MAGI2 Mutations Cause Congenital Nephrotic Syndrome
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Genome Wide Association Study of Response to Interval and Continuous Exercise Training: the Predict‑HIIT Study Camilla J
Williams et al. J Biomed Sci (2021) 28:37 https://doi.org/10.1186/s12929-021-00733-7 RESEARCH Open Access Genome wide association study of response to interval and continuous exercise training: the Predict-HIIT study Camilla J. Williams1†, Zhixiu Li2†, Nicholas Harvey3,4†, Rodney A. Lea4, Brendon J. Gurd5, Jacob T. Bonafglia5, Ioannis Papadimitriou6, Macsue Jacques6, Ilaria Croci1,7,20, Dorthe Stensvold7, Ulrik Wislof1,7, Jenna L. Taylor1, Trishan Gajanand1, Emily R. Cox1, Joyce S. Ramos1,8, Robert G. Fassett1, Jonathan P. Little9, Monique E. Francois9, Christopher M. Hearon Jr10, Satyam Sarma10, Sylvan L. J. E. Janssen10,11, Emeline M. Van Craenenbroeck12, Paul Beckers12, Véronique A. Cornelissen13, Erin J. Howden14, Shelley E. Keating1, Xu Yan6,15, David J. Bishop6,16, Anja Bye7,17, Larisa M. Haupt4, Lyn R. Grifths4, Kevin J. Ashton3, Matthew A. Brown18, Luciana Torquati19, Nir Eynon6 and Jef S. Coombes1* Abstract Background: Low cardiorespiratory ftness (V̇O2peak) is highly associated with chronic disease and mortality from all causes. Whilst exercise training is recommended in health guidelines to improve V̇O2peak, there is considerable inter-individual variability in the V̇O2peak response to the same dose of exercise. Understanding how genetic factors contribute to V̇O2peak training response may improve personalisation of exercise programs. The aim of this study was to identify genetic variants that are associated with the magnitude of V̇O2peak response following exercise training. Methods: Participant change in objectively measured V̇O2peak from 18 diferent interventions was obtained from a multi-centre study (Predict-HIIT). A genome-wide association study was completed (n 507), and a polygenic predictor score (PPS) was developed using alleles from single nucleotide polymorphisms= (SNPs) signifcantly associ- –5 ated (P < 1 10 ) with the magnitude of V̇O2peak response. -

Circular RNA Hsa Circ 0005114‑Mir‑142‑3P/Mir‑590‑5P‑ Adenomatous
ONCOLOGY LETTERS 21: 58, 2021 Circular RNA hsa_circ_0005114‑miR‑142‑3p/miR‑590‑5p‑ adenomatous polyposis coli protein axis as a potential target for treatment of glioma BO WEI1*, LE WANG2* and JINGWEI ZHAO1 1Department of Neurosurgery, China‑Japan Union Hospital of Jilin University, Changchun, Jilin 130033; 2Department of Ophthalmology, The First Hospital of Jilin University, Jilin University, Changchun, Jilin 130021, P.R. China Received September 12, 2019; Accepted October 22, 2020 DOI: 10.3892/ol.2020.12320 Abstract. Glioma is the most common type of brain tumor APC expression with a good overall survival rate. UALCAN and is associated with a high mortality rate. Despite recent analysis using TCGA data of glioblastoma multiforme and the advances in treatment options, the overall prognosis in patients GSE25632 and GSE103229 microarray datasets showed that with glioma remains poor. Studies have suggested that circular hsa‑miR‑142‑3p/hsa‑miR‑590‑5p was upregulated and APC (circ)RNAs serve important roles in the development and was downregulated. Thus, hsa‑miR‑142‑3p/hsa‑miR‑590‑5p‑ progression of glioma and may have potential as therapeutic APC‑related circ/ceRNA axes may be important in glioma, targets. However, the expression profiles of circRNAs and their and hsa_circ_0005114 interacted with both of these miRNAs. functions in glioma have rarely been studied. The present study Functional analysis showed that hsa_circ_0005114 was aimed to screen differentially expressed circRNAs (DECs) involved in insulin secretion, while APC was associated with between glioma and normal brain tissues using sequencing the Wnt signaling pathway. In conclusion, hsa_circ_0005114‑ data collected from the Gene Expression Omnibus database miR‑142‑3p/miR‑590‑5p‑APC ceRNA axes may be potential (GSE86202 and GSE92322 datasets) and explain their mecha‑ targets for the treatment of glioma. -

The Landscape of Genomic Imprinting Across Diverse Adult Human Tissues
Downloaded from genome.cshlp.org on September 30, 2021 - Published by Cold Spring Harbor Laboratory Press Research The landscape of genomic imprinting across diverse adult human tissues Yael Baran,1 Meena Subramaniam,2 Anne Biton,2 Taru Tukiainen,3,4 Emily K. Tsang,5,6 Manuel A. Rivas,7 Matti Pirinen,8 Maria Gutierrez-Arcelus,9 Kevin S. Smith,5,10 Kim R. Kukurba,5,10 Rui Zhang,10 Celeste Eng,2 Dara G. Torgerson,2 Cydney Urbanek,11 the GTEx Consortium, Jin Billy Li,10 Jose R. Rodriguez-Santana,12 Esteban G. Burchard,2,13 Max A. Seibold,11,14,15 Daniel G. MacArthur,3,4,16 Stephen B. Montgomery,5,10 Noah A. Zaitlen,2,19 and Tuuli Lappalainen17,18,19 1The Blavatnik School of Computer Science, Tel-Aviv University, Tel Aviv 69978, Israel; 2Department of Medicine, University of California San Francisco, San Francisco, California 94158, USA; 3Analytic and Translational Genetics Unit, Massachusetts General Hospital, Boston, Massachusetts 02114, USA; 4Program in Medical and Population Genetics, Broad Institute of Harvard and MIT, Cambridge, Massachusetts 02142, USA; 5Department of Pathology, Stanford University, Stanford, California 94305, USA; 6Biomedical Informatics Program, Stanford University, Stanford, California 94305, USA; 7Wellcome Trust Center for Human Genetics, Nuffield Department of Clinical Medicine, University of Oxford, Oxford, OX3 7BN, United Kingdom; 8Institute for Molecular Medicine Finland, University of Helsinki, 00014 Helsinki, Finland; 9Department of Genetic Medicine and Development, University of Geneva, 1211 Geneva, Switzerland; -

MAGI2 Gene Region and Celiac Disease
ORIGINAL RESEARCH published: 19 December 2019 doi: 10.3389/fnut.2019.00187 MAGI2 Gene Region and Celiac Disease Amaia Jauregi-Miguel 1, Izortze Santin 2,3, Koldo Garcia-Etxebarria 1, Ane Olazagoitia-Garmendia 1, Irati Romero-Garmendia 1, Maialen Sebastian-delaCruz 1, Iñaki Irastorza 4, Spanish Consortium for the Genetics of Celiac Disease, Ainara Castellanos-Rubio 1,5* and Jose Ramón Bilbao 1,3* 1 Department of Genetics, Physical Anthropology and Animal Physiology, Biocruces-Bizkaia Health Research Institute, University of the Basque Country (Universidad del País Vasco/Euskal Herriko Unibertsitatea), Leioa, Spain, 2 Department of Biochemistry and Molecular Biology, Biocruces-Bizkaia Health Research Institute, University of the Basque Country (Universidad del País Vasco/Euskal Herriko Unibertsitatea), Leioa, Spain, 3 CIBER in Diabetes and Associated Metabolic Diseases, Madrid, Spain, 4 Department of Pediatrics, Biocruces-Bizkaia Health Research Institute, Cruces University Hospital, University of the Basque Country (Universidad del País Vasco/Euskal Herriko Unibertsitatea), Barakaldo, Spain, 5 Ikerbasque, Basque Foundation for Science, Bilbao, Spain Edited by: Carmen Gianfrani, Institute of Biochemistry and Cell Celiac disease (CD) patients present a loss of intestinal barrier function due to structural Biology (CNR), Italy alterations in the tight junction (TJ) network, the most apical unions between epithelial Reviewed by: cells. The association of TJ-related gene variants points to an implication of this network Yanfei Zhang, Geisinger Health System, in disease susceptibility. This work aims to characterize the functional implication of United States TJ-related, disease-associated loci in CD pathogenesis. We performed an association Xiaofei Sun, study of 8 TJ-related gene variants in a cohort of 270 CD and 91 non-CD controls. -

MAGI2 Mutations Cause Congenital Nephrotic Syndrome
CLINICAL RESEARCH www.jasn.org MAGI2 Mutations Cause Congenital Nephrotic Syndrome † ‡ Agnieszka Bierzynska,* Katrina Soderquest, Philip Dean, Elizabeth Colby,* Ruth Rollason,* | Caroline Jones,§ Carol D. Inward,* Hugh J. McCarthy,* Michael A. Simpson, † ‡ † Graham M. Lord, Maggie Williams, Gavin I. Welsh,* Ania B. Koziell, and Moin A. Saleem* on behalf of NephroS, the UK study of Nephrotic Syndrome *Bristol Renal and Children’s Renal Unit, School of Clinical Sciences, University of Bristol, Bristol, United Kingdom; †Division of Transplantation Immunology and Mucosal Biology, Department of Experimental Immunobiology, and |Division of Genetics and Molecular Medicine, Faculty of Life Sciences and Medicine, King’s College London, London, United Kingdom; ‡Bristol Genetics Laboratory, North Bristol National Health Service Trust, Bristol, United Kingdom; and §Alder Hey Children’s Hospital, Liverpool, United Kingdom ABSTRACT Steroid–resistant nephrotic syndrome (SRNS), a heterogeneous disorder of the renal glomerular filtration barrier, results in impairment of glomerular permselectivity. Inheritance of genetic SRNS may be autosomal dominant or recessive, with a subset of autosomal recessive SRNS presenting as congenital nephrotic syn- drome (CNS). Mutations in 53 genes are associated with human SRNS, but these mutations explain #30% of patients with hereditary cases and only 20% of patients with sporadic cases. The proteins encoded by these genes are expressed in podocytes, and malfunction of these proteins leads to a universal end point of podocyte injury, glomerular filtration barrier disruption, and SRNS. Here, we identified novel disease–causing mutations in membrane–associated guanylate kinase, WW, and PDZ domain–containing 2 (MAGI2)through whole-exome sequencing of a deeply phenotyped cohort of patients with congenital, childhood–onset SRNS. -

Genomic Rearrangements of the 7Q11-21 Region
GENOMIC REARRANGEMENTS IN HUMAN AND MOUSE AND THEIR CONTRIBUTION TO THE WILLIAMS-BEUREN SYNDROME PHENOTYPE. by Edwin James Young A thesis submitted in conformity with the requirements for the degree of Doctor of Philosophy, Institute of Medical Science University of Toronto © Copyright by Edwin James Young (2010) Genomic rearrangements in human and mouse and their contribution to the Williams- Beuren Syndrome phenotype. Doctor of Philosophy (2010) Edwin James Young Institute of Medical Science University of Toronto Abstract: Genomic rearrangements, particularly deletions and duplications, are known to cause many genetic disorders. The chromosome 7q11.23 region in humans is prone to recurrent chromosomal rearrangement, due to the presence of low copy repeats that promote non-allelic homologous recombination. The most well characterized rearrangement of 7q11.23 is a hemizygous 1.5 million base pair (Mb) deletion spanning more than 25 genes. This deletion causes Williams-Beuren Syndrome (WBS; OMIM 194050), a multisystem developmental disorder with distinctive physical and behavioural features. Other rearrangements of the region lead to phenotypes distinct from that of WBS. Here we describe the first individual identified with duplication of the same 1.5 Mb region, resulting in severe impairment of expressive language, in striking contrast to people with WBS who have relatively well preserved language skills. We also describe the identification of a new gene for a severe form of childhood epilepsy through the analysis of individuals with deletions on ii chromosome 7 that extend beyond the boundaries typical for WBS. This gene, MAGI2, is part of the large protein scaffold at the post-synaptic membrane and provides a new avenue of research into both the molecular basis of infantile spasms and the development of effective therapies. -

Perkinelmer Genomics to Request the Saliva Swab Collection Kit for Patients That Cannot Provide a Blood Sample As Whole Blood Is the Preferred Sample
Autism and Intellectual Disability TRIO Panel Test Code TR002 Test Summary This test analyzes 2429 genes that have been associated with Autism and Intellectual Disability and/or disorders associated with Autism and Intellectual Disability with the analysis being performed as a TRIO Turn-Around-Time (TAT)* 3 - 5 weeks Acceptable Sample Types Whole Blood (EDTA) (Preferred sample type) DNA, Isolated Dried Blood Spots Saliva Acceptable Billing Types Self (patient) Payment Institutional Billing Commercial Insurance Indications for Testing Comprehensive test for patients with intellectual disability or global developmental delays (Moeschler et al 2014 PMID: 25157020). Comprehensive test for individuals with multiple congenital anomalies (Miller et al. 2010 PMID 20466091). Patients with autism/autism spectrum disorders (ASDs). Suspected autosomal recessive condition due to close familial relations Previously negative karyotyping and/or chromosomal microarray results. Test Description This panel analyzes 2429 genes that have been associated with Autism and ID and/or disorders associated with Autism and ID. Both sequencing and deletion/duplication (CNV) analysis will be performed on the coding regions of all genes included (unless otherwise marked). All analysis is performed utilizing Next Generation Sequencing (NGS) technology. CNV analysis is designed to detect the majority of deletions and duplications of three exons or greater in size. Smaller CNV events may also be detected and reported, but additional follow-up testing is recommended if a smaller CNV is suspected. All variants are classified according to ACMG guidelines. Condition Description Autism Spectrum Disorder (ASD) refers to a group of developmental disabilities that are typically associated with challenges of varying severity in the areas of social interaction, communication, and repetitive/restricted behaviors. -
Rare Copy Number Variants Are an Important Cause of Epileptic Encephalopathies
ORIGINAL ARTICLE Rare Copy Number Variants Are an Important Cause of Epileptic Encephalopathies Heather C. Mefford, MD, PhD,1 Simone C. Yendle, BSc,2 Cynthia Hsu, BS,1 Joseph Cook, MS,1 Eileen Geraghty, BA,1 Jacinta M. McMahon, BSc,2 Orvar Eeg-Olofsson, MD, PhD,3 Lynette G. Sadleir, MBChB, MD,4 Deepak Gill, MBBS, BSc,5 Bruria Ben-Zeev, MD,6,7 Tally Lerman-Sagie, MD,7,8 Mark Mackay, MBBS,9,10 Jeremy L. Freeman, MBBS,10 Eva Andermann, MD, PhD,11 James T. Pelakanos, MBBS,12 Ian Andrews, MBBS,13 Geoffrey Wallace, MBBS,14 Evan E. Eichler, PhD,15,16 Samuel F. Berkovic, MD,2 and Ingrid E. Scheffer, MBBS, PhD2,9,10,17 Objective: Rare copy number variants (CNVs)—deletions and duplications—have recently been established as important risk factors for both generalized and focal epilepsies. A systematic assessment of the role of CNVs in epileptic encephalopathies, the most devastating and often etiologically obscure group of epilepsies, has not been performed. Methods: We evaluated 315 patients with epileptic encephalopathies characterized by epilepsy and progressive cognitive impairment for rare CNVs using a high-density, exon-focused, whole-genome oligonucleotide array. Results: We found that 25 of 315 (7.9%) of our patients carried rare CNVs that may contribute to their phenotype, with at least one-half being clearly or likely pathogenic. We identified 2 patients with overlapping deletions at 7q21 and 2 patients with identical duplications of 16p11.2. In our cohort, large deletions were enriched in affected individuals compared to controls, and 4 patients harbored 2 rare CNVs. -

HIST1H2BB and MAGI2 Methylation and Somatic Mutations As Precision Medicine Biomarkers for Diagnosis and Prognosis of High-Grade Serous Ovarian Cancer Blanca L
Published OnlineFirst June 24, 2020; DOI: 10.1158/1940-6207.CAPR-19-0412 CANCER PREVENTION RESEARCH | RESEARCH ARTICLE HIST1H2BB and MAGI2 Methylation and Somatic Mutations as Precision Medicine Biomarkers for Diagnosis and Prognosis of High-grade Serous Ovarian Cancer Blanca L. Valle1, Sebastian Rodriguez-Torres2,3, Elisabetta Kuhn4,5, Teresa Díaz-Montes6, Edgardo Parrilla-Castellar7, Fahcina P. Lawson1, Oluwasina Folawiyo1, Carmen Ili-Gangas8, Priscilla Brebi-Mieville8, James R. Eshleman9, James Herman3, Ie-Ming Shih4, David Sidransky1, and Rafael Guerrero-Preston1,10,11 ABSTRACT ◥ Molecular alterations that contribute to long-term (LT) (n ¼ 35). Immunoblot and clonogenic assays after pharma- and short-term (ST) survival in ovarian high-grade serous cologic unmasking show that HIST1H2BB and MAGI2 carcinoma (HGSC) may be used as precision medicine promoter methylation downregulates mRNA expression biomarkers. DNA promoter methylation is an early event levels in ovarian cancer cells. We then used qMSP in paired in tumorigenesis, which can be detected in blood and urine, tissue, ascites, plasma/serum, vaginal swabs, and urine from making it a feasible companion biomarker to somatic muta- a third cohort of patients with HGSC cancer (n ¼ 85) to test tions for early detection and targeted treatment workflows. the clinical potential of HIST1H2BB and MAGI2 in precision We compared the methylation profile in 12 HGSC tissue medicine workflows. We also performed next-generation samples to 30 fallopian tube epithelium samples, using the exome sequencing of 50 frequently mutated in human cancer Infinium Human Methylation 450K Array. We also used genes, using the Ion AmpliSeqCancer Hotspot Panel, to 450K methylation arrays to compare methylation among show that the somatic mutation profile found in tissue and HGSCs long-term survivors (more than 5 years) and short- plasma can be quantified in paired urine samples from term survivors (less than 3 years). -

Blueprint Genetics Beyond Paediatric Epilepsy Panel – for Europe And
Beyond Paediatric Epilepsy Panel – for Europe and Middle East Test code: NE2401 Is a 416 gene panel that includes assessment of non-coding variants. In addition, it also includes the maternally inherited mitochondrial genome. The Paediatric Epilepsy? Look Beyond program offers eligible paediatric patients in European and Middle East Countries comprehensive genetic diagnostics for their epileptic disorder. The major inclusion criteria for this program are: 1. Be ≥24 and ≤48 months old 2. Unprovoked seizures started after 2 year of age 3. One of the following signs/symptoms: history language delay or regression, motor impairments or regression (ataxia, abnormal gait, etc), EEG abnormality, MRI abnormality 4. Have a copy of original medical data report from the physician or hospital assessing clinical condition of the patients 5. Patient lives in Europe or the Middle East* Additional information about the program is available at blueprintgenetics.com/beyondpaediatricepilepsy/. The Blueprint Genetics Comprehensive Epilepsy Panel is used in this program. *To see the complete list of countries included in the programme please click here. Please note when ordering there is a limitation of 5 samples per institution for the year 2020 About Beyond Paediatric Epilepsy – for Europe and Middle East Epilepsy is defined by recurrent, unprovoked seizures due to abnormal, synchronized neuronal firing in the brain. It is one of the most common neurological conditions. Approximately 20-30 % of epilepsy cases are caused by acquired conditions, but the remaining 70-80 % of cases are believed to be due to one or more genetic factors. The epilepsies can be broadly grouped into three classes: genetic generalized epilepsy (formerly idiopathic generalized epilepsy); focal epilepsy; and epileptic encephalopathy. -

MAGI2 Enhances the Sensitivity of BEL-7404 Human Hepatocellular Carcinoma Cells to Staurosporine- Induced Apoptosis by Increasing PTEN Stability
INTERNATIONAL JOURNAL OF MOLECULAR MEDICINE 32: 439-447, 2013 MAGI2 enhances the sensitivity of BEL-7404 human hepatocellular carcinoma cells to staurosporine- induced apoptosis by increasing PTEN stability XIN LI1,4, ZENGXIA LI1-3, NA LI1, JINGJING QI1, KUN FAN1, PENG YIN1, CHAO ZHAO1, YONGLEI LIU1, WANTONG YAO1, XIUMEI CAI1-3, LIYING WANG1-3 and XILIANG ZHA1-3 1Department of Biochemistry and Molecular Biology, School of Basic Medical Science, Fudan University; 2Key Laboratory of Glycoconjugate Research, Ministry of Health; 3Key Laboratory of Molecular Medicine, Ministry of Education, Shanghai 200032; 4Department of Laboratory Medicine, Shanghai Public Health Clinical Center, Fudan University, Shanghai 201508 P.R. China Received February 24, 2013; Accepted April 29, 2013 DOI: 10.3892/ijmm.2013.1411 Abstract. Adaptor proteins are involved in the assembly of of AKT. These results suggest that MAGI2 overexpression various intracellular complexes and the regulation of cellular enhances the sensitivity of cancer cells harboring ectopic functions. Membrane-associated guanylate kinase inverted 2 PTEN to STS-induced apoptosis. (MAGI2), also known as synaptic scaffolding molecule (S-SCAM), plays a critical role in signal transduction by assem- Introduction bling and anchoring its ligands. However, the role of MAGI2 in mediating apoptosis remains largely unknown. In the present Thousands of adaptor proteins are known in metazoans which study, BEL-7404 human hepatocellular carcinoma cells were are involved in the assembly of various intracellular complexes transfected with a plasmid containing myc-MAGI2 or an and the regulation of cellular functions (1). Cytoplasmic scaffold empty plasmid and cell viability was then determined using proteins may be defined as proteins that link two or more part- the Cell Counting kit-8. -
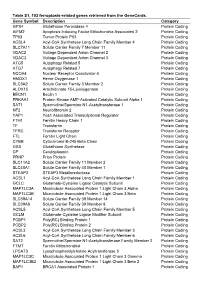
Table S1. 103 Ferroptosis-Related Genes Retrieved from the Genecards
Table S1. 103 ferroptosis-related genes retrieved from the GeneCards. Gene Symbol Description Category GPX4 Glutathione Peroxidase 4 Protein Coding AIFM2 Apoptosis Inducing Factor Mitochondria Associated 2 Protein Coding TP53 Tumor Protein P53 Protein Coding ACSL4 Acyl-CoA Synthetase Long Chain Family Member 4 Protein Coding SLC7A11 Solute Carrier Family 7 Member 11 Protein Coding VDAC2 Voltage Dependent Anion Channel 2 Protein Coding VDAC3 Voltage Dependent Anion Channel 3 Protein Coding ATG5 Autophagy Related 5 Protein Coding ATG7 Autophagy Related 7 Protein Coding NCOA4 Nuclear Receptor Coactivator 4 Protein Coding HMOX1 Heme Oxygenase 1 Protein Coding SLC3A2 Solute Carrier Family 3 Member 2 Protein Coding ALOX15 Arachidonate 15-Lipoxygenase Protein Coding BECN1 Beclin 1 Protein Coding PRKAA1 Protein Kinase AMP-Activated Catalytic Subunit Alpha 1 Protein Coding SAT1 Spermidine/Spermine N1-Acetyltransferase 1 Protein Coding NF2 Neurofibromin 2 Protein Coding YAP1 Yes1 Associated Transcriptional Regulator Protein Coding FTH1 Ferritin Heavy Chain 1 Protein Coding TF Transferrin Protein Coding TFRC Transferrin Receptor Protein Coding FTL Ferritin Light Chain Protein Coding CYBB Cytochrome B-245 Beta Chain Protein Coding GSS Glutathione Synthetase Protein Coding CP Ceruloplasmin Protein Coding PRNP Prion Protein Protein Coding SLC11A2 Solute Carrier Family 11 Member 2 Protein Coding SLC40A1 Solute Carrier Family 40 Member 1 Protein Coding STEAP3 STEAP3 Metalloreductase Protein Coding ACSL1 Acyl-CoA Synthetase Long Chain Family Member 1 Protein