Eatingforgp2ndeditio
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Report Includes Safer Choices for Parents, Manufacturers and Retailers Seeking Healthy Foods for Infants
NEW TESTS SHOW THE 6 TYPES OF BABY FOOD PARENTS SHOULD LIMIT - AND SAFER CHOICES What’s in my baby’s food? A national investigation finds 95 percent of baby foods tested contain toxic chemicals that lower babies’ IQ, including arsenic and lead Report includes safer choices for parents, manufacturers and retailers seeking healthy foods for infants IN PARTNERSHIP WITH Healthy Babies Bright Futures | Jane Houlihan, Research Director and Charlotte Brody, National Director | October 2019 IN PARTNERSHIP WITH ACKNOWLEDGEMENTS TABLE OF CONTENTS Authors: Jane Houlihan, MSCE, Research Director, and Charlotte Brody, RN, National Director, Healthy EXECUTIVE SUMMARY ...................................................................................1 Babies Bright Futures Promising signs of progress must accelerate to protect babies. ......................................................................1 Healthy Babies Bright Futures (HBBF) would like to thank Parents can make six safer baby food choices for 80 percent less toxic metal residue. .................................2 the following people and organizations for their support: Fifteen foods account for more than half of the risk .Rice-based foods top the list. .......................................3 A network of groups and individuals around the country made this study possible by purchasing Parents, baby food companies, farmers, and FDA all have a role cereals at their local stores: Alaska Community Action in measurably reducing babies’ exposures. .......................................................................................................3 -

A Review of Heavy Metal Concentration and Potential Health Implications of Beverages Consumed in Nigeria
toxics Review A Review of Heavy Metal Concentration and Potential Health Implications of Beverages Consumed in Nigeria Sylvester Chibueze Izah *, Iniobong Reuben Inyang, Tariwari C. N. Angaye and Ifeoma Peace Okowa Department of Biological Sciences, Faculty of Science, Niger Delta University, Wilberforce Island, Yenagoa P.M.B. 071, Bayelsa State, Nigeria; [email protected] (I.R.I.); [email protected] (T.C.N.A.); [email protected] (I.P.O.) * Correspondence: [email protected]; Tel.: +234-703-0192-466 Academic Editor: David Bellinger Received: 6 November 2016; Accepted: 18 December 2016; Published: 22 December 2016 Abstract: Beverages are consumed in Nigeria irrespective of age, sex, and socioeconomic status. Beverages may be alcoholic (wine, spirits, and beers) or non-alcoholic (soft drink, energy drinks, candies, chocolates, milks). Notwithstanding, most beverages are packed in cans, bottles, and plastics. This paper reviews the concentration of heavy metals from some commercially-packaged beverages consumed in Nigeria. The study found that heavy metal concentrations, including iron, mercury, tin, antimony, cadmium, zinc, copper, chromium, lead, and manganese, seldom exceed the maximum contaminant level recommended by the Standard Organization of Nigeria (SON) and the World Health Organization (WHO) as applicable to drinking water resources. The occurrence of heavy metals in the beverages could have resulted from the feedstocks and water used in their production. Consumption of beverages high in heavy metal could be toxic and cause adverse effect to human health, depending on the rate of exposure and accumulation dosage. This study concludes by suggesting that heavy metal concentration in the feedstocks and water should be monitored by producers, and its concentration in beverages should also be monitored by appropriate regulatory agencies. -

Buen Provecho!
www.oeko-tex.com International OEKO-TEX® Cookbook | Recipes from all over the world | 2012 what´scooking? mazaidar khanay ka shauk Guten Appetit! Trevlig måltid Buen provecho! Smacznego 尽享美食 Καλή σας όρεξη! Enjoy your meal! Dear OEKO-TEX® friends The OEKO-TEX® Standard 100 is celebrating its 20th anniversary this year. We would like to mark this occasion by saying thank you to all companies participating in the OEKO-TEX® system, and to their employees involved in the OEKO-TEX® product certification in their daily work. Without their personal commitment and close co-operation with our teams around the globe, the great success of the OEKO-TEX® Standard 100 would not have been possible. As a small gift the OEKO-TEX® teams from our worldwide member institutes and representative offices have created a self-made cooking book with favourite recipes which in some way has the same properties as the OEKO-TEX® Standard 100 that you are so familiar with – it is international, it can be used as a modular system and it illustrates the great variety of delicious food and drinks (just like the successfully tested textiles of all kinds). We hope that you will enjoy preparing the individual dishes. Set your creativity and your taste buds free! Should you come across any unusual ingredients or instructions, please feel free to call the OEKO-TEX® employees who will be happy to provide an explanation – following the motto “OEKO-TEX® unites and speaks Imprint the same language” (albeit sometimes with a local accent). Publisher: Design & Layout: Bon appetit! -

Value of Wholegrain Rice in a Healthy Human Nutrition
agriculture Review Value of Wholegrain Rice in a Healthy Human Nutrition Marina Carcea Research Centre on Food and Nutrition (CREA-AN), Council for Agricultural Research and Economics (CREA), Via Ardeatina, 546, 00178 Rome, Italy; [email protected]; Tel.: +39-06-5149-4429 Abstract: Rice is one of the most widely consumed cereals in the world. The husks of harvested, unprocessed rice are not digested by humans and need to be removed to obtain edible grains, whereas the bran can be partially (brown rice) or totally removed (white rice). Brown rice is a wholegrain cereal and, as such, is known to have beneficial effects on human health. Recent epidemiological studies have shown that the consumption of whole grains can reduce the risk of metabolic disorders, cardiovascular diseases, and some types of cancer. However, white rice is preferred for reasons connected to appearance, taste, palatability, ease of cooking, tradition, safety, shelf-life, and lack of awareness about its benefits and availability. In this review, the latest scientific reports regarding the nutritional composition of brown rice and the evolution of the technology for its production will be briefly reviewed together with research on nutritional implications of brown rice consumption also in relation to cancer development in humans. A specific chapter is devoted to pigmented rice which, thanks to its composition, has attracted the growing interest of consumers worldwide. The need for further studies to help promote the consumption of wholegrain rice are also discussed. Keywords: brown rice; nutritional quality; brown rice technology; pigmented rice; glycemic re- sponse; cancer Citation: Carcea, M. -

Gluten-Free Products Shopping List
GLUTEN-FREE PRODUCTS SHOPPING LIST The items on this shopping list, to the best of our knowledge, are made without gluten or any ingredients derived from gluten-containing grains, such as wheat, barley, rye, spelt or kamut. It is possible that products labeled gluten-free may come into contact with gluten during manufacturing. However, with the current FDA guidelines, any product labeled gluten-free should have less than 20 parts per million (ppm), which is considered a safe amount for most individuals following a gluten-free diet. People who have celiac disease and individuals who are exquisitely sensitive may still have a reaction to foods with measurable, although tiny, amounts of gluten. In this case, it is helpful to find companies that produce products in a dedicated gluten-free facility or that are part of a certification program. Products with this symbol are certified by the Gluten-Free Certification Organization, and tested for less than 10 ppm. For more information visit their webpage at www.gfco.org. This list also indicates whether the gluten-free foods listed contain dairy, soy or egg in the ingredients. If soy lecithin is the source of soy in the product, (SL) will appear after the product description. Visit our website at www.newseasonsmarket.com for a list of our regularly scheduled complimentary gluten- free products store tours. Please direct questions and comments regarding this list to [email protected]. Disclaimer: This is merely a guide and we are unable to be responsible for individual reactions to any product. Please read each label carefully to determine whether a food is appropriate for you. -
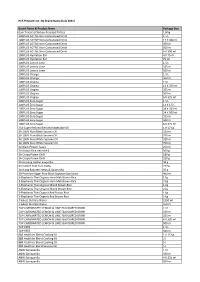
HCS Website List As of 30 June 2021 Working File.Xlsx
HCS Product List - By Brand Name (July 2021) Brand Name & Product Name Package Size (Lim Traders) Chicken Breaded Patties 1.8 kg 100PLUS ACTIVE Non-Carbonated Drink 1.5 L 100PLUS ACTIVE Non-Carbonated Drink 12 X 300 ml 100PLUS ACTIVE Non-Carbonated Drink 300 ml 100PLUS ACTIVE Non-Carbonated Drink 500 ml 100PLUS ACTIVE Non-Carbonated Drink 6 X 300 ml 100PLUS Hydration Bar 4 X 75 ml 100PLUS Hydration Bar 75 ml 100PLUS Lemon Lime 1.5 L 100PLUS Lemon Lime 325 ml 100PLUS Lemon Lime 500 ml 100PLUS Orange 1.5 L 100PLUS Orange 500 ml 100PLUS Original 1.5 L 100PLUS Original 12 X 325 ml 100PLUS Original 325 ml 100PLUS Original 500 ml 100PLUS Original 6 X 325 ml 100PLUS Zero Sugar 1.5 L 100PLUS Zero Sugar 12 X 1.5 L 100PLUS Zero Sugar 24 X 325 ml 100PLUS Zero Sugar 24 X 500 ml 100PLUS Zero Sugar 325 ml 100PLUS Zero Sugar 500 ml 100PLUS Zero Sugar 6 X 325 ml 333 Super Refined Blended Vegetable Oil 1 X 17 kg 3A 100% Pure Black Sesame Oil 320 ml 3A 100% Pure Black Sesame Oil 750 ml 3A 100% Pure White Sesame Oil 320 ml 3A 100% Pure White Sesame Oil 750 ml 3A Black Pepper Sauce 250 ml 3A Brown Rice Vermicelli 500 g 3A Crispy Prawn Chilli 180 g 3A Crispy Prawn Chilli 320 g 3A Ginseng Herbal Soup Mix 40 g 3A Instant Tom Yum Paste 227 g 3A Klang Bakuteh Herbs & Spices Mix 35 g 3A Premium Sugar Free Black Soybean Soy Sauce 400 ml 3-Elephants Thai Organic Hom Mali Brown Rice 1 kg 3-Elephants Thai Organic Hom Mali Brown Rice 2 kg 3-Elephants Thai Organic Mixed Brown Rice 1 kg 3-Elephants Thai Organic Mixed Brown Rice 2 kg 3-Elephants Thai Organic Red Brown -

Small Changes in the Beginning Breakfast
In the previous article, I listed foods that were most balancing to achieve a clean burning metabolism that burns fat and gives you energy to spare. Most of my patients are too busy to cook so they rely on quick meals like breakfast bars, sandwiches, and fast foods from the drive thru. When I introduce them to this new way of eating, most of them do not know where to begin. For some people, it is a huge overhaul of their dietary habits. Breaking old habits and creating a new way of choosing food takes time but it can be done. This article will show you how easy it is to begin eating food that is both balancing and nutritious. SMALL CHANGES IN THE BEGINNING Before instituting major changes in your diet, it is good to have a plan. Start with one item you want to eliminate from your diet then add others as you become successful at finding healthier alternatives. Pick one meal such as breakfast or lunch to begin making changes. Once that meal becomes easy, pick the next meal. Before you know it, you will be eating a diet that energizes you while providing long term benefits to your overall health. You will need to find a good health food store. Local to my patients is Kimberton Whole Foods in Downingtown, PA. They have the best selection of organic grains, beans, produce, and free range, grass fed meats and eggs. BREAKFAST Cereal and milk are popular breakfast items that are usually too high in simple carbohydrates and include cow’s milk. -

Ar .Cn .De .En .Es .Fr .Id .It .Ph .Po .Ru .Sw" class="text-overflow-clamp2"> Rice in Human Nutrition -… Home "" """"> Ar .Cn .De .En .Es .Fr .Id .It .Ph .Po .Ru .Sw
25/10/2011 Rice in human nutrition -… Home "" """"> ar .cn .de .en .es .fr .id .it .ph .po .ru .sw Chapter 3 - Grain structure, composition and consumers' criteria for quality Contents - Previous - Next The rice grain (rough rice or paddy) consists of an outer protective covering, the hull, and the rice caryopsis or fruit (brown, cargo, dehulled or dehusked rice), (Juliano and Bechtel, 1985), (Figure 2). Brown rice consists of the outer layers of pericarp, seed-coat and nucellus; the germ or embryo; and the endosperm. The endosperm consists of the aleurone layer and the endosperm proper, consisting of the subaleurone layer and the starchy or inner endosperm. The aleurone layer encloses the embryo. Pigment is confined to the pericarp (Juliano and Bechtel, 1985). The hull (husk) constitutes about 20 percent of the rough rice weight, but values range from 16 to 28 percent. The distribution of brown rice weight is pericarp 1 to 2 percent, aleurone plus nucellus and seed-coat 4 to 6 percent, germ 1 percent, D:/…/meister1024.htm 1/137 25/10/2011 Rice in human nutrition -… scutellum 2 percent and endosperm 90 to 91 percent (Juliano, 1972). The aleurone layer varies from one to five cell layers; it is thicker at the dorsal than at the ventral side and thicker in short-grain than in long-grain rices (del Rosario et al., 1968). The aleurone and embryo cells are rich in protein bodies, containing globoids or phytate bodies, and in lipid bodies (Tanaka et al., 1973; Tanaka, Ogawa and Kasai, 1977). The endosperm cells are thin-walled and packed with amyloplasts containing compound starch granules. -

Why White Rice Cereal for Babies Must Go
2011 White Paper: Why White Rice Cereal for Babies Must Go Alan Greene, M.D., F.A.A.P. Clinical Professor, Stanford University School of Medicine Introduction Evident even before children’s first birthdays, we are experiencing a true epidemic of childhood overweight and obesity in the United States today. This early onset heralds both great need and opportunity for achievable change. Meanwhile, the Institute of Medicine progress report on Preventing Childhood Obesity asserts that in school-aged children frank obesity has increased more than four- fold since 1971.i One out of three US children are already overweight or obese. This vexing and recalcitrant problem has serious present and future health implications. In the Framingham offspring cohort, 2/3 of high school students already exhibit one or more of the defining characteristics of metabolic syndrome (i.e., hypertension, dyslipidemia, abnormal glucose tolerance, or excessive abdominal girth).ii Moreover, by age 9, type 2 diabetes, previously so rare in teens or young adults as to have recently been called adult onset diabetes, has already overtaken type 1 diabetes (previously juvenile diabetes) in prevalence.iii The obesity epidemic provides clear, visible evidence that the way America’s children are fed is failing them. Moreover, that this wave of obesity is already present by 9 months of age suggests that how America’s babies have been fed in recent decades has been failing them as well. It’s difficult to imagine a successful, efficient solution to the obesity epidemic that doesn’t include a major change in infant feeding practices. For decades now, without adequate practical or scientific justification, white rice flour cereal has been the predominant food recommended by pediatricians across the United States for babies’ first solid food. -

Preparation and Quality Evaluation of Brown Rice and Khoa Incorporated Yamari
PREPARATION AND QUALITY EVALUATION OF BROWN RICE AND KHOA INCORPORATED YAMARI by Bijendra Lal Dangol Department of Food Technology Central Campus of Technology Institute of Science and Technology Tribhuvan University, Nepal 2018 Preparation and Quality Evaluation of Brown Rice and Khoa Incorporated Yamari A dissertation submitted to the Department of Food Technology, Central Campus of Technology, Tribhuvan University, in partial fulfillment of the requirements for the degree of B. Tech. in Food Technology by Bijendra Lal Dangol Department of Food Technology Central Campus of Technology Institute of Science and Technology Tribhuvan University, Nepal April, 2018 ii Tribhuvan University Institute of Science and Technology Department of Food Technology Central Campus of Technology, Dharan Approval Letter This dissertation entitled Preparation and Quality Evaluation of Brown Rice and Khoa Incorporated Yamari presented by Bijendra Lal Dangol has been accepted as the partial fulfillment of the requirements for the B. Tech. degree in Food Technology Dissertation committee 1. Chairperson __________________________ (Mr. Basanta K. Rai, Assoc. Prof.) 2. External Examiner __________________________ (Mr. Pramod Koirala, Chief, RFTQC) 3. Supervisor __________________________ (Mr. Navin Gautam, Asst. Prof.) 4. Internal Examiner __________________________ (Mr. Bunty Maskey, Asst. Prof.) April, 2018 iii Acknowledgement First of all, I would like to express my deep sense of gratitude to my respected supervisor Mr. Navin Gautam, Asst. Prof., Central Campus of Technology (CCT), Dharan for his valuable guidance, suggestion and encouragement throughout the work. I want to thank Prof. Dr. Dhan Bahadur Karki (Campus chief, CCT) for providing necessary facilities during the work. I am grateful to Assoc. Prof. Basanta Kumar Rai (HOD, Food Technology Department) for their valuable time and suggestion. -

Effects of Inorganic Arsenic in Infant Rice Cereal on Children's
Effects of Inorganic Arsenic in Infant Rice Cereal on Children’s Neurodevelopment December 7, 2017 Prepared for: Healthy Babies Bright Futures Submitted by: Andrea Chiger and Meghan T. Lynch Abt Associates 4550 Montgomery Avenue Suite 800 North Bethesda, MD 20814 CONTENTS Contents Contents .................................................................................................................................................. i Acronyms and Abbreviations ............................................................................................................. iii Executive Summary ............................................................................................................................. 1 Report Outline ...................................................................................................................................... 3 1. Background on Arsenic Sources and Health Effects ............................................................ 4 2. Standards for Inorganic Arsenic in Infant Rice Cereal ....................................................... 6 2.1 European Commission Standard ..................................................................................... 6 2.2 Proposed FDA Standard .................................................................................................. 7 3. Infant Rice Cereal Consumption, Arsenic Concentration, and Exposure Data ................ 8 3.1 Sources of Data on Arsenic Concentrations in Infant Food ............................................ 8 3.2 -

Reimbursable Foods in the Food Program
Reimbursable Foods in the Food Program Key: BR=Breakfast SN=Snack Category Food Item Food Item Food Item Meat / Alt Beef Beef Barbecue Beef Stix Pot Roast Beef Franks Beef Tips Roast Beef Beef Ground Braunschwieger Round Steak Beef Jerky Brisket Sausage - Beef Beef Liver Chuck Roast Stew Meat - Beef Beef Lunchmeat Corn Dog Veal Beef Meatballs Corned Beef Vienna Sausage Beef Ribs Meat Spread Chicken Chicken Breasts Chicken Legs Chicken Thighs Chicken Franks Chicken Liver Stew Meat - Chicken Chicken Gizzards Chicken Lunchmeat Whole Chicken Chicken Ground Chicken Nuggets / Stix Seafood Catfish Fish Fillets Shrimp Clams Fish Sticks Tuna Crab Salmon Pork Bratwurst Pork Chops Pork Roast Canadian Bacon Pork Ground Sausage - Pork Ham Pork Lunchmeat Spare Ribs Pepperoni Pork Meatballs Stew Meat – Pork Turkey Turkey Breast Turkey Ham Turkey Roast Turkey Franks Turkey Lunchmeat Whole Turkey Turkey Ground Turkey Meatballs Lamb Lamb Cheeses American Cheese Colby Cheese Pimento Cheese Cheddar Cheese Cottage Cheese Ricotta Cheese Cheese and Macaron (homemade)i Fried Cheese Sticks String Cheese (homemade) Lowfat Cheese Swiss Cheese Cheese Spread / Food Mozzarella Cheese Beans Baked Beans Great Northern Beans Pork & Beans Bean Soup Lima Beans Red / Kidney Beans Garbanzo Beans Navy Beans Refried Beans Chick Peas Pinto Beans Peas Black-eyed Peas Lentils Split Pea Soup Dried Green / Yellow Peas Eggs Egg, cooked Peanut Butter Peanut Butter (snack only) Peanut Butter & Meat / Alternate Yogurt Yogurt Seeds Pumpkin Seeds (snack only) Sesame Seeds (snack only)