Ertugliflozin Compared to Other Anti-Hyperglycemic Agents As
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Steglujan, INN-Ertugliflozin-Sitagliptin
25 January 2018 EMA/86941/2018 Committee for Medicinal Products for Human Use (CHMP) Assessment report Steglujan International non-proprietary name: ertugliflozin / sitagliptin Procedure No. EMEA/H/C/004313/0000 Note Assessment report as adopted by the CHMP with all information of a commercially confidential nature deleted. 30 Churchill Place ● Canary Wharf ● London E14 5EU ● United Kingdom Telephone +44 (0)20 3660 6000 Facsimile +44 (0)20 3660 5555 Send a question via our website www.ema.europa.eu/contact An agency of the European Union © European Medicines Agency, 2018. Reproduction is authorised provided the source is acknowledged. Table of contents 1. Background information on the procedure .............................................. 7 1.1. Submission of the dossier ...................................................................................... 7 1.2. Steps taken for the assessment of the product ......................................................... 8 2. Scientific discussion ................................................................................ 9 2.1. Problem statement ............................................................................................... 9 2.1.1. Disease or condition ........................................................................................... 9 2.1.2. Epidemiology .................................................................................................... 9 2.1.3. Clinical presentation .......................................................................................... -

Steglujan (Ertugliflozin/Sitagliptin), Segluromet
Steglatro™ (ertugliflozin), Steglujan™ (ertugliflozin/sitagliptin), Segluromet™ (ertugliflozin/metformin) – New drug approval • On December 19, 2017, the FDA approved Merck’s Steglatro (ertugliflozin), Steglujan (ertugliflozin/sitagliptin), and Segluromet (ertugliflozin/metformin) as an adjunct to diet and exercise to improve glycemic control in adults with type 2 diabetes mellitus (T2DM). — Steglujan is indicated when treatment with both ertugliflozin and sitagliptin is appropriate. — Segluromet is indicated when patients are not adequately controlled on a regimen containing ertugliflozin or metformin, or in patients who are already treated with both ertugliflozin and metformin. — These drugs are not recommended in patients with type 1 diabetes mellitus (T1DM) or for the treatment of diabetic ketoacidosis. — Steglujan has not been studied in patients with a history of pancreatitis. It is unknown whether patients with a history of pancreatitis are at increased risk for the development of pancreatitis while using Steglujan. • Ertugliflozin is the fourth sodium-glucose co-transoporter-2 (SGLT2) inhibitor approved by the FDA. Other marketed SGLT2 inhibitors include Jardiance® (empagliflozin), Farxiga® (dapagliflozin), and Invokana® (canagliflozin). • The efficacy and safety of ertugliflozin were evaluated in multiple clinical studies involving patients with T2DM. Ertugliflozin was studied as monotherapy and in combination with metformin and/or a dipeptidyl peptidase 4 (DPP-4) inhibitor. Ertugliflozin was also studied in combination with other antidiabetic medications, including insulin and a sulfonylurea, and in T2DM patients with moderate renal impairment. — In patients with T2DM, treatment with ertugliflozin, ertugliflozin + sitagliptin, and ertugliflozin + metformin reduced hemoglobin A1c (HbA1c) vs. placebo or the active comparator. — In patients with T2DM and moderate renal impairment, treatment with ertugliflozin did not result in a reduction in HbA1c vs. -

Newer Diabetes Treatments Drug Class Update with New Drug Evaluation: Semaglutide and Ertugliflozin
© Copyright 2012 Oregon State University. All Rights Reserved Drug Use Research & Management Program Oregon State University, 500 Summer Street NE, E35 Salem, Oregon 97301-1079 Phone 503-947-5220 | Fax 503-947-1119 Newer Diabetes Treatments Drug Class Update with New Drug Evaluation: Semaglutide and Ertugliflozin Date of Review: July 2018 Date of Last Review: September 2017 End Date of Literature Search: 05/23/2018 Generic Name: semaglutide Brand Name (Manufacturer): Ozempic® (Novo Nordisk) Generic Name: ertugliflozin, ertugliflozin/sitagliptin, ertugliflozin/metformin Brand Name (Manufacturer): Steglatro™, Steglujan™, Segluromet™ (Merck & Co., Inc.) Dossier Received: ertugliflozin (yes), semaglutide (no) Current Status of PDL Class: See Appendix 1. Purpose for Class Update: To evaluate the safety and efficacy of semaglutide and ertugliflozin (and combinations) which were recently approved for blood glucose lowering in patients with type 2 diabetes mellitus (T2DM). High quality new evidence published since the last review will also be presented. Research Questions: 1. In patients with T2DM, is there any new comparative evidence for non-insulin antidiabetic therapies based on surrogate efficacy outcomes (e.g., hemoglobin A1c [HbA1c]) and long-term clinically meaningful effectiveness outcomes (e.g., microvascular outcomes, macrovascular outcomes and mortality)? 2. In patients with T2DM, is there any new comparative evidence for non-insulin diabetes treatments based on harms outcomes (e.g., severe hypoglycemia, heart failure, diabetic ketoacidosis, pancreatitis, etc.)? 3. Are there subpopulations of patients with T2DM for which specific therapies may be more effective or associated with less harm? 4. What are the efficacy and harms evidence for the two new non-insulin diabetes treatments, ertugliflozin and semaglutide? Conclusions: A Drug Effectiveness Review Project (DERP) update on newer diabetes therapies, three new guidelines/standards, one new randomized controlled trial and two new drug reviews were reviewed for this class update. -

SEGLUROMET, INN-Ertugliflozin-Metformin
ANNEX I SUMMARY OF PRODUCT CHARACTERISTICS 1 This medicinal product is subject to additional monitoring. This will allow quick identification of new safety information. Healthcare professionals are asked to report any suspected adverse reactions. See section 4.8 for how to report adverse reactions. 1. NAME OF THE MEDICINAL PRODUCT Segluromet 2.5 mg/850 mg film-coated tablets Segluromet 2.5 mg/1,000 mg film-coated tablets Segluromet 7.5 mg/850 mg film-coated tablets Segluromet 7.5 mg/1,000 mg film-coated tablets 2. QUALITATIVE AND QUANTITATIVE COMPOSITION Segluromet 2.5 mg/850 mg film-coated tablets Each tablet contains 2.5 mg ertugliflozin (as ertugliflozin L-pyroglutamic acid) and 850 mg of metformin hydrochloride. Segluromet 2.5 mg/1,000 mg film-coated tablets Each tablet contains 2.5 mg ertugliflozin (as ertugliflozin L-pyroglutamic acid) and 1,000 mg of metformin hydrochloride. Segluromet 7.5 mg/850 mg film-coated tablets Each tablet contains 7.5 mg ertugliflozin (as ertugliflozin L-pyroglutamic acid) and 850 mg metformin hydrochloride. Segluromet 7.5 mg/1,000 mg film-coated tablets Each tablet contains 7.5 mg ertugliflozin (as ertugliflozin L-pyroglutamic acid) and 1,000 mg metformin hydrochloride. For the full list of excipients, see section 6.1. 3. PHARMACEUTICAL FORM Film-coated tablet (tablet). Segluromet 2.5 mg/850 mg film-coated tablets Beige, 18 x 10 mm oval, film-coated tablet debossed with “2.5/850” on one side and plain on the other side. Segluromet 2.5 mg/1,000 mg film-coated tablets Pink, 19.1 x 10.6 mm oval, film-coated tablet debossed with “2.5/1000” on one side and plain on the other side. -

SGLT2) Inhibitors (Gliflozins) in Adults with Type 2 Diabetes (T2DM
Sodium-glucose cotransporter-2 (SGLT2) inhibitors (Gliflozins) in Adults with Type 2 Diabetes (T2DM) There are currently four SGLT2 inhibitors (canagliflozin, dapagliflozin, empagliflozin and ertugliflozin) licensed in the UK for the management of adults with T2DM. No head to head trials between the SGLT2 inhibitors have been conducted. As at December 2019, clinical outcome data is available for three of the four SGLT2 inhibitors around their cardiovascular effects in people with T2DM. Ertugliflozin is still to report on this data. This document summarises the key prescribing considerations. NICE Technology Appraisal Recommendation NICE makes recommendations for when SGLT2 inhibitors can be considered in adults with T2DM; Hertfordshire Medicines Management Committee Recommendations are in line with NICE guidance: Monotherapy NICE TA 390: Canagliflozin, Dapagliflozin and Empagliflozin and NICE TA 572: Ertugliflozin as monotherapies for treating T2DM Monotherapy recommended as option in adults for whom metformin is contraindicated or not tolerated and when diet & exercise alone do not provide adequate glycaemic control, only if: •a DPP‑4 inhibitor would otherwise be prescribed and •a sulfonylurea or pioglitazone is not appropriate. Dual therapy NICE TA 315: Canagliflozin, NICE TA288: Dapagliflozin, TA 336: Empagliflozin, TA 572: Ertugliflozin as combination therapies for treating T2DM In a dual therapy regimen in combination with metformin is recommended as an option, only if: •a sulfonylurea is contraindicated or not tolerated or •the person is at significant risk of hypoglycaemia or its consequences. In combination with insulin NICE TA 315: Canagliflozin, NICE TA288: Dapagliflozin, TA 336: Empagliflozin in combination with insulin with or without other antidiabetic drugs is recommended as an option. -
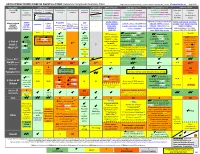
ANTI-HYPERGLYCEMIC DIABETES AGENTS in T2DM: Color Outcomes Comparison Summary Table
ANTI-HYPERGLYCEMIC DIABETES AGENTS in T2DM: Outcomes Comparison Summary Table L Regier BSP BA, M LeBras PharmD, T Trischuk PharmD, J Bareham BSP, L Lu BSP © www.RxFiles.ca Aug 2021 Drug Class Sulfonylureas TZDs Meglitinides DPP4 Inhibitors GLP1 Agonists *** SGLT2 Inhibitors *** Insulin in T2DM Generic Metformin Gliclazide Glyburide Pioglitazone Rosiglitazone Acarbose Repaglinide Saxagliptin ONGLYZA Liraglutide VICTOZA Empagliflozin JARDIANCE Intensity: Intensity: BRAND (MF) DIAMICRON DIABETA ACTOS, g AVANDIA GLUCOBAY GLUCONORM Sitagliptin JANUVIA Exenatide BYETTA, BYDUREON Canagliflozin INVOKANA Less More GLUCOPHAGE Dulaglutide TRULICITY Dapagliflozin FORXIGA, FARXIGA Alogliptin NESINA (e.g. NPH (Multiple daily GLUCOTROL D/C STEGLATRO Glipizide Nateglinide Semaglutide OZEMPIC, RYBELSUS (PO) Ertugliflozin Linagliptin TRAJENTA HS + MF) doses) STARLIX D/C SPREAD-DIMCAD] Lixisenatide ADLYXINE; ALBIGLUTIDE D/C SAVOR-TIMI 53, EMPA-REG, CANVAS, CREDENCE, T2DM: UKPDS-33,80; ADVANCE, Major trials to UKPDS- ProACTIVE ACE 33,34,80 UKPDS- Meta-analysis. TECOS, EXAMINE LEADER, EXSCEL, FREEDOM CVO, DECLARE, VERTIS-CV (2020), ACCORD, VADT, ORIGIN, DEVOTE support ADVANCE (Prevention (ADOPT; 33,80 Ferwana M. Meta- RECORD interim, PROLOGUE, REWIND, SUSTAIN-6, PIONEER-6, DAPA-HF, DAPA-CKD (2020), T1DM: DCCT/EDIC findings/ analysis 2013. trial: Stop- - some use in (ADOPT) ADOPT, DREAM CARMELINA, EMPEROR-Reduced & -Preserved (Also Boussageon et al. Meta- Outcomes* ADVANCE) SR-Liao 2017; IRIS NIDDM) ELIXA, HARMONY CAROLINA (2020), EMPA-Kidney (2022) analysis. -

STEGLUJAN Safely and Effectively
therapy in clinical situations known to predispose to ketoacidosis. HIGHLIGHTS OF PRESCRIBING INFORMATION (5.3) These highlights do not include all the information needed to use • Acute Kidney Injury and Impairment in Renal Function: Consider STEGLUJAN safely and effectively. See full prescribing temporarily discontinuing in settings of reduced oral intake or fluid information for STEGLUJAN. losses. If acute kidney injury occurs, discontinue and promptly treat. There have been postmarketing reports of acute renal failure in STEGLUJAN™ (ertugliflozin and sitagliptin) tablets, for oral use patients taking sitagliptin, sometimes requiring dialysis. Monitor Initial U.S. Approval: 2017 renal function. (5.4) • Urosepsis and Pyelonephritis: Evaluate patients for signs and ----------------------------INDICATIONS AND USAGE --------------------------- symptoms of urinary tract infections and treat promptly, if indicated. STEGLUJAN is a combination of ertugliflozin, a sodium glucose co- (5.5) transporter 2 (SGLT2) inhibitor, and sitagliptin, a dipeptidyl peptidase-4 • Lower Limb Amputation: Before initiating, consider factors that may (DPP-4) inhibitor, indicated as an adjunct to diet and exercise to increase risk of amputation. Monitor patients for infections or ulcers improve glycemic control in adults with type 2 diabetes mellitus when of lower limbs, and discontinue if these occur. (5.6) treatment with both ertugliflozin and sitagliptin is appropriate. (1) • Heart Failure: Heart failure has been observed with two other members of the DPP-4 inhibitor class. Consider risks and benefits in Limitations of Use: patients who have known risk factors for heart failure. Monitor • Not for the treatment of type 1 diabetes mellitus or diabetic patients for signs and symptoms. (5.7) ketoacidosis. (1) • Hypoglycemia: Consider a lower dose of insulin or insulin • Has not been studied in patients with a history of pancreatitis. -

Merck to Present Phase 3 Data on Investigational Medicines Ertugli�Ozin and MK-1293 at the 76Th Scienti�C Sessions of the American Diabetes Association
NEWS RELEASE Merck to Present Phase 3 Data on Investigational Medicines Ertugliozin and MK-1293 at the 76th Scientic Sessions of the American Diabetes Association 5/12/2016 Additional Analyses from the TECOS Cardiovascular Safety Trial of JANUVIA® (sitagliptin) Also to Be Presented Merck (NYSE: MRK), known as MSD outside the United States and Canada, today announced that researchers will present data from clinical trials of its investigational diabetes pipeline, JANUVIA® (sitagliptin), and new real-world research in more than 20 scientic data presentations at the 76th Scientic Sessions of the American Diabetes Association (ADA) being held in New Orleans, June 10-14, 2016. New investigational clinical trial data to be presented include the rst Phase 3 results for ertugliozin, an oral SGLT2 inhibitor in development with Pzer for patients with type 2 diabetes, and for MK-1293, Merck’s follow-on biologic insulin glargine candidate being evaluated for patients with type 1 and type 2 diabetes. Additional analyses will also be presented from the TECOS (Trial Evaluating Cardiovascular Outcomes with Sitagliptin) cardiovascular safety trial of JANUVIA. “At Merck, we have a long-term commitment to diabetes research and advancing the care of people living with diabetes around the world,” said Peter Stein, M.D., vice president, late stage development, diabetes and endocrinology, Merck. “We look forward to presenting new clinical trial data and results of several studies from real- world settings at this year’s American Diabetes Association Scientic Sessions.” Indications and Usage for JANUVIA (sitagliptin) 25 mg, 50 mg and 100 mg tablets JANUVIA is indicated, as an adjunct to diet and exercise, to improve glycemic control in adults with type 2 diabetes 1 mellitus. -

Attachment: Product Information: Ertugliflozin / Sitagliptin
Attachment 1: Product information AusPAR Steglatro, Steglujan and Segluromet - Ertugliflozin monotherapy; Ertugliflozin Sitagliptin FDC; Ertugliflozin Metformin FDC - Merck Sharpe and Dohme Pty Ltd PM-2017-01328-1-5/PM-2017-01329-1-5/PM-2017-01330-1-5 FINAL 5 February 2019. This is the Product Information that was approved with the submission described in this AusPAR. It may have been superseded. For the most recent PI, please refer to the TGA website at <https://www.tga.gov.au/product-information-pi> ▼This medicinal product is subject to additional monitoring in Australia. This will allow quick identification of new safety information. Healthcare professionals are asked to report any suspected adverse events at https://www.tga.gov.au/reporting-problems. AUSTRALIAN PRODUCT INFORMATION - STEGLUJAN® (Ertugliflozin/Sitagliptin) 1 NAME OF THE MEDICINE Ertugliflozin / sitagliptin 2 QUALITATIVE AND QUANTITATIVE COMPOSITION STEGLUJAN contains ertugliflozin, a sodium-glucose co-transporter 2 (SGLT2) inhibitor and sitagliptin phosphate, a dipeptidyl peptidase 4 (DPP-4) inhibitor. STEGLUJAN is available for oral use as film-coated tablets containing: · 6.48 mg ertugliflozin pyroglutamic acid equivalent to 5 mg of ertugliflozin and 128.5 mg sitagliptin phosphate monohydrate equivalent to 100 mg of sitagliptin (STEGLUJAN 5 / 100) · 19.43 mg ertugliflozin pyroglutamic acid equivalent to 15 mg of ertugliflozin and 128.5 mg sitagliptin phosphate monohydrate equivalent to 100 mg of sitagliptin (STEGLUJAN 15 / 100 ) For the full list of excipients see Section 6.1 LIST OF EXCIPIENTS 3 PHARMACEUTICAL FORM STEGLUJAN 5 / 100 tablets are beige, almond-shaped, film-coated tablets debossed with “554” on one side and plain on the other side. -

Diabetes Treatment Suggested Treatment for Type II Diabetes
Diabetes Treatment Suggested Treatment for Type II Diabetes MONOTHERAPY METFORMIN (if no contraindications) EFFICACY: High HYPOGLYCEMIA RISK: Low WEIGHT: Neutral/Weight Loss CV EFFECT: Beneficial SIDE EFFECTS: GI/Lactic Acidosis COST: $ Check A1c in three months. If the patient is not at program target of < 8 percent, consider two-drug combination (choice dependent on the individual patient and disease-specific factors). IF PATIENT CAN'T TOLERATE/CONTRAINDICATION TO METFORMIN: GLP-1 or SGLT-2 Inhibitor (SGLT2i) + basal insulin Intolerance: Use extended release formulation. Take with food. Titrate dose slowly. Go back to prior tolerated dose if excessive side effects, GI side effects will generally lessen with time. Contraindication: Updated safety labeling says safe to use in patients with eGFR > 30 mL/min/1.73m^2 DRUG ORDER KEY: GREEN YELLOW RED = progression of most to least preferred DUAL THERAPY METFORMIN+ GLP-1 SGLT2i Basal Insulin DPP-IV Inhibitor Glitazone (TZD) EFFICACY: High Intermediate High Intermediate High HYPOGLYCEMIA RISK: Low Low High Low Low WEIGHT: Loss Loss Gain Neutral Gain CV EFFECT: Beneficial Beneficial Neutral May increase HF hospitalizations Potential HF worsening SIDE EFFECTS: GI Dehydration, Fracture, Genitouri- Hypoglycemia Rare Edema, Fracture nary Infections COST: $$$$ $$$ $$$ $$$ $ Check A1c in three months. If the patient is not at program target of < 8 percent, consider combinations below (choice dependent on the individual patient and disease-specific factors). PATIENT SCENARIO PREFERRED DRUG(S) NOTES Refuses to administer Avoid using insulin as a threat or sign of failure. Patient education is key. Discuss with patient injections that diabetes is a progressive disease and injection therapies are important for glycemic control, teach patient about proper injection techniques, self-monitoring of glucose, recognizing signs and symptoms of hypoglycemia and how to treat it. -

Overview of Ertugliflozin Vivianne K
CLINICAL PHARMACOLOGY UPDATE Overview of Ertugliflozin Vivianne K. Nguyen and John R. White, Jr. Introduction combinations with the DPP-4 sita- espite the availability of 12 gliptin (brand name Stegujan) or with different classes of medica- metformin (brand name Segluromet). Dtions, many people with type Ertugliflozin is not approved for the 2 diabetes struggle to maintain gly- treatment of type 1 diabetes, renal im- cemic control (1). Among the many pairment, or ketoacidosis. new antidiabetic medications to have Mechanism of Action emerged in recent years, sodium– As other SGLT2 inhibitors, ertug- glucose cotransporter 2 (SGLT2) liflozin works by blocking glucose inhibitors have proved to be a par- transport from the glomerular filtrate ticularly effective oral treatment for across the apical membrane of the these patients (2). Since the approval proximal epithelial cells, resulting in of the first drug in this class, canagli- increased urinary glucose excretion flozin, by the U.S. Food and Drug and reduced filtered glucose renal re- Administration (FDA) in March absorption. Ertugliflozin is predom- 2013, a total of four SGLT2 agents inantly metabolized by the enzymes have become available (both as single UGT1A9 and UGT2B, with minor and fixed-dose combination formu- contributions by CYP3A4, and even las) (1). In 2017, an estimated 1.7 less by CYP3A5 and CYP2C8 (4). million patients received a dispensed Ertugliflozin does not inhibit CYP450 prescription for an SGLT2 inhibitor isoenzymes (CYPs) 1A2, 2C9, 2C19, from U.S. outpatient retail pharmacies 2C8, 2B6, 2D6, or 3A4 and does not (2). Ertugliflozin is the newest agent induce CYPs 1A2, 2B6, or 3A4 (4). -

Growing Our Future in Diabetes Care: Where Are We Now and Where Are We Going?
GROWING OUR FUTURE IN DIABETES CARE: WHERE ARE WE NOW AND WHERE ARE WE GOING? Ashley Firm, Pharm.D. Lindsey Meston, Pharm.D. Disclosure Neither Dr. Firm nor Dr. Meston have anything to disclosure concerning possible financial or personal relationships with commercial entities (or their competitors) mentioned in this presentation. Objectives ■ Summarize key differences and updates to guidelines related to the care of diabetic patients, especially updates in the 2018 American Diabetes Association Standard of Medical Care in Diabetes ■ Select most appropriate treatment regimens for sample patients based on diabetic presentation and co-morbid conditions ■ Evaluate new products to the market for the treatment of diabetes, including place in therapy, pros and cons of use, major adverse effects, and other pertinent pharmacokinetic and pharmacodynamic properties. SOC-36238233 Socrative Join Code Which of the following correctly pairs a basal insulin and GLP1-RA coformulation? A. Insulin glargine- semaglutide B. Insulin determir- dulaglutide C. Insulin degludec- liraglutide Which new agent was accepted by the FDA for regulatory filing as a dual inhibitor of SGLT-2 in the treatment of type 1 diabetes? A. Sotagliflozin B. Empagliflozin C. Dapagliflozin D. Canagliflozin Under the ADA Standards of Care 2018, a patient with a history of a myocardial infarction would be recommended for which class of medication in addition to metformin? A. Thiazolidinediones B. Sulfonylureas C. Sodium Glucose Co-Transporter 2 Inhibitor D. Alpha Glucosidase Inhibitor Under the updated guidelines of the American Association of Clinical Endocrinologists, a patient failing to achieve A1C goal with metformin would be most appropriately treated with a medication from which class? A.