Bc Simulation Current State Report
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-
Open Session Meeting Agenda
Board of Governors Open Session Agenda Pkg - Nov. 24, 2020 Page 1 of 124 Board of Governors Open Session Meeting Agenda Tuesday, November 24, 2020 Meetings to be held via the Zoom Conference System (www.zoom.us) 9:00am-9:10am • To join the meeting, click HERE • Meeting ID: 650 5160 5949 • To join by phone dial: 1-778-907-2071 (Vancouver) and use meeting ID: 650 5160 5949# **please note that long distance charges may apply 10:35am-12:00pm • To join the meeting, click HERE • Meeting ID: 691 2777 3815 • To join by phone dial: 1-778-907-2071 (Vancouver) and use meeting ID: 691 2777 3815# **please note that long distance charges will apply We respectfully acknowledge that we are meeting on the unceded traditional lands of the Indigenous people who have inhabited and used the lands since time immemorial. Related Time Pages APPROVAL OF AGENDA Recommended Motion: 9:00am “BE IT RESOLVED THAT the November 24, 2020, Okanagan College Board of Governors Open session meeting agenda is approved.” INTRODUCTION OF NEW MEMBERS 9:05am OATH OF OFFICE DECLARATION OF CONFLICT CONSENT AGENDA 10:35am Recommended Motion: “BE IT RESOLVED THAT the Consent Agenda be approved as presented.” Previous Minutes – September 29, 2020 6-9 Written Reports 5.2.1. President’s Report (J. Hamilton) 10-11 Board of Governors Open Session Agenda Pkg - Nov. 24, 2020 Page 2 of 124 Related Time Pages Approvals 5.3.1. Board Observers Recommended Motion: “BE IT RESOLVED that the be following persons be appointed as Board Observers for a one-year term from November 24, 2020 to November 23, 2021: Sharon Mansiere, representing Okanagan College Faculty Association (OCFA), Cam McRobb, representing BCGEU Vocational Instructors, Paula Faragher, representing BCGEU Support Staff, Inga Wheeler, representing Okanagan College Admin. -
Change the World
change the world for the better / live on a healthy planet / do the most with your money, your ideas and your ideals / improve lives of people around the world / focus on your vision for change / make your mission a reality 2008 Annual Report From the President & CEO The following pages reduce the impacts of HIV/ feature stories of these AIDS, promote peace and Ross McMillan change makers – people disarmament, empower and organizations who are women and youth, and striving, with support from advance our vision of just Tides Canada, to address societies. intractable problems ranging from species Looking Forward extinction to poverty Ross McMillan Addressing the major reduction, from climate social and environmental change to sustainability in challenges of our time will the developing world. require a new response 2008: Mission- from the charitable sector: a smart, activist Minded Amid philanthropy capable of Economic Turmoil long-range thinking and Tides Canada has visionary leadership to link grown and matured 2008 was a year of continued growth and the aspirations of donors remarkably in eight impact amid global with concrete action and short years. economic uncertainty. outcomes. Conceived to fill a gap in Of course, Tides Canada Tides Canada is prepared Canadian philanthropy, and its donors were to lead this new mode Tides Canada initially not immune to the of philanthropy by focused on helping unparalleled correction in expanding our reach, progressive donors global financial markets. deepening our programs support smaller, Our investment portfolio and forging new innovative social justice fared materially better relationships. We will and environmental than market averages, but continue to help you charities. -

SCHEDULE B – RECOGNIZED PRACTICAL NURSING EDUCATION PROGRAMS (Sections 88, 91, 93) ______
SCHEDULE B – RECOGNIZED PRACTICAL NURSING EDUCATION PROGRAMS (Sections 88, 91, 93) ___________ Educational Institution Campus Program Type Camosun College Victoria Generic CDI College Richmond Generic CDI College Surrey Generic Coast Mountain College Terrace Access College of New Caledonia Burns Lake Generic College of New Caledonia Prince George Generic College of the Rockies Cranbrook Generic Discovery Community College Campbell River Generic & Access Discovery Community College Nanaimo Generic & Access Nicola Valley Institute of Technology Merritt Access North Island College Campbell River Generic North Island College Port Alberni Generic Northern Lights College Dawson Creek Generic Okanagan College Kelowna Generic Okanagan College Penticton Generic Okanagan College Salmon Arm Generic Okanagan College Vernon Generic Sprott Shaw College Abbotsford Generic Sprott Shaw College Downtown Vancouver Generic & Access Sprott Shaw College East Vancouver Generic & Access Educational Institution Campus Program Type Sprott Shaw College Kamloops Generic & Access Sprott Shaw College Kelowna Generic & Access Sprott Shaw College New Westminster Generic & Access Sprott Shaw College Penticton Generic & Access Sprott Shaw College Surrey Generic Sprott Shaw College Victoria Generic Stenberg College Surrey Generic Thompson Rivers University Williams Lake Generic University of the Fraser Valley Chilliwack Generic Vancouver Career College Abbotsford Generic Vancouver Career College Burnaby Generic Vancouver Community College Vancouver (Broadway) Generic & -

Assisted Living Residences List – by Community Last Update: July, 2015
Home and Community Care Assisted Living Residences Assisted Living Residences List – by Community Last Update: July, 2015 Community Site Name Address Owner / Northern Health Northern (# of publicly Operator Contact Health subsidized units) (Title) Telephone Burns Lake Tweedsmuir 53 9th Ave Lakes District Manager, Home & 250-692-2494 House Burns Lake BC Senior Citizens Community Care, (17 units) V0J 1E0 Housing Society Lakes District Chetwynd Surerus Place 5353 47th Ave Chetwynd Manager, 250-719-6510 (4 units) Chetwynd BC Senior Citizens Community Care, V0C 1J0 Housing Society South Peace Dawson Creek Northview 1125 90th Ave Dawson Creek Manager, 250-719-6510 (26 units) Dawson Creek BC Society for Community Care, V1G 5A3 Community South Peace Living Fort St. James Pioneer Place 200 School Rd Fort St James Manager, Home & 250-567-2013 (2 units) Fort St James BC Senior Citizens Community Care, Extn 6282 V0J 1P0 Housing Society Omineca District Fort St John Heritage 9824 106th Ave Northern Manager, 250-263-6025 Manor II Fort St John BC Health Community Care, (24 units) V1J 2N7 North Peace Hazelton Skeena Place 4780 Janze Way Wrinch Manager, Home & 250-847-6430 (6 units) Hazelton BC Memorial Community Care, V0J 1Y0 Foundation East Cluster Houston Cottonwood 2261 Copeland Smithers Manager, Home & 250-847-6430 Manor Ave Community Community Care, (5 units) Houston BC Services East Cluster V0J 1Z0 Association Kitimat Delta King 701 Mountainview Delta King Manager, Home & 250-632-8312 Place Square Place Housing Community Care, (15 units) Kitimat BC Society Central Cluster V8C 5G9 Masset Nick Grosse 2524 Harrison Rd Northern Coordinator 250-626-4735 AL Residences Masset BC Health (4 units) V0T 1M0 Prince George Laurier Manor 2175 9th Ave Northern Intake Liaison, 250-565-7443 (32 units) Prince George BC Health Community V2M 5E3 Services - PG For more information on accessing our Assisted Living program, contact your local Community Services Office. -

Development of a Hospitality Management Program, in the East Kootenay Region Of
1 Development of a Hospitality Management Program, in the East Kootenay Region of British Columbia (Canada), to Address the Employment Needs of the Region Abstract College of the Rockies (Canada), guided by its strategic initiatives, explored the potential of introducing a two-year Hospitality Management Diploma program in Invermere, British Columbia. After a successful feasibility study, the program was developed and introduced during the Spring semester of 2018. The program content is aligned with the provincial core curriculum for Hospitality Management and developed in collaboration with local Hospitality industry inputs. The distinctiveness of the program lies in its design and structure, focused on regional industry employment needs and includes a 500-hour Co-operative education semester to further enhance students’ employability skills and job-readiness for the Hospitality industry. Key words Industry Employability Partnership Collaboration Education Development 2 Introduction Job-ready graduates as well as filling employment gaps are essential focus areas and desired outcomes for tertiary education institutions. College of the Rockies (COTR), British Columbia (BC), Canada explored the local Hospitality industries’ needs to design an academic program to do just that. The Kootenay Regional Skills Training Plan (2013) indicates the demand for workers to increase from 78 560 in 2012 to 83 240 in 2020, thus predicting a 5.6% increase, as indicated in Figure 1.1 Kootenay Labour Demand and Supply Projections 2012 to 2020. The Kootenay Regional Skills Training Plan (2013) further reveals the shortage of qualified employees in the Tourism and Hospitality industries in the Kootenay region. The region, with an already shortfall of qualified employees, has a projected Tourism and Hospitality employee growth, potentially similar to the 1.6% estimated for the province as well as business development that support the claim of a desired increase of qualified employees. -

Northern First Nations Health and Wellness Plan
Northern First Nations Health and Wellness Plan Northern First Nations Health Partnership Committee Northern Health • Chief Operating Officer, Northeast: Betty Morris • Chief Operating Officer, Northwest: Penny Anguish • Chief Operating Officer, Northern Interior: Michael McMillan • Chief Medical Health Officer: Dr. David Bowering • Vice President, Clinical Programs and Chief Nursing Officer: Dr. Suzanne Johnston • Regional Director of Aboriginal Health: Agnes Snow • Vice President, Medicine: Dr. Ronald Chapman • Vice President, Aboriginal Health: Dr. Margo Greenwood Northern Regional Table • FNHC Northwest Political Representative: Charles Morven • Northwest Technical Representative: Health Director: Therese Hagan • Northwest Technical Representative: Health Director: Lauren Brown • FNHC North Central Political Representative: Warner Adam • North Central Technical Representative: Julia Morris • North Central Technical Representative: Health Director: Vern Tom • FNHC Northeast Political Representative: Tammy Watson • Northeast Technical Representative: Health Director: Colleen Totusek • Northeast Technical Representative: Corene Apsassin Ex Officio Members • Northern Health Authority CEO or Delegate • First Nations Health Authority CEO or Delegate Northern Regional Table secretariat provided by: • Regional Health Liaison FNHA (North Central/Northern Interior): Nicole Cross • Regional Health Liaison FNHA (Northwest): Brian Mairs Northern Health secretariat provided by: • Lead, Aboriginal Health Engagement & Integration: Victoria Stewart -
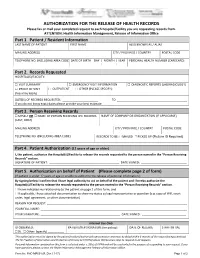
AUTHORIZATION for the RELEASE of HEALTH RECORDS Please Fax Or Mail Your Completed Request to Each Hospital/Facility You Are Requesting Records From
AUTHORIZATION FOR THE RELEASE OF HEALTH RECORDS Please fax or mail your completed request to each hospital/facility you are requesting records from. ATTENTION: Health Information Management, Release of Information Office Part 1. Patient / Resident Information LAST NAME OF PATIENT FIRST NAME ALSO KNOWN AS / ALIAS MAILING ADDRESS CITY / PROVINCE / COUNTRY POSTAL CODE TELEPHONE NO. (INCLUDING AREA CODE) DATE OF BIRTH DAY | MONTH | YEAR PERSONAL HEALTH NUMBER (CARECARD) | | Part 2. Records Requested HOSPITAL(S)/FACILITY: □ VISIT SUMMARY □ EMERGENCY VISIT INFORMATION □ DIAGNOSTIC REPORTS (LAB/RADIOLOGY) □ PROOF OF VISIT □ OUTPATIENT □ OTHER (PLEASE SPECIFY): (fees may apply) DATE(S) OF RECORDS REQUESTED: ______________________ TO ___________________________________________ If you do not know exact dates please provide your best estimate Part 3. Person Receiving Records □ MYSELF OR □ NAME OF PERSON RECEIVING THE RECORDS NAME OF COMPANY OR ORGANIZATION (IF APPLICABLE) (LAST, FIRST) MAILING ADDRESS CITY / PROVINCE / COUNTRY POSTAL CODE TELEPHONE NO. (INCLUDING AREA CODE) RECORDS TO BE: □ MAILED □ PICKED UP (Picture ID Required) Part 4. Patient Authorization (12 years of age or older) I, the patient, authorize the Hospital(s)/Facility to release the records requested to the person named in the “Person Receiving Records” section. SIGNATURE OF PATIENT: ___________________________________________ DATE SIGNED: ____________________________ Part 5. Authorization on behalf of Patient (Please complete page 2 of form) (If patient is under 12 years of age or unable to authorize the release of personal information.) By signing below I confirm that I have legal authority to act on behalf of the patient and I hereby authorize the Hospital(s)/Facility to release the records requested to the person named in the “Person Receiving Records” section. -

Camosun College Transportation and Parking Management Plan
Camosun College Transportation and Parking Management Plan By Todd Litman Victoria Transport Policy Institute 2009 Revised June, 2009 Camosun College Transportation and Parking Management Plan Victoria Transport Policy Institute Camosun College Transportation and Parking Management Plan 18 June 2009 By Todd Litman Victoria Transport Policy Institute Summary The Camosun College Transportation and Parking Management (TPM) Project includes a planning process to identify optimal solutions to campus transportation and parking problems. Through the TPM project, specific ways to improve transportation and parking management in order to create a more sustainable campus will be identified. The plan will be flexible and responsive to future demands and conditions. This TPM plan describes existing transportation and parking conditions, identifies current and future challenges, and recommends specific transportation and parking policies and management programs. The TPM Project will continue beyond this plan through the implementation phases. 2 Camosun College Transportation and Parking Management Plan Victoria Transport Policy Institute Contents Introduction .................................................................................................................................................... 5 Planning Goals and Objectives ....................................................................................................................... 5 Camosun College Campuses .......................................................................................................................... -
Mere Mortals W21 Programme 0.Pdf
The Douglas College Departments of Theatre and Stagecraft & Event Technology recognize and acknowledge the QayQayt (Kee-Kite) First Nation, as well as all Coast Salish Peoples, on whose traditional and unceded territories we live, learn, play, and do our work. further As an institution, Douglas College opposes all acts of racism and stands with Black, Indigenous and people of colour to actively combat systemic bias in our communities. The Departments of Theatre and Stagecraft & Event Technology present M E R E M O R T A L S a n d O t h e r s Plays by D A V I D I V E S March 16 - 18, 2021 Streaming Live from the Laura C. Muir Performing Arts Theatre Direction Kathleen Duborg Set Design Craig Alfredson Costume Design Alaia Hamer Lighting Design Gerald King The use of cameras or recording devices in the theatre is strictly prohibited. Please disengage all mobile phones and other devices that may interrupt the performance with light and sound. W E L C O M E T O T H E 2 0 2 0 / 2 0 2 1 S E A S O N “Nobody understands nothing no more.” Thus spake Christina Drayton, Katherine Hepburn’s character in 1967’s Guess Who’s Coming to Dinner, echoing the words of her black housekeeper of twenty-two years, Tillie (Isabelle Sanford), as the liberal family grappled with the reality of an interracial marriage. These words have been haunting me for the better part of a year and they have become my constant refrain. -
Infection Prevention and Control
Infection Prevention and Control Annual Report 2015 - 2016 Table of Contents Executive Summary ............................................................................................................... 3 Introduction .......................................................................................................................... 5 Education .............................................................................................................................. 9 Surveillance ......................................................................................................................... 11 Hand Hygiene Compliance .................................................................................................... 11 Clostridium difficile Infection (CDI) Incidence Rates ............................................................. 15 Methicillin-resistant Staphylococcus aureus (MRSA) Incidence Rates ................................. 16 Vancomycin-Resistant Enterococci (VRE) Incidence Rates ................................................... 18 Management of Carbapenemase Producing Organisms (CPO) ............................................ 19 Surgical Site Infection (SSI) Incidence Rates .......................................................................... 20 Outbreak Management ....................................................................................................... 24 Medical Device Reprocessing Department (MDRD) .............................................................. 26 Accreditation -

Pre-Hospital Triage and Transport Guidelines for Adult and Pediatric Major Trauma in British Columbia
2019 PROVINCIAL GUIDELINE Pre-hospital Triage and Transport Guidelines for Adult and Pediatric Major Trauma in British Columbia Trauma Services BC A service of the Provincial Health Services Authority Contents Foreword ..........................................................................................................................................................................................3 Introduction ....................................................................................................................................................................................4 Adult and Pediatric Pre-hospital Trauma Triage Guidelines – Principles .........................................................................5 Step One – Physiological ................................................................................................................................................... 6 Step Two – Anatomical ........................................................................................................................................................7 Step Three – Mechanism ................................................................................................................................................... 8 Step Four – Special Considerations .................................................................................................................................. 8 Pre-hospital Trauma Triage Standard – British Columbia .....................................................................................................9 -

BC's Faith-Based Postsecondary Institutions
Made In B.C. – Volume II A History of Postsecondary Education in British Columbia B.C.’s Faith-Based Postsecondary Institutions Bob Cowin Douglas College April 2009 The little paper that keeps growing I had a great deal of fun in 2007 using some of my professional development time to assemble a short history of public postsecondary education in British Columbia. My colleagues’ interest in the topic was greater than I had anticipated, encouraging me to write a more comprehensive report than I had planned. Interest was such that I found myself leading a small session in the autumn of 2008 for the BC Council of Post Secondary Library Directors, a group that I enjoyed meeting. A few days after the session, the director from Trinity Western University, Ted Goshulak, sent me a couple of books about TWU. I was pleased to receive them because I already suspected that another faith-based institution, Regent College in Vancouver, was perhaps BC’s most remarkable postsecondary success. Would Trinity Western’s story be equally fascinating? The short answer was yes. Now I was hooked. I wanted to know the stories of the other faith-based institutions, how they developed and where they fit in the province’s current postsecondary landscape. In the ensuing months, I poked around as time permitted on websites, searched library databases and catalogues, spoke with people, and circulated drafts for review. A surprisingly rich set of historical information was available. I have drawn heavily on this documentation, summarizing it to focus on organizations rather than on people in leadership roles.