College. Selecting this option will assign copyright to the College. !Cthc author/swishes later to publish the work, he/she/they will need to obtain permission to do so Crom the Libraries, which will be granted except in unusual circumstances. -
Final Program
FINAL PROGRAM www.MohsCollege.org/AnnualMeeting THE REVOLUTIONARY 12 QSCRYOSTAT Avantik Biogroup The #1 Name in Mohs. Eliminate chatter, venetian blind & thick/thin Up to 75% Less Noise Ergonomically Designed Adjustable LED Lighting Ultra Smooth Handwheel Operation Precision & Accuracy Perfect Sections Dovetail Bladeholder Perfect Sections Peltier - Fast Freezing UV Disinfection Option The Mohs Laboratory Solution Your laboratory... quick, efficient, easy. The QS12 and QS12UV have been the result of extensive research and development over the span of years. From bladeholder to microtome, cryobar to refrigeration... every aspect of the QS12 and QS12UV is unsurpassed in quality and precision. A Perfect Section...it’s unmistakable! The Mohs Laboratory Performers CALL TODAY TO SPEAK TO YOUR MOHS LAB SPECIALIST REGARDING ALL OF YOUR MOHS LAB NEEDS! 888.392.8411 www.avantik-us.com Table of Contents ACMS Board of Directors ..................................................................................................................................... 2 THE REVOLUTIONARY ACMS Committees and Task Forces – 2016-17 ......................................................................................................... 3 Welcome from the President ................................................................................................................................... 4 12 Welcome from the Scientific Program Committee Chair ............................................................................................... 4 QSCRYOSTAT Program -
Nr********************************************************** I' ,...°4' L`,1 ,'.1{ II
VP DOCUMENT RESUME ED 179 511 SP 014 905 .TITLE Nurse Staffing ReqUirements and Related Toidcs: Sea.ected Bib,licgraphy. Nurse Flanning Information Series No. 9. INSTITUTION Franklin Research Center, Philadelpg), Pa. SPONS AGENCY Health Resources Administration WI /PHS), Bethesda, Md. Div. of Nursing. FEPORT NO HRA-79-39: HRP-0501001 PUB DATE Jul 79 , CONTRACT 232-7R-0000 NOTE 224p. 't EDRS PRICE MF01/PCO9 Plus Postage. U.SCRIPIORS Health Personnel: *Hospital Personnel; *Labor; *Manpower Needs: 'Manpower Utilization; Models; .*Nurses; Nursing: Nursing Homes: *0ccupationa4 Surveys: *Staff Utili2ation ABSTRACT Recent literature on the changing staffing requirements for regitered nurses arid the factors affectingthose requirements is cited in this annctated bibliographythat comprises the ninth volume in the NOrse Planning InformationSeries. A broad concept ot staffing is emplo7cd and includes information usefulto . both managers wit n individual institutions and to heAlth planners concerned with co munity, county, ot state institutions.Abstracts of the literature arg ouped accerding to the following categories: hospitel inpatient nd hospital'outpatient settings; long-termcare settings; models and strategies, and economic-studiesot staffing methodoiogies: regional, state, and national -studies ofneeds and requirements:-and bibliographies And summaries. (JD) 4 *********************************************************************** Reproductions supplied by EPPS are the'best thatcan be made from the origin01 document. ***********Nr********************************************************** I' ,...°4' l`,1 ,'.1{ II l'. ; ).. i ' ,.' .. '. ',"',441. .. ;,.1.1r7 'At, ,. IT. , .. 1 ,:tt . ,.. !,,,,, ;,',i:4.'el:? :: ', , ,,,,a.... .:: y, ;44) .. '' If0V:,:i A ',54,T.i14;, : -4 t ., h.d.'ci!t r "-F 4 , .. tikitiathaNWk e , f , A, .1.1.,..1. ,,,,e it,-.4' i:: re f.:1.,e.. : 'c ,: L'.. it, I , s1,11, :t; ..