Care for the Caregiver Domain Process
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-
Community Benefit Report for Fiscal Year 2015 and 2016 Implementation Strategy
Community Benefit Report for Fiscal Year 2015 and 2016 Implementation Strategy 2 stanfordchildrens.org Contents Welcome: a Letter from Community Health Initiative: 3 our President and CEO � � � � � � � � � � � � � � � � � � � � � � � � 3 Improve the Social, Emotional and Mental Health of Children and Youth � � � � � � � � 18 Programs 19 In Depth: Reach & Rise 20 About Us � � � � � � � � � � � � � � � � � � � � � � � � � � � � � � � � � � � � � � � 6 Other FY2015 Community Patient Care Highlights 2015 � � � � � � � � � � � � � � � � � � 7 Benefit Activities � � � � � � � � � � � � � � � � � � � � � � � � � � � � � 21 In the Community: Programs that benefit the broader community 21 Community Benefit Report Overview � � � � � � � � � 8 Keeping Kids Safe: Programs that build safe communities 21 Community Benefit Defined 8 Advocacy and Outreach: A voice for children and families 22 Community Benefit Implementation Strategy 8 Workforce Development: Programs that train the next Community Health Needs Assessment 8 generation of health professionals 24 Community Benefit Oversight 8 Stanford Children’s Health Network Community Investment � � � � � � � � � � � � � � � � � � � � � � � 9 Overview � � � � � � � � � � � � � � � � � � � � � � � � � � � � � � � � � � � � � �26 Our Community 9 Joint Ventures 27 Our Investments 9 California Pacific Medical Center 27 John Muir Health 27 Community Health Initiatives � � � � � � � � � � � � � � � � 10 Our Bay Area Network � � � � � � � � � � � � � � � � � � � � � � �28 Our network locations by primary and secondary -
John Muir and UCSF Expand Network to Form Canopy Health
August 8, 2016 | VOLUME 23 | NUMBER 31 TOP STORIES John Muir and UCSF Expand Published Monday, California Healthfax is Network to Form Canopy Health copyrighted by HealthLeaders Media, a division of BLR, 35 Village Road, Suite 200, Middleton, Health plan to launch this fall with Health Net MA 01949 and is transmitted solely to the sub- scriber. Any unauthorized copying, duplication or The Bay Area Accountable Care Network established by John Muir Health transmission is strictly prohibited. Subscriptions and UCSF Health has added seven new hospitals to its network and changed its are $179 for 48 issues. For group and bulk sub- name to Canopy Health as it prepares to launch this fall. scriptions, call 800-650-6787. Canopy Health also added three new medical groups to its network to bolster a provider base that now includes more than 4,000 physicians. “We’ve CUSTOMER SERVICE CENTER made significant strides in a short amount of time as we work to provide Bay Email Subscribers: If you do not receive your copy of HealthFax, Area residents with an option to choose Canopy Health during open enrollment in send a request to: [email protected]. the fall of 2016,” said Canopy Health CEO Joel Criste. For renewals or other subscription questions, As part of its expansion, Canopy Health added Marin General Hospital, please call: 800-650-6787. By fax: 866-592-7573. Sonoma Valley Hospital, San Ramon Regional Medical Center, Washington By email: [email protected] Hospital Healthcare System, Alameda Hospital, Highland Hospital, and San Leandro Hospital. Medical groups joining the network are Hill Physicians EDITORIAL SUBMISSIONS Medical Group, which has more than 2,250 physicians in the Bay Area, the John To submit an item for consideration, con- Muir Physician Network, and Meritage Medical Network. -
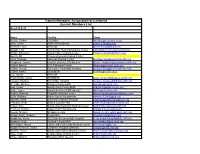
Trauma Managers Association of California Current Members List As of 10-8-15
Trauma Managers Association of California Current Members List As of 10-8-15 Name Facility Email Becker, Debra CCEMSA [email protected] Behr, Lynne Kaiser Permanente [email protected] Bennink, Lynn (Retired) [email protected] Blough, Lois Community Regional Medical Center [email protected] Bowlin, Maureen Inland Valley Medical Center [email protected] Bunch, Bill Colusa Regional Medical Center Case, Melinda Palomar Medical Center [email protected] Chapman, Joanne Coastal Valleys EMS Agency [email protected] Cohen, Marilyn UCLA Medical Center [email protected] Collins, Georgi Riverside Community Hospital [email protected] Collins, Kathy SSVEMSA [email protected] Cox, Susan (Retired) Crain-Riddle, Karen SSVEMSA [email protected] Crowley, Melanie Northridge Hospital [email protected] De Laby, Michael Orange County EMS [email protected] Diaz, Linda Santa Clara County EMS [email protected] Doyle, Lance Mountain-Valley EMS Agency [email protected] Dudley, Pamela Regional Medical Center [email protected] Duffy, Barbara Kaiser South Sacramento [email protected] Earnest, Karla Stanford Childrens Hospital [email protected] Erickson, Keith Solano County EMS [email protected] Fortier, Sue Sierra Vista Regional Medical Center [email protected] Frecceri, Christy Kaiser South Sacramento [email protected] Gawlik, Melanie Scripps La Jolla [email protected] Gough-Smith, -
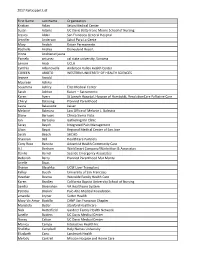
2017 Participant List First Name Last Name Organization Kristian Aclan
2017 Participant List First Name Last Name Organization Kristian Aclan Seton Medical Center Susan Adams UC Davis Betty Irene Moore School of Nursing Jessica Aldaz San Francisco General Hospital Jennifer Anderson Salud Para La Gente Mary Andich Kaiser Permanente Rochelle Andres Disneyland Resort Irinna Andrianarijaona Pamela antunez cal state university, Sonoma Lenore Arab UCLA Cynthia Arbanovella Anderson Valley Health Center COREEN ARIOTO WESTERN UNIVERSITY OF HEALTH SCIENCES Jeanne Arnold Maureen Ashiku Sosamma Ashley Elite Medical Center Sarah Ashton Kaiser -- Sacramento Karen Ayers St Joseph Hospital, Hospice of Humboldt, ResolutionCare Palliative Care Cheryl Balaoing Planned Parenthood Laura Balassone kaiser Melanie Balestra Law Office of Melanie L. Balestra Diane Barrows Clinica Sierra Vista Jan Bartuska Gathering Inn Clinic Seray Bayoh Integrated Pain Management Lilian Bayot Regional Medical Center of San Jose Sarah Beach SHCHD Shannon Bell HealthCare Partners Cony Rose Bencito Adventist Health Community Care A.J. Benham WorkSmart Company/Warbritton & Associates Danilo Bernal Seaside Emergency Associates Deborah Berry Planned Parenthood Mar Monte Arielle Bivas Sharon Blaschka UCSF Liver Transplant Kelley Booth University of San Francisco Heather Bosma Westside Family Health Care Karen Bradley California Baptist University School of Nursing Sandra Bresnahan VA Healthcare System Patricia Briskin` Palo Alto Medical Foundation amanda bryner Sutter Health Mary Vic Amor Bustillo CANP San Francisco Chapter Maristela Butler Stanford Healthcare -
NICU Data Updates
CPQCC 2016 Data Finalization Summary and Updates Santa Clara Valley Medical Center , San Jose October 3, 2017 – Janella Parucha CPQCC Member- ship CPQCC Quarterly Data Close-Out Help Desk Finalization Initiatives Summary CPQCC Website Data Center Overview Topics ì Membership ì Data Finalization Summary ì Close-Out Checklist updates ì Data Management Award comparisons by year and award type ì Quarterly Close-Out initiatives ì CPQCC Help Desk – new look ì CPQCC Updating Directories ì CPQCC Website Highlights – Where would I find? ì Downloads ì Data Trainings ì Data Finalization etc. CPQCC Participants Membership ì 2017: 138 active members ì 2016: 137 members participating in data finalization DF Resources: Close-Out Check List The Close-out Check List re-cap ì The CPQCC database automatically checks each deliverable as they are completed. ì Items 3-6 ì Items 9-14 ì The following items MUST be manually checked: ì Item 1 – Membership Dues (completed by Data Center) ì Item 2 – Confirmation of DF Guidelines ì Item 7 – Contact Report ì Item 8 – VON Membership Survey ì Once any of these items are checked, you must click the Set Confirmation status button below to complete. Close-Out Check List Manually check off 3% April 1st Deliverables Manually check off April 1st Deliverables June 1st Deliverables New HRIF eligibility criteria will be added to Item 13 for infants who: • received a diagnosis of moderate or severe HIE • surgery for Congenital Heart Disease • received Inhaled Nitric Oxide >4 hours • experience seizures June 1ST Deliverable Item #11 Confirmed Unknown Report The Close-Out Check List UPDATE ì Item# 10 included both the Error & Warning Reports and the Confirmed Unknown Report. -

Benefiting from Charity Care: California Not-For-Profit Hospitals
Benefiting from Charity Care: California Not-for-Profit Hospitals Ver. 1.1 August 15, 2012 Prepared by the Institute for Health and Socio-Economic Policy The Institute for Health & Socio-Economic Policy (IHSP) is a non-profit policy and research group and is the exclusive research arm of the California Nurses Association/National Nurses United. The IHSP focus is current political/economic policy analysis in health care and other Industries and the constructive engagement of alternative policies with international, national, state and local bodies to enhance promote and defend the quality of life for all. The Health Care Advisory Board is comprised of scholars and policy activists from the Albert Einstein College of Medicine, Boston University, Harvard University, the Canadian National Federation of Nurses’ Unions, the New School New York and the University of California. Media Inquires should be directed to: Chuck Idelson, CNA/NNU 510-2732246 Benefiting from Charity Care: California Not-for-Profit Hospitals Table of Contents. Table of Contents……………………………………………………………………………………………………………………….Page 2 Introduction…………………………………………………………………………….…………………………………………………Page 4 Summary of Findings………………………………………………………………………………………………………………….Page 5 Serving a Community Need……………………………………………………………………………………..…………………Page 9 Federal Regulation……………………………………………………………………………………………………….……………Page 9 California Regulation…………………………………………………………………………………………………………………Page 10 County and City…………………………………………………………………………………………………………………………Page 12 Net Income…………………………………………………………………………………………………….…………………………Page -

Ancillary-Roster.Pdf
John Muir Health Physician Network Ancillary Roster Vendor Address City Zip Phone ACUTE INPATIENT HOSPITALS John Muir Medical Center_Walnut Creek 1610 Ygnacio Valley Road Walnut Creek 94598 (925) 947-5252 John Muir Medical Center_Concord 2540 East Street Concord 94520 (925) 682-8200 San Ramon Regional Medical Center 6001 Norris Canyon Road San Ramon 94583 (925) 275-9200 AMBULANCE (for Humana and United HealthCare MA Secure Horizons Focus plan) Bay Medic Ambulance Service 1485 Coventry Road Concord 94518 (925) 691-8000 Pro Transport 2450 Estand Way Pleasant Hill 94523 Royal Ambulance, Inc. 14472 Wicks Blvd. San Leandro 94577 (877) 995-6161 AUDIOLOGY (for Humana and United HealthCare MA Secure Horizons Focus plan) Connect Hearing 1485 Civic Court Ste. 1330 Concord 94520 (925) 674-3607 Hearing Services of Antioch 4045 Lone Tree Way, No. D Antioch 94531 (925) 778-3298 CARDIAC CATHERIZATION SERVICES East County Cardiology 3200 Lone Tree Way, #101 Antioch 94509 (925) 777-3360 John Muir Health Outpatient Center 1450 Treat Blvd #220B Walnut Creek 94597 (925) 937-1770 John Muir Health Outpatient Center 2700 Grant St #106 Concord 94520 (925) 685-7598 John Muir Health Outpatient Center 2485 High School Avenue, #100 Concord 94520 (925) 671-0610 John Muir Health Outpatient Center 5860 Owens Drive, Suite 220 Pleasanton 94588 (925) 734-0336 John Muir Health Outpatient Center 100 Hospital Dr. #304 Vallejo 94589 (707) 557-6002 John Muir Health Outpatient Center 2101 Vale Rd #201 San Pablo 94806 (510) 233-9300 John Muir Health Outpatient Center 2400 Balfour Rd. #201 Brentwood 94513 (925) 308-8120 John Muir Medical Center_ Concord 2540 East Street Concord 94520 (925) 682-8200 Rohra Cardiovascular Inc. -
Trauma Managers Association of California Current Members List As of 4/30/17
Trauma Managers Association of California Current Members List As of 4/30/17 Trauma Center Name Facility Level Job Title Bateman, Bridgette Sierra Vista Regional Medical Center III Trauma Program Manager Behr, Lynne Kaiser San Rafael EDAT Trauma Program Director Bennink, Lynn (Retired) Blough, Lois Community Regional Medical Center I Trauma Program Director Brown, Sharon Arrowhead Regional Medical Center II Trauma Program Manager Carroll (White), Meaghan Marin General Hospital III Trauma Program Manager Case, Melinda Palomar Medical Center II Trauma Program Manager Castillejo, Aimee Pomona Valley Hospital Medical Center II Trauma Clinical Manager Chapman, Joanne Coastal Valleys EMS Agency Trauma Coordinator Chiatello, Anthony Scripps Mercy Hospital I Trauma Program Manager Cohen, Marilyn UCLA Medical Center I Trauma Program Manager Collins, Georgi Riverside Community Hospital II Trauma Program Director Crain-Riddle, Karen (Retired) / Consulting Crowley, Melanie Providence Holy Cross Medical Center II Trauma Program Manager Cruz-Manglapus, Gilda Henry Mayo Newhall Hospital II Trauma Program Manager Doyle, Lance Mountain-Valley EMS Agency Trauma Coordinator Fortier, Sue Santa Barbara Cottage Hospital II Trauma Program Manager Gough-Smith, Robynn Surgical Affiliates Management Group, Inc. Chief Administrative Officer Green, Paula Kaiser Vacaville Medical Center II Trauma Educator, Injury Prevention and Outreach Coordinator Haddleton, Kevin St.Elizabeth Community Hospital III RN Hadduck, Katy Ventura County EMS Trauma System Manager Henderson, -

2016 Community Health Needs Assessment Acknowledgments
2016 Community Health Needs Assessment Acknowledgments This report was prepared by Applied Survey Research (ASR) on behalf of the hospitals listed in this report. ASR gratefully acknowledges the contributions of the following individuals: Diana Camacho, John Muir Health Molly Bergstrom, Kaiser Permanente – Diablo Area Jean Nudelman, Kaiser Permanente – East Bay Area Debra Lambert, Kaiser Permanente – Greater Southern Alameda Area Michael Cobb, St. Rose Hospital Sue Fairbanks, San Ramon Regional Medical Center, LLC Karen Reid, San Ramon Regional Medical Center, LLC Tim Traver, San Ramon Regional Medical Center, LLC Denise Bouillerce, Stanford Health Care – ValleyCare Shelby Salonga, Stanford Health Care – ValleyCare Adam Davis, UCSF Benioff Children’s Hospital Oakland Lucy Hernandez, Washington Hospital Healthcare System Ruth Traylor, Washington Hospital Healthcare System ASR is also pleased to acknowledge the contributions of the following individuals: Dale Ainsworth, California State University, Sacramento Marianne Balin, Kaiser Permanente – Diablo Area Debi Ford, San Ramon Regional Medical Center, LLC Susan Miranda, Kaiser Permanente – Greater Southern Alameda Area Dana Williamson, Kaiser Permanente – Northern California Region Applied Survey Research is a social research firm dedicated to helping people build better communities. Bay Area Office 1871 The Alameda, Suite 180 San Jose, CA 95126 Phone: (408) 247-8319 | Fax: (408) 260-7749 1 Table of Contents ACKNOWLEDGMENTS ....................................................................................................................................... -

John Muir Physician Network Provider Directory by Specialty May, 2011
John Muir Physician Network Provider Directory by Specialty May, 2011 Allergy and Immunology David A. Cook, MD Board Certification(s): Expiration: American Board of Allergy and Immunology Lifetime Allergy & Asthma Medical Group American Board of Pediatrics Lifetime Address: Phone: Fax: 130 La Casa Via#2-209 Walnut Creek CA 94598 (925) 935-6252 (925) 935-7611 2305 Camino Ramon #225 San Ramon CA 94583 (925) 327-1450 (925) 327-1454 Anthony N. DeMeo, MD Board Certification(s): Expiration: American Board of Allergy and Immunology Lifetime Anthony DeMeo, M.D. American Board of Internal Medicine Lifetime Address: Phone: Fax: 1844 San Miguel Drive #305 Walnut Creek CA 94596 (925) 939-3437 (925) 939-7814 Joshua S. Jacobs, MD Board Certification(s): Expiration: American Board of Allergy and Immunology 12/31/2017 Allergy & Asthma Medical Group Address: Phone: Fax: 130 La Casa Via #2-209 Walnut Creek CA 94598 (925) 935-6252 (925) 935-7611 350 John Muir Parkway #180 Brentwood CA 94513 (925) 513-3140 (925) 513-2830 5575 W. Las Positas Blvd. #230 Pleasanton CA 94588 (925) 463-9400 (925) 463-8554 Barbara I. Karpel, MD Board Certification(s): Expiration: American Board of Pediatrics Lifetime Allergy & Asthma Medical Group American Board of Allergy and Immunology Lifetime Address: Phone: Fax: 2305 Camino Ramon #225 San Ramon CA 94583 (925) 327-1450 (925) 327-1454 5575 W. Las Positas, #230 Pleasanton CA 94588 (925) 463-9400 (925) 463-8554 Matthew J. Lodewick, MD Board Certification(s): Expiration: American Board of Pediatrics 12/31/2015 Allergy & Asthma Medical Group American Board of Allergy and Immunology 12/31/2013 Address: Phone: Fax: 2305 Camino Ramon #225 San Ramon CA 94583 (925) 327-1450 (925) 327-1454 130 La Casa Via #2-209 Walnut Creek CA 94598 (925) 935-6252 (925) 935-7611 Nancy B. -

Cha Human Resources Committee Conference Call
CHA HUMAN RESOURCES COMMITTEE CONFERENCE CALL February 27, 2019 1:00 - 2:00 p.m. Dial-in: 1-800-882-3610 Passcode: 7940090# AGENDA ITEM TIME SUBJECT I. 1:00 - 1:05 p.m. WELCOME, INTRODUCTIONS A. HR Committee Roster: changes to Michele Coughlin II. 1:05 - 1:10 p.m. CALIFORNIA HOSPITAL POLITICAL ACTION COMMITTEE (CHPAC) III. 1:10 - 1:45 p.m. LEGISLATIVE/REGULATORY UPDATE A. General update and expected needs B. Dynamex C. Cal/OSHA Regulations IV. 1:45 - 2:00 p.m. EDUCATION A. CHA Employee Safety and Workers Compensation Seminar 1. Program information: Available online here March 14: Costa Mesa Register online here March 20: Sacramento Register online here B. Joint HR and Workforce Summit: September 12, 2019 C. CHA Labor & Employment Law Seminar Planning V. 2:00 p.m. ADJOURN ANTITRUST POLICY STATEMENT This meeting will bring together representatives of organizations that are competitors to explore issues that might provide general benefit to the industry. Although the subject matter of these discussions is not intended to restrain competition in any manner, it is important for everyone to recognize that this meeting conceivably could be characterized as an opportunity for inappropriate information exchanges or agreements that result in anticompetitive or otherwise unlawful conduct in violation of the antitrust laws. It is the intent of all participants that this meeting and their participation in it will comply fully with all legal obligations. In particular, any discussions or agreements that could raise antitrust concerns are entirely beyond the bounds of this meeting and the advice of legal counsel will be sought if there is any question in this regard. -

East Bay Hospitals Planning $4 Billion in Construction - San Francisco Business Times: Page 1 of 5
East Bay hospitals planning $4 billion in construction - San Francisco Business Times: Page 1 of 5 Members: S Choose Another City: San Francisco K HOME NEWS SMALL BUSINESS SALES & MKTG REAL ESTATE EVENTS COMMUNITY CAREERS CITY GUIDE MORE TOPICS Green awards nominations Email Alerts EXCLUSIVE REPORTS San Francisco > Print Edition > Industries > Health Care Friday, April 25, 2008 East Bay hospitals planning $4 billion in construction San Francisco Business Times - by Chris Rauber Print Email Reprints RSS Feeds Add to Del.icio.us Digg This Comments (1) Related News More than $4 billion in hospital rebuild projects are on the books in the East Bay, including huge projects at Kaiser Permanente and Richmond City Hall sees $100M rehab John Muir Health, and nearly $2 billion in proposed work at Clark to build $80M Highland Hospital, Children's Hospital Oakland and Alta Bates University of Maryland Summit. residence hall Stanford sues And that doesn't include Doctors Medical Center in San Pablo, Se builder over humid which is scrambling to escape bankruptcy protection, and has little genomics lab, ruined chance of making rapid progress on a state-mandated seismic DNA Vie rebuild in the immediate future. Sutter Health to postpone hospitals With construction costs hovering around $2.5 million per bed and S Stanford hospitals tap architects for $2 state seismic safety deadlines looming in January 2013, the B billion project consequences of making the wrong decision are huge, which explains C why some hospital executives are taking their time before making a Su final decision. Cost inflation has eased in recent months, said health-care principal Gary fun Burk of Ratcliff Architects in Emeryville, but still remains high, despite slowdowns rela elsewhere in the economy.