In the Name of God, the Beneficent, the Merciful
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Comparison of Etoricoxib and Indomethacin for the Treatment of Experimental Periodontitis in Rats
Brazilian Journal of Medical and Biological Research (2007) 40: 117-125 Etoricoxib in experimental periodontitis 117 ISSN 0100-879X Comparison of etoricoxib and indomethacin for the treatment of experimental periodontitis in rats M.C.F. Azoubel1, 1Departamento de Fisiologia e Farmacologia, A.M.A. Menezes1, 2Departamento de Morfologia, Faculdade de Medicina, D. Bezerra1, R.B. Oriá2, Universidade Federal do Ceará, Fortaleza, CE, Brasil R.A. Ribeiro1 and G.A.C. Brito2 Abstract Correspondence We investigated the effect of etoricoxib, a selective cyclooxygenase- Key words G.A.C. Brito 2 inhibitor, and indomethacin, a non-selective cyclooxygenase inhib- • Alveolar bone loss Departamento de Fisiologia itor, on experimental periodontitis, and compared their gastrointesti- • Inflammation e Farmacologia nal side effects. A ligature was placed around the second upper left • Periodontitis Faculdade de Medicina, UFC molars of female Wistar rats (160 to 200 g). Animals (6 per group) • Cyclooxygenase inhibitors Rua Coronel Nunes de Melo, 1127 • were treated daily with oral doses of 3 or 9 mg/kg etoricoxib, 5 mg/kg Etoricoxib 60430-270 Fortaleza, CE • Indomethacin Brasil indomethacin, or 0.2 mL saline, starting 5 days after the induction of Fax: +55-85-3366-8333 periodontitis, when bone resorption was detected, until the sacrifice E-mail: [email protected] on the 11th day. The weight and survival rate were monitored. Alveolar bone loss (ABL) was measured as the sum of distances Research supported by CNPq and between the cusp tips and the alveolar bone. The gastric mucosa was Fundação Cearense de Pesquisa e examined macroscopically and the periodontium and gastric and Cultura (FUNCAP). -

Lecture 2 – Bone
Oral Histology Summary Notes Enoch Ng Lecture 2 – Bone - Protection of brain, lungs, other internal organs - Structural support for heart, lungs, and marrow - Attachment sites for muscles - Mineral reservoir for calcium (99% of body’s) and phosphorous (85% of body’s) - Trap for dangerous minerals (ex:// lead) - Transduction of sound - Endocrine organ (osteocalcin regulates insulin signaling, glucose metabolism, and fat mass) Structure - Compact/Cortical o Diaphysis of long bone, “envelope” of cuboid bones (vertebrae) o 10% porosity, 70-80% calcified (4x mass of trabecular bone) o Protective, subject to bending/torsion/compressive forces o Has Haversian system structure - Trabecular/Cancellous o Metaphysis and epiphysis of long bone, cuboid bone o 3D branching lattice formed along areas of mechanical stress o 50-90% porosity, 15-25% calcified (1/4 mass of compact bone) o High surface area high cellular activity (has marrow) o Metabolic turnover 8x greater than cortical bone o Subject to compressive forces o Trabeculae lined with endosteum (contains osteoprogenitors, osteoblasts, osteoclasts) - Woven Bone o Immature/primitive, rapidly growing . Normally – embryos, newborns, fracture calluses, metaphyseal region of bone . Abnormally – tumors, osteogenesis imperfecta, Pagetic bone o Disorganized, no uniform orientation of collagen fibers, coarse fibers, cells randomly arranged, varying mineral content, isotropic mechanical behavior (behavior the same no matter direction of applied force) - Lamellar Bone o Mature bone, remodeling of woven -

The Cementum: Its Role in Periodontal Health and Disease*
THE JOURNAL OF PERIODONTOLOGY JULY, NINETEEN HUNDRED SIXTY ONE The Cementum: Its Role In Periodontal Health and Disease* by DONALD A. KERR, D.D.S., M.S.,** Ann Arbor, Michigan HE cementum is a specialized calcified tissue of mesenchymal origin which provides for the attachment of the periodontal fibers to the surface of the Troot. It consists of 45 to 50 per cent inorganic material and 50 to 55 per cent organic material with the inorganic material in a hydroxyl apatite structure. The primary cementum is formed initially by appositional growth from the dental sac and later from the periodontal membrane under the influence of cementoblasts. It is formed in laminated layers with the incorporation of Sharpey's fibers into a fibrillar matrix which undergoes calcification. Cementum deposition is a Continuous process throughout life with new cementum being deposited over the old cemental surface. Cementum is formed by the organiza• tion of collagen fibrils which are cemented together by a matrix produced by the polymerization of mucopolysaccharides. This material is designated as cementoid and becomes mature cementum upon calcification. The significance of the continuous deposition of cementum has received various interpretations. 1. Continuous deposition of cementum is necessary for the reattachment of periodontal fibers which have been destroyed or which require reorientation due to change in position of teeth. It is logical that there should be a continuous deposition of cementum because it is doubtful that the initial fibers are retained throughout the life of the tooth, and therefore new fibers must be continually formed and attached by new cementum. -

Clinical Significance of Dental Anatomy, Histology, Physiology, and Occlusion
1 Clinical Significance of Dental Anatomy, Histology, Physiology, and Occlusion LEE W. BOUSHELL, JOHN R. STURDEVANT thorough understanding of the histology, physiology, and Incisors are essential for proper esthetics of the smile, facial soft occlusal interactions of the dentition and supporting tissues tissue contours (e.g., lip support), and speech (phonetics). is essential for the restorative dentist. Knowledge of the structuresA of teeth (enamel, dentin, cementum, and pulp) and Canines their relationships to each other and to the supporting structures Canines possess the longest roots of all teeth and are located at is necessary, especially when treating dental caries. The protective the corners of the dental arches. They function in the seizing, function of the tooth form is revealed by its impact on masticatory piercing, tearing, and cutting of food. From a proximal view, the muscle activity, the supporting tissues (osseous and mucosal), and crown also has a triangular shape, with a thick incisal ridge. The the pulp. Proper tooth form contributes to healthy supporting anatomic form of the crown and the length of the root make tissues. The contour and contact relationships of teeth with adjacent canine teeth strong, stable abutments for fixed or removable and opposing teeth are major determinants of muscle function in prostheses. Canines not only serve as important guides in occlusion, mastication, esthetics, speech, and protection. The relationships because of their anchorage and position in the dental arches, but of form to function are especially noteworthy when considering also play a crucial role (along with the incisors) in the esthetics of the shape of the dental arch, proximal contacts, occlusal contacts, the smile and lip support. -

Splitting of the Alveolar Process of the Lower Jaw
SPLITTING OF THE ALVEOLAR PROCESS OF THE LOWER JAW. Peekskill, N. Y., Nov. 1, 1858. Messrs. Editors:—I send you the following communica tion, which I received from G. J. Fisher, M. D., of Sing Sing, New York, eminent as a surgeon in this part of the country, which you are at liberty to publish, if you think it of suffi cient interest to the dental profession, to be intitled to a place in your valuable journal. Respectfully, yours, E. D. Fuller, D. D. S. Sing Sing, N. Y., October 28, 1858. My Dear Friend :—I send you an account of a case which is so near the boundary line which separates dental from general surgery, that you may be interested with it, and even consider it worthy of insertion in some one of the journals devoted to your speciality. You are at liberty to use it as your own. Miss V., of Tarrytown, New York, a tall and comely lass, while engaged in juvenile sports with several children in the dining room, was tripped by her dress, causing her to fall, with great violence, striking the front teeth of the lower jaw against the margin of a mahogony table. On arising, she found the teeth driven into the mouth, and the jaw broken*. She applied to a physician, who directed her to a dentist for treatment. She came to Sing Sing the following day (Oct. 20th), and applied to Dentist Greenleaf, who, after examin ing the case, came to the conclusion that it was a little more surgical than dental, and therefore called me in to treat the injury. -

Hereditary Gingival Hyperplasia – Case Report Dziedziczny Przerost Dziąseł – Opis Przypadków
CLINICAL CASE Dent. Med. Probl. 2011, 48, 3, 443–449 © Copyright by Wroclaw Medical University ISSN 1644-387X and Polish Dental Society Karolina Thum-Tyzo¹, Beata Petkowicz², Joanna Wysokińska-Miszczuk¹ Hereditary Gingival Hyperplasia – Case Report Dziedziczny przerost dziąseł – opis przypadków ¹ Chair and Department of Periodontology of the Medical University of Lublin, Poland ² Oral Medicine Independent Unit of the Medical University of Lublin, Poland Abstract Hereditary gingival hyperplasia is a rare case in clinical practice. The study describes two cases of this pathology occurring in several members of one family. This disease is inherited in an autosomal dominant or recessive way. Patients affected by this disease require a thorough diagnosis. In addition to basic medical history and dental examination, outside and inside oral cavity, additional study may be needed. The first reported case concerns a young mother with enlargement of gum tissue, which also appeared in her children, mother and grandmother. In children, hyperplasia has caused the delay in the eruption of permanent teeth, diastema secondary, dental abnor- malities, changes in facial appearance and problems with oral hygiene. Similar changes were observed in the second case described a father and son for whom gingival hyperplasia was a serious problem, with respect to functional and aesthetic disturbances, deteriorating quality of life. The aim of this study is to present the problems associated with enlargement of the gums and the difficulty in the treatment this disease which is not always successful (Dent. Med. Probl. 2011, 48, 3, 443–449). Key words: gingival hyperplasia, inherited disease, gingivectomy. Streszczenie Dziedziczny rozrost dziąseł jest przypadkiem rzadko spotykanym w praktyce klinicznej. -
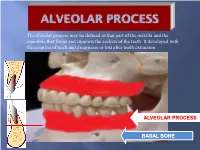
Alveolar Process May Be Defined As That Part of the Maxilla and the Mandible That Forms and Supports the Sockets of the Teeth
The alveolar process may be defined as that part of the maxilla and the mandible that forms and supports the sockets of the teeth. It developed with the eruption of teeth and disappears or lost after tooth extraction ALVEOLAR PROCESS BASAL BONE Alveolar (bone) process: is that part of the maxilla and the mandible that forms and supports the sockets of the teeth. Basal Bone. it is the bone of the facial skeleton which support the alveolar bone. There is no anatomical boundary between basal bones and alveolar bone. Both alveolar process and basal bone are covered by the same periosteum. In some areas alveolar processes may fuse or masked with jaw bones as in (1) Anterior part of maxilla (palatal). (2) Oblique line of the mandible. * Alveolar process is resorbed after extraction of teeth. Functions of alveolar bone – Houses and protects developing permanent teeth, while supporting primary teeth. – Organizes eruption of primary and permanent teeth. – Anchors the roots of teeth to the alveoli, which is achieved by the insertion of Sharpey’s fibers into the alveolar bone proper (attachment). – Helps to move the teeth for better occlusion (support). – Helps to absorb and distribute occlusal forces generated during tooth contact (shock absorber). – Supplies vessels to periodontal ligament. •DEVELOPMENT OF ALVEOLAR BONE •Near the end of the second month of fetal life, the maxilla as well as the mandible form a groove that is open towards the surface of the oral cavity. •Tooth germs develop within the bony structures at late bell stage. •Bony septa and bony bridge begin to form and separatethe individual tooth germs from one another, keeping individual tooth germs in clearly outlined bony compartments. -

Alveolar Bone in Health
Review Article DOI: 10.18231/2457-0087.2017.0002 Alveolar bone in health Suchetha A.1, Esha Tanwar2,*, Sapna N3, Divya Bhat4, Spandana A5 1Professor & Head, 2,5PG Student, 3Reader, 4Senior Lecturer, Dept. of Periodontology, DAPMRV Dental College, Bangalore, Karnataka *Corresponding Author: Email: [email protected] Abstract Alveolar bone is the component of the maxilla and the mandible that accommodates and supports the alveoli of the teeth. The alveolar bone comprises of two parts-alveolar bone proper which lines the socket of the tooth along with root, cementum and the periodontal ligament (periodontium) constitutes the Attachment apparatus; and the supporting alveolar bone. This attachment apparatus provides support to the tooth in the jaw as well as distributes forces generated by the teeth uniformly to the alveolar bone surrounding it. These functional changes are expressed by the process of ‘Bony remodelling’ in alveolar process. Therefore, this review provides an understanding of the anatomical aspect of alveolar bone and the molecular events that balance the formation and remodelling of alveolar bone. Keywords: Alveolar Bone, Attachment Apparatus, Bony Remodelling. Introduction analysis of its role in periodontal diseases and systemic Bone is a remarkably dynamic as well as an active diseases. tissue, which constantly undergoes renewal in response to physiologic and pathologic stimulations.(1) Composition of Alveolar Bone The alveolar bone is the component of the maxilla Alveolar bone is a mineralized connective tissue. and the -

Scholars Journal of Medical Case Reports
DOI: 10.21276/sjmcr.2016.4.6.16 Scholars Journal of Medical Case Reports ISSN 2347-6559 (Online) Sch J Med Case Rep 2016; 4(6):416-419 ISSN 2347-9507 (Print) ©Scholars Academic and Scientific Publishers (SAS Publishers) (An International Publisher for Academic and Scientific Resources) Hereditary Gingival Fibromatosis: A Case Report with Review of Literature Jesudass Govada1, Sridhar Reddy Erugula2, Narendra Kumar Narahari3, Vijay Kumar R4,Rajajee KTSS5, Sudhir Kumar Vujhini6 1Associate Professor, Department of Pedodontics and Preventive Dentistry, Government Dental College and Hospital, RIMS, Kadapa, Andhra Pradesh, India 2Senior lecturer, Department of Oral Pathology, MNR Dental College and Hospital, Sangareddy, Telangana, India 3Assistant Professor, Department of Respiratory Medicine, Nizam’s Institute of Medical Sciences, Hyderabad, India. 4Assistant Professor, Dept. of Dentistry, Govt. Dental College, Ananthapur,, Andhra Pradesh, India 5Reader, Dept of Pedodontics, Anil Neerukonda Institute of Dental Sciences, Visakhapatnam, Andhra Pradesh, India. 6Assistant Professor, Transfusion Medicine, Nizam’s Institute of Medical Sciences, Hyderabad, India *Corresponding author Sudhir Kumar Vujhini Email: [email protected] Abstract: Gingival fibromatosis is characterized by localized or generalized fibrous enlargement of the gingivae, mainly around permanent teeth. Gingival fibromatosis affects only the masticatory mucosa and does not extend beyond the muco-gingival junction. This article describes an unusual case of hereditary gingival fibromatosis with delayed eruption of permanent teeth in an 11 year-old girl and her younger sibling. The patient presented with severely enlarged gingival tissues affecting both arches and multiple retained deciduous. Most of the permanent teeth were not erupted. She had no associated symptoms to suggest any syndrome but there was family history of similar disorder with father and paternal aunt. -

Healing After Partial Denudation of the Alveolar Process<Link Href="#Fn 1"/>
Healing after Partial Denudation adjacent areas. The gingivectomy was done with a bev• eled incision which extended to the alveolar crest. Then of the Alveolar Process* the labial soft tissues, including the periosteum were removed over the experimental tooth leaving a strip of exposed bone 3 to 4 mm apically from the alveolar crest by (Fig. 1), and approximately 6 mm wide mesiodistally. EMMETT R. COSTICH,** D.D.S., PH.D. Measurements from the reference notch to the re• SIGURD P. RAMFJORD,*** L.D.S., PH.D. maining soft tissue attachment, to the alveolar crest and to the apical border of the bone exposure were recorded ALTHOUGH extensive buccal and lingual denudation of at the completion of the experimental surgery. the alveolar process has been abandoned, bone is often exposed at the alveolar crest and in interproximal areas A surgical dressing (Wondr-Pak) was placed over the during periodontal surgery. The purpose of the present blood covered bone and soft tissue wound. The dressing investigation was to study the healing after surgical de• was changed at weekly intervals until the wound healed. nudation of small areas of the alveolar process in Some specimens were obtained before the healing was humans. complete and in these cases the dressing was retained until the removal of the experimental block section. MATERIAL Clinical pictures and measurements from the refer• Ten immediate denture patients at The University of ence notch to the free gingival margin, and to the attach• Michigan, School of Dentistry, participated in the study. ment level on the root surface were obtained just before The patients were in good health and varied from 26 to removal of the specimens. -

Periodontal Osseous Defects: a Review 1Bharath Chandra GNR, 2KL Vandana
CODSJOD Bharath Chandra GNR, KL Vandana 10.5005/jp-journals-10063-0028 REVIEW ARTICLE Periodontal Osseous Defects: A Review 1Bharath Chandra GNR, 2KL Vandana ABSTRACT The bone loss in periodontal disease occurs at local Periodontitis is an inflammatory process affecting the perio- sites, but it is regulated by both systemic and local factors. dontal tissues caused by multi-factorial origin. Among all the Bone resorption is probably the most critical factor in peri- characteristic signs of periodontal disease, loss of support from odontal attachment loss leading to eventual tooth loss.2 alveolar boneis the one which usually represents theanatomical Radiographically it is diagnosed by evidence of "bone sequela to the progression of periodontitis apically.The bone loss which is induced by periodontitis occur either single or in loss" around the tooth. Normally the crest of alveolar different combination forms. The identification of these osseous bone is situated between 0.4 to 1.97 mm approximately defects on surgical exposure of bone is clinically challenging apically to the cemento-enamel junction (CEJ) of thatpar- as the osseous and it becomes imperative for a clinician to ticular tooth.3 understand these defects and categorize them well to have The bone loss which is induced by periodontitis i.e better therapeutic approaches. Intimate knowledge of all these periodontal osseous defects associated with periodontal osseous defects occur either single or in different combi- disease is essential. So this review is aimed at classification nation forms. The identification of these osseous defects and deep insight which will be helpful for proper diagnosis and on surgical bone exposure is clinically challenging as the treatment of periodontal osseous defects. -

Anatomy of the Periodontium: a Biological Basis for Radiographic Evaluation of Periradicular Pathology
Vol. 6(7), pp. 70-76, November 2014 DOI: 10.5897/JDOH2014.0119 Article Number: A8D0AD648346 Journal of Dentistry and ISSN 2006-9871 Copyright © 2014 Oral Hygiene Author(s) retain the copyright of this article http://www.academicjournals.org/JDOH Case Report Anatomy of the periodontium: A biological basis for radiographic evaluation of periradicular pathology I. U. Madukwe Department of Oral Surgery and Pathology, Faculty of Dentistry, College of Medical Sciences, University of Benin, Edo State, Nigeria. Received 2 June, 2014; Accepted 8 October, 2014 The periodontium surrounds and supports the teeth and consists of four major components; gingiva, periodontal ligaments, cementum/dentin, and alveolar bone/lamina dura, with collective function of keeping the tooth in position despite varying changes and responses during mastication. A near-normal radiograph of periradicular tissues was used as the basis for evaluation of some common periradicular radiographic pathologies. Apical periodontitis was 70 (58.33%), alveolar abscess 32 (26.66%), and apical granulomas 15 (12.50%). A background anatomy of the periodontium is advocated as a precondition for accurate evaluation of periradicular pathologies. Key words: Periodontium, periradicular, pathology. INTRODUCTION The periodontium surrounds and supports the teeth. It the form of teeth, events that occur during tooth eruption, consists dominantly of four major components; gingiva, the eventual inclination and position of the fully erupted periodontal ligaments, cementum and the alveolar bone. teeth (Skoog et al., 2007; Seba et al., 2014). Gingiva and They collectively function as a unit to keep the tooth in the periodontal ligaments though not appearing radio- position, despite varying responses during mastication.