MSM in SOUTH AFRICA Data Triangulationproject
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Government Gazette Staatskoerant REPUBLIC of SOUTH AFRICA REPUBLIEK VAN SUID AFRIKA
Government Gazette Staatskoerant REPUBLIC OF SOUTH AFRICA REPUBLIEK VAN SUID AFRIKA Regulation Gazette No. 10177 Regulasiekoerant February Vol. 668 11 2021 No. 44146 Februarie ISSN 1682-5845 N.B. The Government Printing Works will 44146 not be held responsible for the quality of “Hard Copies” or “Electronic Files” submitted for publication purposes 9 771682 584003 AIDS HELPLINE: 0800-0123-22 Prevention is the cure 2 No. 44146 GOVERNMENT GAZETTE, 11 FEBRUARY 2021 IMPORTANT NOTICE: THE GOVERNMENT PRINTING WORKS WILL NOT BE HELD RESPONSIBLE FOR ANY ERRORS THAT MIGHT OCCUR DUE TO THE SUBMISSION OF INCOMPLETE / INCORRECT / ILLEGIBLE COPY. NO FUTURE QUERIES WILL BE HANDLED IN CONNECTION WITH THE ABOVE. Contents Gazette Page No. No. No. GOVERNMENT NOTICES • GOEWERMENTSKENNISGEWINGS Transport, Department of / Vervoer, Departement van 82 South African National Roads Agency Limited and National Roads Act (7/1998): Huguenot, Vaal River, Great North, Tsitsikamma, South Coast, North Coast, Mariannhill, Magalies, N17 and R30/R730/R34 Toll Roads: Publication of the amounts of Toll for the different categories of motor vehicles, and the date and time from which the toll tariffs shall become payable .............................................................................................................................................. 44146 3 82 Suid-Afrikaanse Nasionale Padagentskap Beperk en Nasionale Paaie Wet (7/1998) : Hugenote, Vaalrivier, Verre Noord, Tsitsikamma, Suidkus, Noordkus, Mariannhill, Magalies, N17 en R30/R730/R34 Tolpaaie: Publisering -
Casterbridge-Fact-Sheet.Pdf
TOP 25 HOTELS IN SOUTH AFRICA WHITE RIVER I MPUMALANGA www.casterbridgehollow.co.za AUGUST 2019 Pilgrim’sGRASKOP Rest R535 Graskop HAZYVIEW R536 Hazyview Kruger National Park MOZAMBIQUE LIMPOPO PROVINCE KRUGER BOTSWANA Skukuza NATIONAL CASTERBRIDGE SABIE PARK HOLLOW R40 Johannesburg Sabie R538 NAMIBIA NORTH WEST PROVINCE GAUTENG MPUMALANGA Pretoriuskop SWAZILAND R37 R537 FREE STATE KWAZULU- NATAL White River LESOTHO KRUGER NORTHERN CAPE WHITE RIVER Casterbridge Lifestyle Centre Durban NATIONAL PLASTON PARK EASTERN CAPE R37 KMIA Kruger Mpumalanga R40 International Airport WESTERN CAPE Cape Town N4 NELSPRUIT N4 R40 WHITE RIVER I MPUMALANGA Casterbridge, once a spreading Mango plantation in White River, has been transformed into one of the most original and enchanting country estates in South Africa. Just 20 km from Nelspruit, a mere 40 km from Hazyview and Sabie; White River has become home to a host of creative talents; artists, designers, fine craftsmen, ceramicists, cooks and restaurateurs. Casterbridge Hollow is a concept that has evolved with great charm with colours reminiscent of romantic hillside villages in Provence and Tuscany. LOCATION • Casterbridge Hollow Boutique Hotel is situated outside White River. • It is the ideal destination from which to access the reserves of the Lowveld and the attractions of Mpumalanga. ACCOMMODATION 30 ROOMS • 24 Standard, 2 Honeymoon and 4 Family • Air-conditioning and heating • Ceiling fans • Balconies overlook the courtyard and swimming pool • Satellite television • Tea / coffee making facilities -

Directions from Johannesburg to Makalali Private Game Lodge • The
Directions from Johannesburg to Makalali Private Game Lodge • The distance from Johannesburg to Makalali Lodge is approx 480 km. • Take the N1 North towards Pretoria. • Take the N4 east to eMalahleni (previously Witbank) and onwards to Belfast (Pretoria to Belfast ± 240 km). • Turn left off the highway to Belfast. • In Belfast, turn right onto the Dullstroom / Mashishing (previously Lydenberg) road (R540). • At the T-Junction (R540 & R36) turn left into Mashishing (previously Lydenberg). • In Mashishing, at the Ohrigstad sign, turn left and follow the main road of Mashishing (De Clerq Street) onto the Ohrigstad road (R36). • Follow the R36 through Ohrigstad and on through the Strijdom Tunnel. • Turn left towards Tzaneen at the next T-junction (Giraffe Junction). There is a Total garage on your left – This is also your last petrol stop before the Lodge. • Follow the road over the Olifants River, slowly (60kph) past the Oaks (local village) for approx 7km and just past the Phalaborwa / Mica turnoff, look for Makalali signs. • Turn right at Gravelotte turnoff (D202); this immediately becomes a gravel road. Go through the boom gate. • Travel ±9 km on the gravel road to the Makalali Main Gate on your right-hand side. Reception is a further 11 km (30 min), through the Reserve. Directions from Hazyview and Nelspruit to Makalali Private Game Lodge • Take R40 North towards Phalaborwa. • At the 4-way stop in Hazyview (Perry’s Bridge Centre) take the turn off towards Sabie R536, past Casa do Sol. • Go through Sabie towards Graskop • Through Graskop towards God’s Window • At the T-Junction turn Right towards the Abel Erasmus Pass • Go through the JG Strijdom tunnel • Take a left turn on the R36 towards Tzaneen • Turn right onto the Gravelotte Road, a gravel road • Head on for about 9km until you see the Makalali stone pillars • Main Gate to Reception is a further 11km (30min) in the Reserve. -

Map & Directions: Regional Head Office Johannesburg
Johannesburg Map & Directions: Regional Head Office Johannesburg Directions from Johannesburg Directions from OR Tambo PHYSICAL ADDRESS: CBD (Newtown) International Airport Yokogawa SA (Pty) Ltd Block C, Cresta Junction Distance: 12.8Km Distance: 48.3Km Corner Beyers Naude Drive and Approximate time: 23 minutes Approximate time: 39 minutes Judges Avenue Cresta Head west on Jeppe St towards Henry Get on to the R24 from To Parking Road Johannesburg, 2194 Nxumalo Street. Continue onto Mahlathini and Exit 46. Keep right at the fork to Street and turn right onto Malherbe Street continue on Exit 46, follow the signs for POSTAL ADDRESS: then turn left onto Lilian Ngoyi Street. Take R24/Johannesburg. Continue on the R24 Yokogawa SA (Pty) Ltd a slight right onto Burghersdorp Street and until it merges with the N12. Continue until PostNet Suite #222 a slight left onto Carr Street. Continue onto exit 113 and take that exit to get onto the Private Bag X1 Subway Street. Turn right onto Seventeenth N3 South/N12 toward M2/Kimberley/ Northcliff, 2115 Street then turn left onto Solomon Street. Germiston/Durban. Keep right at the fork Continue onto Annet Road. Take a slight and follow the signs for N3 S: -26.12737 E: 27.97000 right to stay on Annet Road and continue North/N1/Pretoria and merge onto N3 onto Barry Hertzog Avenue. Turn left onto Eastern Bypass/N1. Continue for 18km. Judith Road after the Barry Hertzog bends. Get into the left lane to take the M5/ Continue on Judith road to the T-junction Beyers Naude Drive exit towards and turn right onto Beyers Naude Drive Honeydew/Northcliff. -

The Health and Health System of South Africa: Historical Roots of Current Public Health Challenges
Series Health in South Africa 1 The health and health system of South Africa: historical roots of current public health challenges Hoosen Coovadia, Rachel Jewkes, Peter Barron, David Sanders, Diane McIntyre The roots of a dysfunctional health system and the collision of the epidemics of communicable and non-communicable Lancet 2009; 374: 817–34 diseases in South Africa can be found in policies from periods of the country’s history, from colonial subjugation, Published Online apartheid dispossession, to the post-apartheid period. Racial and gender discrimination, the migrant labour system, August 25, 2009 the destruction of family life, vast income inequalities, and extreme violence have all formed part of South Africa’s DOI:10.1016/S0140- 6736(09)60951-X troubled past, and all have inexorably aff ected health and health services. In 1994, when apartheid ended, the health See Editorial page 757 system faced massive challenges, many of which still persist. Macroeconomic policies, fostering growth rather than See Comment pages 759 redistribution, contributed to the persistence of economic disparities between races despite a large expansion in and 760 social grants. The public health system has been transformed into an integrated, comprehensive national service, but See Perspectives page 777 failures in leadership and stewardship and weak management have led to inadequate implementation of what are This is fi rst in a Series of often good policies. Pivotal facets of primary health care are not in place and there is a substantial human resources six papers on health in crisis facing the health sector. The HIV epidemic has contributed to and accelerated these challenges. -
Gauteng Gauteng
Gauteng Gauteng Thousands of visitors to South Africa make Gauteng their first stop, but most don’t stay long enough to appreciate all it has in store. They’re missing out. With two vibrant cities, Johannesburg and Tshwane (Pretoria), and a hinterland stuffed with cultural treasures, there’s a great deal more to this province than Jo’burg Striking gold International Airport, says John Malathronas. “The golf course was created in 1974,” said in Pimville, Soweto, and the fact that ‘anyone’ the manager. “Eighteen holes, par 72.” could become a member of the previously black- It was a Monday afternoon and the tees only Soweto Country Club, was spoken with due were relatively quiet: fewer than a dozen people satisfaction. I looked around. Some fairways were in the heart of were swinging their clubs among the greens. overgrown and others so dried up it was difficult to “We now have 190 full-time members,” my host tell the bunkers from the greens. Still, the advent went on. “It costs 350 rand per year to join for of a fully-functioning golf course, an oasis of the first year and 250 rand per year afterwards. tranquillity in the noisy, bustling township, was, But day membership costs 60 rand only. Of indeed, an achievement of which to be proud. course, now anyone can become a member.” Thirty years after the Soweto schoolboys South Africa This last sentence hit home. I was, after all, rebelled against the apartheid regime and carved ll 40 Travel Africa Travel Africa 41 ERIC NATHAN / ALAMY NATHAN ERIC Gauteng Gauteng LERATO MADUNA / REUTERS LERATO its name into the annals of modern history, the The seeping transformation township’s predicament can be summed up by Tswaing the word I kept hearing during my time there: of Jo’burg is taking visitors by R511 Crater ‘upgraded’. -

Greylingstad Mpumalanga Done by Do
Archaeological investigations, done at Bakkiesfontein 568 IR, (Dipaliseng Local Municipality) Greylingstad Mpumalanga Done by Domonique-Marie Verkerk BHSC (Heritage and Cultural Tourism), 2011, UP BA Archaeology, 2012, UP Tel: 012 3333931 E-mail: [email protected] Department of Anthropology and Archaeology, University of Pretoria 5 October 2015 Summary Concentration camps were a tactic created by the British to end the South African War (1899- 1902). Many innocent Boer and African families were sent to these camps where they died of diseases, such as, poor conditions and lack of shelters. Boer families were sent to concentration camps in Heidelberg. Africans, on the other hand, were sent to the concentration camp in Greylingstad. A possible location for the African concentration camp in Greylingstad is Bakkiesfontein 568 IR. Unfortunately, there is nothing to show where this camp is as a fire destroyed many of the records. Bakkiesfontein 568 IR was chosen as a possible location for the African concentration camp in Greylingstad because of the old house, stream, stone walls, railway, SR fort and the African cemetery. Bakkiesfontein was surveyed by foot. The aim was to find the location of the concentration camp. Areas where pedestrian surveys were conducted included the house, barn, possible midden, graves, stone walls and stone circle. The pedestrian survey showed that Iron Age communities also lived on the farm. Three test-pits were also conducted. Areas where the test-pits were conducted included the midden, between stone walls and on a slope near a stone wall. The test-pits were not that successful. The artefacts found during the test- pits and surveys include; metal, ceramic pieces and pottery, glass pieces and even plastic. -

Hello Limpopo 2019 V7 Repro.Indd 1 2019/11/05 10:58 Driving the Growth of Limpopo
2019 LIMPOPOLIMPOPO Produced by SANRAL The province needs adequate national roads to grow the economy. As SANRAL, not only are we committed to our mandate to manage South Africa’s road infrastructure but we place particular focus on making sure that our roads are meticulously engineered for all road users. www.sanral.co.za @sanral_za @sanralza @sanral_za SANRAL SANRAL Corporate 5830 Hello Limpopo 2019 V7 Repro.indd 1 2019/11/05 10:58 Driving the growth of Limpopo DR MONNICA MOCHADI especially during high peak periods. We thus welcome the installation of cutting-edge technology near the he Limpopo provincial government is committed Kranskop Toll Plaza in Modimolle which have already to the expansion and improvement of our primary contributed to a reduction in fatalities on one of the Troad network. busiest stretches of roads. Roads play a critical role in all of the priority SANRAL’s contribution to the transformation of the economic sectors identified in the Provincial Growth construction sector must be applauded. An increasing and Development Strategy, most notably tourism, number of black-owned companies and enterprises agriculture, mining and commerce. The bulk of our owned by women are now participating in construction products and services are carried on the primary road and road maintenance projects and acquiring skills that network and none of our world-class heritage and will enable them to grow and create more jobs. tourism sites would be accessible without the existence This publication, Hello Limpopo, celebrates the of well-designed and well-maintained roads. productive relationship that exists between the South It is encouraging to note that some of the critical African National Roads Agency and the province of construction projects that were placed on hold have Limpopo. -
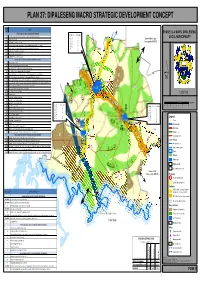
Dipaleseng Macro Strategic Development Concept
PLAN 37: DIPALESENG MACRO STRATEGIC DEVELOPMENT CONCEPT Project Projects No SPATIAL OBJECTIVE: EXPLOIT ECONOMIC OPPORTUNITIES T 7 PHASE 3 & 4 MAPS: DIPALESENG PROJECTS: STRATEGIES: o 1 N /N 1 Compilation of an implementation plan to create mining enabling environment 17 18 C n i o g v LOCAL MUNICIPALITY 2 Beneficiation of coal 24 28 D e e Govan Mbeki Local 29 35 F l D o F Municipality (MP307) 3 (n/a) Development of a Tourism Strategy 38 43 G T 4 (n/a) Access suitable land for irrigation farming and beneficiation of agricultural products 44 46 H 47 50 I 5 (n/a) Access agricultural support programmes for the development of arable land 52 J 1! 7 (n/a) Beneficiation of agricultural products K 23! 8 (n/a) Implement land reform Programme L L 8 15 (n/a) SMME/BEE Development Programmes 4 5 SPATIAL OBJECTIVE: CREATE SUSTAINABLE HUMAN SETTLEMENTS R 17 Thusong service centres. F 18 Draft detailed Urban Design Framework for nodes E P e t r u s v d M e r w e ! 19 Upgrade of the R23 road between Greylingstad and Balfour P e t r u s v d M e r w e 1 1 5 HHaarrooffff DDaamm 20 Upgrade of the R51 road between Balfour and Grootvlei R 21! 21 Maintain R23 transport corridor to the east of Greylingstad and to the north of Balfour N 22 (n/a) Upgrade gravel access roads to schools to enable public transport provision 23 Maintain R51-R548 main road south of Grootvlei (to Vaal River) and north of Balfour (to Devon, Secunda) F 55! ´ S i y a t h e m b a 24 Develop services master plans (roads, water, sewer, electricity) for Balfour, Greylingstad and Grootvlei T S i y a t h e m b a o 28 Identification of new cemetery and land fill sites in all main towns H / ! B 1 ! e /!!! 53 L B aa ll ff o u r L 29 Upgrade Main Substations (Bulk Electricity supply) id ! u r e 53 30 (n/a) Rural Water Supply (15 boreholes) lb e 32 (n/a) Provision of VIP's rg 1:320 000 35 Develop Storm Water Master Plan N N 19! 38 Sewer Reticulation & Maintenance L B B R 39 Sewer Reticulation 700 H/H Ext. -

20 Sharland Street, Driehoek (Germiston)
DIRECTIONS TO NEW PREMISES OF RGS GROUP/ MEGA MAGAZINES/ SMART THINKING - 20 SHARLAND STREET, DRIEHOEK (GERMISTON) From West Rand From South 1) N1 Western by pass 1) Get on M1 2) Follow signs to the N12 2) Use the right 2 lanes to take exit 10 to merge onto Francois Oberholzer Fwy/M2 3) Continue onto N12 toward Stad/City 4) Take Germiston Exit 3) Keep right, follow signs for M2/Germiston 5) Keep right follow signs for M2 Germiston 4) Continue onto Francois Oberholzer Freeway 6) Continue onto Francois Oberholzer Freeway 5) Turn left onto Refinery Road 7) Turn left onto Refinery Road 6) Turn left onto Sharland Street 8) Turn left onto Sharland Street 7) Destination : 20 Sharland Street 9) Destination : 20 Sharland Street From East Rand From Pretoria 1) Get on N12 toward Johannesburg 1) Take the ramp onto Nelson Mandela Dr/M3/M5 2) Continue on N12 to Germiston. Take exit 108-Geldenhuys 2) Continue to follow R21 from N3 Eastern Bypass/N12/N3 4) Use the right 3 lanes to take the R24 exit toward N3/Johannesburg 3) Merge onto N12 5) Continue onto R24 4) Use the left 3 lanes to take exit 113 for N3 S/N12 toward 6) Merge onto N12/R24 M2/Kimberley/Germiston/Durban 7) Use the left 3 lanes to take exit 113 for N3 S/N12 toward M2/Kimberley 5) Merge onto N3 Eastern Bypass/N12/N3\ /Germiston/Durban 6) At the interchange 108-Geldenhuys 8) Merge onto N3 Eastern Bypass/N12/N3 7) Use the left lane to follow signs for Germiston 9) At the interchange 108-Geldenhuys 8) Continue onto Francois Oberholzer Freeway 10) Use the left lane to follow signs for Germiston 9) Turn left onto Refinery Road 11) Continue onto Francois Oberholzer Freeway 10) Turn left onto Sharland Street 12) Turn left onto Refinery Road 11) Destination : 20 Sharland Street 13) Turn left onto Sharland Street 14) Destination : 20 Sharland Street 12) . -
Gautrain Construction Update
Month end 30 April 2008 Gautrain construction update SOUTHERN SECTION Within the station box, waler beams and struts have been Underground section installed to provide temporary lateral support to the perimeter Park Station walls during station box excavation. Excavation of the single-track rail tunnel towards Emergency Shaft 2 in Houghton has reached approximately 310 m from the Emergency Shaft 1 (Hillbrow) tunnel portal. Construction of the underground station box and The single-track rail tunnel between Park Station and Sandton multi-storey parkade foundation is making good progress. Station will feature seven emergency access shafts. These shafts will provide emergency services personnel access to the tun- 1 nels below. At the bases of these shafts there will be safe havens where passengers can gather in case of an emergency. The land required for Emergency Shaft 1 in Hillbrow is in the process of being expropriated. Site establishment and shaft exca- vation will start once this process has been completed. Emergency Shaft 2 (The Wilds, Houghton) At Shaft E2, shaft lining was completed to the 38 m depth above the cavern and grouting ahead of the cavern excavation was in progress. Once this cavern is complete, an adit linking the bottom of the shaft to the tunnel alignment will be excavated, from where two rail tunnel sections will be excavated. The one tunnel will head south towards Park Station, while the other 2 tunnel will head north towards Rosebank Station. Emergency Shaft 3 (Riviera) Construction of this shaft will start soon. The construction site has been hoarded and site establishment has commenced. -

REUNERT LIMITED (Incorporated in the Republic of South Africa
REUNERT LIMITED (Incorporated in the Republic of South Africa) (Registration number: 1913/004355/06) ISIN: ZAE000057428 Share code: RLO (“Reunert” or the “Company” or the “Group”) FINALISATION OF ACQUISITION OF SHARES IN ACCORDANCE WITH CSP HEDGING TRANSACTION Reunert shareholders (“Shareholders”) are referred to the announcement published on SENS on 30 September 2020 wherein Shareholders were advised of the hedging transaction entered into between Reunert and Investec Bank Limited (“Investec”), an independent third party, on behalf of the Reunert 2019 Conditional Share Plan (“CSP”), to hedge the potential future obligations of the CSP (the “Hedging Transaction”), as provided for in the CSP rules. As required by the JSE Limited Listings Requirements (“Listings Requirements”), a purchase programme was put in place prior to the commencement of Reunert’s closed period on 1 October 2020. In accordance with paragraph 14.9(f) of schedule 14 of the Listings Requirements, Shareholders are advised of the following acquisitions of Reunert ordinary shares (“Shares”) on behalf of the CSP, in execution of the Hedging Transaction, between 30 September 2020 and 19 November 2020: Name of entity: Investec, on behalf of the CSP Class of securities: Ordinary shares Nature of transaction: Purchase of Shares pursuant to the Hedging Transaction Transaction completed: On-market Total number of Shares acquired: 2 346 930 Total value of Shares acquired: R79 032 108 Nature of interest: Indirect beneficial (purchased by Investec acting as an independent agent on