Genetics in Epilepsy
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Epilepsy Syndromes E9 (1)
EPILEPSY SYNDROMES E9 (1) Epilepsy Syndromes Last updated: September 9, 2021 CLASSIFICATION .......................................................................................................................................... 2 LOCALIZATION-RELATED (FOCAL) EPILEPSY SYNDROMES ........................................................................ 3 TEMPORAL LOBE EPILEPSY (TLE) ............................................................................................................... 3 Epidemiology ......................................................................................................................................... 3 Etiology, Pathology ................................................................................................................................ 3 Clinical Features ..................................................................................................................................... 7 Diagnosis ................................................................................................................................................ 8 Treatment ............................................................................................................................................. 15 EXTRATEMPORAL NEOCORTICAL EPILEPSY ............................................................................................... 16 Etiology ................................................................................................................................................ 16 -
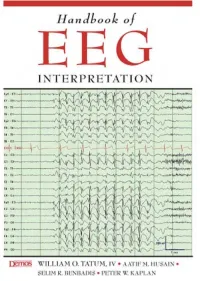
Handbook of EEG INTERPRETATION This Page Intentionally Left Blank Handbook of EEG INTERPRETATION
Handbook of EEG INTERPRETATION This page intentionally left blank Handbook of EEG INTERPRETATION William O. Tatum, IV, DO Section Chief, Department of Neurology, Tampa General Hospital Clinical Professor, Department of Neurology, University of South Florida Tampa, Florida Aatif M. Husain, MD Associate Professor, Department of Medicine (Neurology), Duke University Medical Center Director, Neurodiagnostic Center, Veterans Affairs Medical Center Durham, North Carolina Selim R. Benbadis, MD Director, Comprehensive Epilepsy Program, Tampa General Hospital Professor, Departments of Neurology and Neurosurgery, University of South Florida Tampa, Florida Peter W. Kaplan, MB, FRCP Director, Epilepsy and EEG, Johns Hopkins Bayview Medical Center Professor, Department of Neurology, Johns Hopkins University School of Medicine Baltimore, Maryland Acquisitions Editor: R. Craig Percy Developmental Editor: Richard Johnson Cover Designer: Steve Pisano Indexer: Joann Woy Compositor: Patricia Wallenburg Printer: Victor Graphics Visit our website at www.demosmedpub.com © 2008 Demos Medical Publishing, LLC. All rights reserved. This book is pro- tected by copyright. No part of it may be reproduced, stored in a retrieval sys- tem, or transmitted in any form or by any means, electronic, mechanical, photocopying, recording, or otherwise, without the prior written permission of the publisher. Library of Congress Cataloging-in-Publication Data Handbook of EEG interpretation / William O. Tatum IV ... [et al.]. p. ; cm. Includes bibliographical references and index. ISBN-13: 978-1-933864-11-2 (pbk. : alk. paper) ISBN-10: 1-933864-11-7 (pbk. : alk. paper) 1. Electroencephalography—Handbooks, manuals, etc. I. Tatum, William O. [DNLM: 1. Electroencephalography—methods—Handbooks. WL 39 H23657 2007] RC386.6.E43H36 2007 616.8'047547—dc22 2007022376 Medicine is an ever-changing science undergoing continual development. -

The Genetic Relationship Between Paroxysmal Movement Disorders and Epilepsy
Review article pISSN 2635-909X • eISSN 2635-9103 Ann Child Neurol 2020;28(3):76-87 https://doi.org/10.26815/acn.2020.00073 The Genetic Relationship between Paroxysmal Movement Disorders and Epilepsy Hyunji Ahn, MD, Tae-Sung Ko, MD Department of Pediatrics, Asan Medical Center Children’s Hospital, University of Ulsan College of Medicine, Seoul, Korea Received: May 1, 2020 Revised: May 12, 2020 Seizures and movement disorders both involve abnormal movements and are often difficult to Accepted: May 24, 2020 distinguish due to their overlapping phenomenology and possible etiological commonalities. Par- oxysmal movement disorders, which include three paroxysmal dyskinesia syndromes (paroxysmal Corresponding author: kinesigenic dyskinesia, paroxysmal non-kinesigenic dyskinesia, paroxysmal exercise-induced dys- Tae-Sung Ko, MD kinesia), hemiplegic migraine, and episodic ataxia, are important examples of conditions where Department of Pediatrics, Asan movement disorders and seizures overlap. Recently, many articles describing genes associated Medical Center Children’s Hospital, University of Ulsan College of with paroxysmal movement disorders and epilepsy have been published, providing much infor- Medicine, 88 Olympic-ro 43-gil, mation about their molecular pathology. In this review, we summarize the main genetic disorders Songpa-gu, Seoul 05505, Korea that results in co-occurrence of epilepsy and paroxysmal movement disorders, with a presenta- Tel: +82-2-3010-3390 tion of their genetic characteristics, suspected pathogenic mechanisms, and detailed descriptions Fax: +82-2-473-3725 of paroxysmal movement disorders and seizure types. E-mail: [email protected] Keywords: Dyskinesias; Movement disorders; Seizures; Epilepsy Introduction ies, and paroxysmal dyskinesias [3,4]. Paroxysmal dyskinesias are an important disease paradigm asso- Movement disorders often arise from the basal ganglia nuclei or ciated with overlapping movement disorders and seizures [5]. -
The Frequency of Seizures with Roseola. the Study Corroborates the Suggestion That Seizures with Roseola, HHV-6, and Fever Are Not Always Simple in Type
the frequency of seizures with roseola. The study corroborates the suggestion that seizures with roseola, HHV-6, and fever are not always simple in type. They are frequently prolonged, recurrent, and complex, and sometimes a manifestation of encephalitis or encephalopathy. (Progress in Pediatric Neurology II. Millichap JG, Ed, PNB Publ, 1994, pp 410, 415). These findings further weaken the hypothesis of the so-called simple febrile seizure as a distinct disease entity. For abstracts from the 16th annual conference on febrile convulsions held in Tokyo, Dec 18, 1993, see Fukuyama Y. Brain Dev July/Aug 1994;16:339-346. Papers included neurochemical aspects, EEG studies, and clinical, epidemiological, and treatment reports. The reputed safety and effectiveness of intermittent oral diazepam (0.4 mg/kg, 3 doses) at times of fever for prevention of recurrence of febrile seizures was supported in 23 children treated at Shimane Medical University and Central Hospital, Japan. GLUTAMATE IN PYRIDOXINE-DEPENDENT EPILEPSY Cerebrospinal fluid levels of glutamate, g-aminobutyric acid, and pyridoxal-5-phosphate examined in a patient with pyridoxine dependency while on and off vitamin B6 treatment are reported from Universitat Munchen, and Universitats-Nervenklinik, Wurzburg, Germany. Seizures began at age 3 weeks. Despite phenobarbital, status epilepticus occurred at 3 months and was followed by infantile spasms and hypsarrhythmia. The addition of ACTH and vitamin B6 controlled the seizures and the EEG became normal. Seizures recurred on each of several occasions when vitamin B6 was withdrawn. CSF glutamate was elevated 200-fold, whereas GABA and PLP were normal. After vitamin B6 (5 mg/kg BW/day) was reintroduced, seizures stopped and the EEG was normal, but CSF glutamate was still elevated 10 fold. -

Psychogenic Seizurespsychogenicseizures
PsychogenicPsychogenicSeizuresSeizures MMaartrtiinnSaSalliinsnskykyMM..DD.. PoPortrtllaandndVVAAMMCCEEpipillepsyepsyCCententererooffEExxcecellllenceence OreOreggoonnHeaHealltthh&&SciScienceenceUUninivverersisittyy …You’d better ask the doctors here about my illness, sir. Ask them whether my fit was real or not. TTheheBBrrootthershersKaKararamamazzoovv;;FF..DDooststooevevskskyy,,11888811 Psychogenic Seizures Psychogenic seizures (PNES) PNES in Veterans Treatment and Prognosis *excluding headache, back pain Epilepsy Cases per 100 persons 0.2 0.4 0.6 0.8 1.2 1.4 neurologists worldwide* The most common problem faced by 0 1 Epilepsy Neuropathy Cerebrovascular Dementia ~1% of the world burden of disease (WHO) Prevalence (per 100 persons) Murray et al; WHO, 1994Singhai; Arch Neurol 1998 Kobau; MMR, August Medina; 2008 J Neurol Sci 2007 Speaec 08%Sprevalence ~0.85% US prevalence ~0.85%US Disorders that may mimic epilepsy (adults) Cardiovascular events (syncope) » Vasovagal attacks (vasodepressor syncope) » Arrhythmias (Stokes-Adams attacks) Movement disorders » Paroxysmal choreoathetosis » Myoclonus, tics, habit spasms Migraine - confusional, basilar Sleep disorders (parasomnias) Metabolic disorders (hypoglycemia) Psychological disorders » Psychogenic seizures Non-Epileptic Seizures (NES) A transient alteration in behavior resembling an epileptic seizure but not due to paroxysmal neuronal discharges; –Psychogenic Seizures (PNES) without other physiologic abnormalities with probable psychological origin Non-Epileptic Seizures (NES) Seizures Epileptic -

ILAE Classification and Definition of Epilepsy Syndromes with Onset in Childhood: Position Paper by the ILAE Task Force on Nosology and Definitions
ILAE Classification and Definition of Epilepsy Syndromes with Onset in Childhood: Position Paper by the ILAE Task Force on Nosology and Definitions N Specchio1, EC Wirrell2*, IE Scheffer3, R Nabbout4, K Riney5, P Samia6, SM Zuberi7, JM Wilmshurst8, E Yozawitz9, R Pressler10, E Hirsch11, S Wiebe12, JH Cross13, P Tinuper14, S Auvin15 1. Rare and Complex Epilepsy Unit, Department of Neuroscience, Bambino Gesu’ Children’s Hospital, IRCCS, Member of European Reference Network EpiCARE, Rome, Italy 2. Divisions of Child and Adolescent Neurology and Epilepsy, Department of Neurology, Mayo Clinic, Rochester MN, USA. 3. University of Melbourne, Austin Health and Royal Children’s Hospital, Florey Institute, Murdoch Children’s Research Institute, Melbourne, Australia. 4. Reference Centre for Rare Epilepsies, Department of Pediatric Neurology, Necker–Enfants Malades Hospital, APHP, Member of European Reference Network EpiCARE, Institut Imagine, INSERM, UMR 1163, Université de Paris, Paris, France. 5. Neurosciences Unit, Queensland Children's Hospital, South Brisbane, Queensland, Australia. Faculty of Medicine, University of Queensland, Queensland, Australia. 6. Department of Paediatrics and Child Health, Aga Khan University, East Africa. 7. Paediatric Neurosciences Research Group, Royal Hospital for Children & Institute of Health & Wellbeing, University of Glasgow, Member of European Refence Network EpiCARE, Glasgow, UK. 8. Department of Paediatric Neurology, Red Cross War Memorial Children’s Hospital, Neuroscience Institute, University of Cape Town, South Africa. 9. Isabelle Rapin Division of Child Neurology of the Saul R Korey Department of Neurology, Montefiore Medical Center, Bronx, NY USA. 10. Programme of Developmental Neurosciences, UCL NIHR BRC Great Ormond Street Institute of Child Health, Department of Clinical Neurophysiology, Great Ormond Street Hospital for Children, London, UK 11. -

Febrile Seizures: Clinical Practice Guideline for the Long-Term Management of the Child with Simple Febrile Seizures
CLINICAL PRACTICE GUIDELINE Febrile Seizures: Clinical Practice Guideline for the Long-term Management of the Child With Simple Febrile Seizures Steering Committee on Quality Improvement and Management, Subcommittee on Febrile Seizures ABSTRACT Febrile seizures are the most common seizure disorder in childhood, affecting 2% to 5% of children between the ages of 6 and 60 months. Simple febrile seizures are www.pediatrics.org/cgi/doi/10.1542/ peds.2008-0939 defined as brief (Ͻ15-minute) generalized seizures that occur once during a 24-hour period in a febrile child who does not have an intracranial infection, doi:10.1542/peds.2008-0939 metabolic disturbance, or history of afebrile seizures. This guideline (a revision of All clinical reports from the American Academy of Pediatrics automatically expire the 1999 American Academy of Pediatrics practice parameter [now termed clinical 5 years after publication unless reaffirmed, practice guideline] “The Long-term Treatment of the Child With Simple Febrile revised, or retired at or before that time. Seizures”) addresses the risks and benefits of both continuous and intermittent The guidance in this report does not anticonvulsant therapy as well as the use of antipyretics in children with simple indicate an exclusive course of treatment febrile seizures. It is designed to assist pediatricians by providing an analytic or serve as a standard of medical care. Variations, taking into account individual framework for decisions regarding possible therapeutic interventions in this pa- circumstances, may be appropriate. tient population. It is not intended to replace clinical judgment or to establish a Key Word protocol for all patients with this disorder. -

Mesial Frontal Epilepsy
Epikpsia, 39(Suppl. 4):S49-S61. 1998 Lippincon-Raven Publishers, Philadelphia 0 International League Against Epilepsy Mesial Frontal Epilepsy Norman K. So Oregon Comprehensive Epilepsy Program, Legacy Portland Hospitals, Portland, Oregon, U.S.A. Summary: The mesiofrontal cortex comprises a number of occur. The task of localization of the epileptogenic zone can be distinct anatomic and functional areas. Structural lesions and challenging, whether EEG or imaging methods are used. Suc- cortical dysgenesis are recognized causes of mesial frontal epi- cessful localization can lead to a rewarding outcome after epi- lepsy, but a specific gene defect may also be important, as seen lepsy surgery, particularly in those with an imaged lesion. in some forms of familial frontal lobe epilepsy. The predomi- Key Words: Mesial frontal epilepsy-cingulate gyrus- nant seizure manifestations, which are not necessarily strictly Supplementary motor area-Absence seizure-Hypermotor correlated with a specific ictal onset zone, are absence, hyper- seizure-Postural tonic seizure-Epilepsy surgery. motor, and postural tonic seizures. Other seizure types also FUNCTIONAL ANATOMY convolution. Traditional cytoarchitectonics have further subdivided this anterior frontal region. The frontal pole The frontal lobe is the largest lobe in the brain, ac- refers to the anterior most portion of the frontal lobe, but counting for one-third to one-half of total brain volume there is little consensus on how far back this extends. and weight. On the medial surface, the most important One or more curved.sulci are seen anterior and inferior to landmark is the cingulate sulcus (Fig. 1). This runs as an the cingulate sulcus, called the superior and inferior ros- inverted “C” following the contour of the corpus callo- tral sulci. -

Chloride Channelopathies Rosa Planells-Cases, Thomas J
Chloride channelopathies Rosa Planells-Cases, Thomas J. Jentsch To cite this version: Rosa Planells-Cases, Thomas J. Jentsch. Chloride channelopathies. Biochimica et Biophysica Acta - Molecular Basis of Disease, Elsevier, 2009, 1792 (3), pp.173. 10.1016/j.bbadis.2009.02.002. hal- 00501604 HAL Id: hal-00501604 https://hal.archives-ouvertes.fr/hal-00501604 Submitted on 12 Jul 2010 HAL is a multi-disciplinary open access L’archive ouverte pluridisciplinaire HAL, est archive for the deposit and dissemination of sci- destinée au dépôt et à la diffusion de documents entific research documents, whether they are pub- scientifiques de niveau recherche, publiés ou non, lished or not. The documents may come from émanant des établissements d’enseignement et de teaching and research institutions in France or recherche français ou étrangers, des laboratoires abroad, or from public or private research centers. publics ou privés. ÔØ ÅÒÙ×Ö ÔØ Chloride channelopathies Rosa Planells-Cases, Thomas J. Jentsch PII: S0925-4439(09)00036-2 DOI: doi:10.1016/j.bbadis.2009.02.002 Reference: BBADIS 62931 To appear in: BBA - Molecular Basis of Disease Received date: 23 December 2008 Revised date: 1 February 2009 Accepted date: 3 February 2009 Please cite this article as: Rosa Planells-Cases, Thomas J. Jentsch, Chloride chan- nelopathies, BBA - Molecular Basis of Disease (2009), doi:10.1016/j.bbadis.2009.02.002 This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final form. -

Treatment for Patients with Lennox-Gastaut Syndrome Roundtable
Treatment for Patients with Lennox-Gastaut Syndrome Roundtable Video 3/5 – Diagnosis, Issues and Seizures Dr. Randa Jarrar Pediatric Epileptologist at Phoenix Children's Hospital Given the poor prognosis of Lennox-Gastaut Syndrome with regards to seizure control and cognitive outcome, it is very important to apply that term with caution. How do we go about diagnosing it and what kind of investigations do we have to do once we diagnosis it? Well, the diagnosis really relies on that classic triad of many seizure types, mental retardation, and the classic EEG features that we just went over, mainly the slow spike in wave. Some people consider the presence of ten-hertz fast activity as an essential for diagnosis. This can be either associated with atonic seizures or can occur with minimal clinical manifestations, such as apnea or perhaps truncal rigidity, that can be seen mainly during non-REM sleep. As we said, the diagnosis relies heavily on the EEG. Although it sounds easy to diagnosis since you have all these features, the features may not be very clear early at onset. Why? The cause, the history, the seizure types, the EEG features, are not pathognomonic for Lennox-Gastaut Syndrome. They are shared by other epilepsy syndromes and can occur in other seizure types. In addition, the core seizure types may not be present at onset. You can initially have focal seizure or the patient may present with myoclonic seizures, which can complicate the picture. The EEG features we talked about extensively, but I just want to emphasize that a sleep recording is almost essential, not just a sleep recording, but a video sleep recording. -

Epileptic Spasms Are a Feature of DEPDC5 Mtoropathy
Epileptic spasms are a feature of DEPDC5 mTORopathy Gemma L. Carvill, PhD ABSTRACT Douglas E. Crompton, Objective: To assess the presence of DEPDC5 mutations in a cohort of patients with epileptic PhD, MBBS spasms. Brigid M. Regan, BSc Methods: We performed DEPDC5 resequencing in 130 patients with spasms, segregation anal- (Hons) ysis of variants of interest, and detailed clinical assessment of patients with possibly and likely Jacinta M. McMahon, pathogenic variants. BSc (Hons) DEPDC5 Julia Saykally Results: We identified 3 patients with variants in in the cohort of 130 patients with DEPDC5 Matthew Zemel, BS spasms. We also describe 3 additional patients with alterations and epileptic spasms: 2 Amy L. Schneider, MGen from a previously described family and a third ascertained by clinical testing. Overall, we describe DEPDC5 Couns 6 patients from 5 families with spasms and variants; 2 arose de novo and 3 were Leanne Dibbens, PhD familial. Two individuals had focal cortical dysplasia. Clinical outcome was highly variable. Katherine B. Howell, Conclusions: While recent molecular findings in epileptic spasms emphasize the contribution of de MBBS (Hons), novo mutations, we highlight the relevance of inherited mutations in the setting of a family history BMedSc of focal epilepsies. We also illustrate the utility of clinical diagnostic testing and detailed pheno- Simone Mandelstam, typic evaluation in characterizing the constellation of phenotypes associated with DEPDC5 alter- MBChB ations. We expand this phenotypic spectrum to include epileptic spasms, aligning DEPDC5 Richard J. Leventer, epilepsies more with the recognized features of other mTORopathies. Neurol Genet 2015;1:e17; MBBS, PhD doi: 10.1212/NXG.0000000000000016 A. -

Role of Antineuronal Antibodies in Children with Encephalopathy and Febrile Status Epilepticus
View metadata, citation and similar papers at core.ac.uk brought to you by CORE provided by Elsevier - Publisher Connector Pediatrics and Neonatology (2014) 55, 161e167 Available online at www.sciencedirect.com ScienceDirect journal homepage: http://www.pediatr-neonatol.com REVIEW ARTICLE Role of Antineuronal Antibodies in Children with Encephalopathy and Febrile Status Epilepticus Kuang-Lin Lin, Huei-Shyong Wang* Division of Pediatric Neurology, Chang Gung Children’s Hospital and Chang Gung Memorial Hospital, Chang Gung University College of Medicine, Taoyuan, Taiwan Received Mar 11, 2013; received in revised form Jul 3, 2013; accepted Jul 16, 2013 Available online 16 September 2013 Key Words Status epilepticus in childhood is more common, with a different range of causes and a lower status epilepticus; risk of death, than convulsive status epilepticus in adults. Acute central nervous system infec- childhood; tions appear to be markers for morbidity and mortality. Nevertheless, central nervous infec- encephalitis; tion is usually presumed in these conditions. Many aspects of the pathogenesis of acute antineuronal encephalitis and acute febrile encephalopathy with status epilepticus have been clarified in antibodies the past decade. The pathogenesis is divided into direct pathogens invasion or immune- mediated mechanisms. Over the past few decades, the number of antineuronal antibodies to ion channels, receptors, and other synaptic proteins described in association with central nervous system disorders has increased dramatically, especially