Epikeratophakia for Keratoconus
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-
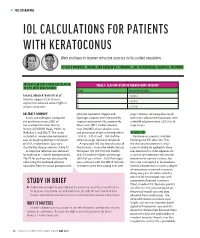
Iol Calculations for Patients with Keratoconus
s THE LITERATURE IOL CALCULATIONS FOR PATIENTS WITH KERATOCONUS Work continues to improve refractive accuracy in this patient population. BY ALICE ROTHWELL, MBCHB, AND ANDREW M.J. TURNBULL, BM, PGCERTMEDED, PGDIPCRS, FRCOPHTH INTRAOCULAR LENS POWER CALCULATION TABLE 1. CLASSIFICATION OF KERATOCONUS SEVERITY IN EYES WITH KERATOCONUS Stage Keratometry Reading Savini G, Abbate R, Hoffer KJ, et al1 1 ≤ 48.00 D Industry support: K.J.H. licenses 2 > 48.00 D registered trademark name Hoffer to various companies 3 > 53.00 D ABSTRACT SUMMARY spherical equivalent. Myopic and stage 1 disease. Accuracy decreased Savini and colleagues compared hyperopic surprises were indicated by with more advanced keratoconus, with the prediction errors (PEs) of negative and positive PEs, respectively. a MedAE of greater than 2.50 D in all five standard formulas: Barrett Mean error (ME), median absolute stage 3 eyes. Universal II (BUII), Haigis, Hoffer Q, error (MedAE), mean absolute error, Holladay 1, and SRK/T. The study and percentage of eyes achieving within DISCUSSION included 41 consecutive keratoconic ±0.50 D, ±0.75 D, and ±1.00 D of the Keratoconus presents multiple eyes undergoing phacoemulsification refractive target were also calculated. challenges to IOL selection. First, and IOL implantation. Eyes were A hyperopic ME was found across all the standard keratometric index classified by disease severity (Table 1). five formulas. Across the whole dataset, cannot reliably be applied to these A subjective refraction was obtained the lowest ME (0.91 D) and MedAE eyes because this index depends on for each eye at 1 month postoperatively. (0.62 D) and the highest percentage a normal ratio between the anterior The PE for each eye was calculated by (36%) of eyes within ±0.50 D of target and posterior corneal surfaces, but subtracting the predicted spherical were achieved with the SRK/T formula. -

Improved Preservation of Human Corneal Basement Membrane
BritishJournal ofOphthalmology 1994; 78: 863-870 863 Improved preservation ofhuman corneal basement membrane following freezing of donor tissue for Br J Ophthalmol: first published as 10.1136/bjo.78.11.863 on 1 November 1994. Downloaded from epikeratophakia Robert D Young, W John Armitage, Paul Bowerman, Stuart D Cook, David L Easty Abstract States, good results continue to be achieved by Current methods for the production of the small number ofBritish surgeons performing lenticules for epikeratophakia involve rapid the technique.4 However, no comprehensive freezing, cryolathing, and slow warming of the account of its long term outcome has yet been donor cornea. We have found that this pro- published. cedure causes structural damage to the Several complications resulting in the failure epithelial basement membrane in the donor of epikeratophakia have been reported, includ- cornea which may subsequently contribute to ing infection, graft dehiscence, persistent inter- poor postoperative re-epithelialisation of the face haze or opacity, ulceration, and imperfect implant, leading to graft failure. Endeavouring re-epithelialisation. Among these, the failure of to overcome these problems, the effects of host epithelial cells to migrate over and re- cryoprotection of donor cornea were investi- surface the anterior face of the grafted tissue gated, using dimethyl sulphoxide, in conjunc- continues to be the major reason for the removal tion with different cooling and warming rates ofepikeratophakia lenticules.'-'0 as part of the protocol for cryolathing. The Epithelial healing is itselfa complex phenome- structural integrity of the epithelial basement non involving mitosis of host cells at the graft membrane zone (BMZ) was then assessed by periphery, centripetal migration, and attach- electron microscopy and by immunofluores- ment. -

Photorefractive Keratectomy for Correction of Epikeratophakia
CASE REPORTS AND SMALL CASE SERIES high myopia resulting from poste- results might be related to the pre- Photorefractive Keratectomy rior lenticonus. Postsurgical refrac- existing corneal stromal abnormali- for Correction of tion was stable for 8 years, then a ties in their patients, which were not Epikeratophakia Regression rapid myopic regression of the epi- observed in our group. Thus, PRK keratophakic lenses was observed can effectively be used to treat epi- Excimer laser photorefractive kera- the following year (Table). In- keratophakic regressed lenses in a se- tectomy (PRK) is widely used for the stead of removing the failed epikera- lected group of patients in whom correction of myopia, astigmatism, tophakic lenses, we performed PRK both the epikeratograft and the sur- and hyperopia.1,2 It has also been on the eyes. rounding cornea are clear. This used for correction of astigmatism method eliminates the need for re- after penetrating keratoplasty.3 Results. Two and a half years after moval of the epikeratograft and ex- Epikeratophakia has been used PRK, the refraction in all 4 eyes is posing the patient to the risks of suc- in the treatment of nontolerant con- stable and the epigrafts are clear. The cessive penetrating keratoplasty. tact lens keratoconous patients.4,5 Table presents the refraction and vi- The epigrafts were made from ma- sual acuity results for the eyes be- Hirsh Ami, MD chined corneal tissue that was found fore PRK and at 3 months, 1 year, Solberg Yoram, MD, PhD unsuitable for penetrating kerato- and 21⁄2 years after PRK. No haze has Cahana Michael, MD plasty. -

Analysis of Human Corneal Igg by Isoelectric Focusing
Investigative Ophthalmology & Visual Science, Vol. 29, No. 10, October 1988 Copyright © Association for Research in Vision and Ophthalmology Analysis of Human Corneal IgG by Isoelectric Focusing J. Clifford Woldrep,* Robin L. Noe,f and R. Doyle Stulringf Parameters which regulate the localization and retention of IgG within the corneal stroma are complex and poorly understood. Although multiple factors are involved, electrostatic interactions between IgG and anionic corneal tissue components, ie, proteoglycans (PG) and glycosaminoglycans (GAG) may regulate the distribution of antibodies within the corneal stroma. Isoelectric focusing (IEF) and blotting analysis of IgG revealed a restricted pi profile for both central and peripheral regions of the normal cornea. Similar analysis of pathological corneas from keratoplasty specimens in Fuchs' dys- trophy and keratoconus reveal a variable IEF profile. In the majority of keratoplasty specimens from patients with corneal edema or graft rejection, there was generally little or no IgG detectable. These results suggest that in edematous corneas where there is altered PG/GAG in the stroma and modified fluid dynamics, there is a concomitant loss of IgG. These findings may have implications for immuno- logic surveillance and protection of the avascular cornea. Invest Ophthalmol Vis Sci 29:1538-1543, 1988 The humoral immune system plays an important the soluble plasma proteins through ionic interac- role in mediating immunologic surveillance and pro- tions. The PGs and GAGs have long been known to -
Management Modalities for Keratoconus an Overview of Noninterventional and Interventional Treatments
REFRACTIVE SURGERY FEATURE STORY EXCLUSIVE ONLINE CONTENT AVAILABLE Management Modalities for Keratoconus An overview of noninterventional and interventional treatments. BY MAZEN M. SINJAB, MD, PHD anagement of keratoconus has advanced TAKE-HOME MESSAGE during the past few years, and surgeons can • When evaluating patients with keratoconus, ask now choose among numerous traditional and them to stop using RGP contact lenses at least 2 modern treatments. Traditional modalities weeks before evaluation to achieve correct Msuch as spectacle correction, contact lenses, penetrating measurement of the corneal shape. keratoplasty (PKP), and conductive keratoplasty (CK) • Interventional management modalities include CK, are still effective; however, demand for the last two has PKP, DALK, ICRSs, CXL, phakic IOLs, or some decreased with the advent of modern alternatives, specifi- combination of these treatments. cally intrastromal corneal ring segments (ICRSs) and cor- • Making the right management decision depends neal collagen crosslinking (CXL). Caution should be used on the patient’s corneal transparency and stress when considering these newer treatment modalities, and lines, age, progression, contact lens tolerance, surgeons should be aware of their indications, contraindi- refractive error, UCVA and BCVA, K-max, corneal cations, conditions, and complications before proceeding thickness, and sex. with treatment. Keratoconus treatments can be divided into two cate- Some patients achieve good vision correction and comfort gories, interventional and noninterventional. In this article, with this strategy. particular attention is given to ICRSs and CXL, as they are Advances in lens designs and materials have increased the the most popular emerging interventional management proportion of keratoconus patients who can be fitted with modalities for keratoconus. -

Acute Keratoconus-Like Corneal Hydrops Secondary to Ocular
perim Ex en l & ta a l ic O p in l h Journal of Clinical & Experimental t C h f a o l m l a o Ke et al., J Clin Exp Ophthalmol 2017, 8:6 n l o r g u y o Ophthalmology J DOI: 10.4172/2155-9570.1000694 ISSN: 2155-9570 Case Report Open Access Acute Keratoconus-Like Corneal Hydrops Secondary to Ocular Massage Following Trabeculectomy Hongmin Ke, Chengguo Zuo and Mingkai Lin* State Key Laboratory of Ophthalmology, Zhongshan Ophthalmic Center, Sun Yat-sen University, 54 Xianlie Nan Road, Guangzhou, China *Corresponding author: Mingkai Lin, State Key Laboratory of Ophthalmology, Zhongshan Ophthalmic Center, 54 Xianlie Nan Road, Guangzhou, China, 510060, E- mail: [email protected] Received date: November 13, 2017; Accepted date: November 21, 2017; Published date: November 23, 2017 Copyright: © 2017 Ke H, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited. Abstract Purpose: To report a case of acute keratoconus-like corneal hydrops in a patient with long-term ocular massage following trabeculectomy. Methods: Case report and review of medical literature. Results: A rare complication of acute keratoconus-like corneal hydrops occurred in a patient following the use of ocular massage to maintain satisfactory aqueous humor filtration after trabeculectomy. The patient had a history of high myopia but denied previous ocular trauma, allergic disease and a family history of keratoconus. Slit-lamp examination demonstrated keratoconus-like corneal hydrops with formation of epithelial microcystic, and intrastromal cleft. -

Scleral Lenses and Eye Health
Scleral Lenses and Eye Health Anatomy and Function of the Human Eye How Scleral Lenses Interact with the Ocular Surface Just as the skin protects the human body, the ocular surface protects the human Scleral lenses are large-diameter lenses designed to vault the cornea and rest on the conjunctival tissue sitting on eye. The ocular surface is made up of the cornea, the conjunctiva, the tear film, top of the sclera. The space between the back surface of the lens and the cornea acts as a fluid reservoir. Scleral and the glands that produce tears, oils, and mucus in the tear film. lenses can range in size from 13mm to 19mm, although larger diameter lenses may be designed for patients with more severe eye conditions. Due to their size, scleral lenses consist SCLERA: The sclera is the white outer wall of the eye. It is SCLERAL LENS made of collagen fibers that are arranged for strength rather of at least two zones: than transmission of light. OPTIC ZONE The optic zone vaults over the cornea CORNEA: The cornea is the front center portion of the outer Cross section of FLUID RESERVOIR wall of the eye. It is made of collagen fibers that are arranged in the eye shows The haptic zone rests on the conjunctiva such a way so that the cornea is clear. The cornea bends light the cornea, overlying the sclera as it enters the eye so that the light is focused on the retina. conjunctiva, and sclera as CORNEA The cornea has a protective surface layer called the epithelium. -

Association Between Visual Field Damage and Corneal Structural
www.nature.com/scientificreports OPEN Association between visual feld damage and corneal structural parameters Alexandru Lavric1*, Valentin Popa1, Hidenori Takahashi2, Rossen M. Hazarbassanov3 & Siamak Yousef4,5 The main goal of this study is to identify the association between corneal shape, elevation, and thickness parameters and visual feld damage using machine learning. A total of 676 eyes from 568 patients from the Jichi Medical University in Japan were included in this study. Corneal topography, pachymetry, and elevation images were obtained using anterior segment optical coherence tomography (OCT) and visual feld tests were collected using standard automated perimetry with 24-2 Swedish Interactive Threshold Algorithm. The association between corneal structural parameters and visual feld damage was investigated using machine learning and evaluated through tenfold cross-validation of the area under the receiver operating characteristic curves (AUC). The average mean deviation was − 8.0 dB and the average central corneal thickness (CCT) was 513.1 µm. Using ensemble machine learning bagged trees classifers, we detected visual feld abnormality from corneal parameters with an AUC of 0.83. Using a tree-based machine learning classifer, we detected four visual feld severity levels from corneal parameters with an AUC of 0.74. Although CCT and corneal hysteresis have long been accepted as predictors of glaucoma development and future visual feld loss, corneal shape and elevation parameters may also predict glaucoma-induced visual functional loss. While intraocular pressure (IOP), age, disc hemorrhage, and optic cup characteristics have been long identifed as classic risk factors for development of primary open-angle glaucoma (POAG)1,2, the Ocular Hypertension Treatment Study (OHTS) suggested central corneal thickness (CCT) as a new risk factor for development of POAG3. -

Eleventh Edition
SUPPLEMENT TO April 15, 2009 A JOBSON PUBLICATION www.revoptom.com Eleventh Edition Joseph W. Sowka, O.D., FAAO, Dipl. Andrew S. Gurwood, O.D., FAAO, Dipl. Alan G. Kabat, O.D., FAAO Supported by an unrestricted grant from Alcon, Inc. 001_ro0409_handbook 4/2/09 9:42 AM Page 4 TABLE OF CONTENTS Eyelids & Adnexa Conjunctiva & Sclera Cornea Uvea & Glaucoma Viitreous & Retiina Neuro-Ophthalmic Disease Oculosystemic Disease EYELIDS & ADNEXA VITREOUS & RETINA Blow-Out Fracture................................................ 6 Asteroid Hyalosis ................................................33 Acquired Ptosis ................................................... 7 Retinal Arterial Macroaneurysm............................34 Acquired Entropion ............................................. 9 Retinal Emboli.....................................................36 Verruca & Papilloma............................................11 Hypertensive Retinopathy.....................................37 Idiopathic Juxtafoveal Retinal Telangiectasia...........39 CONJUNCTIVA & SCLERA Ocular Ischemic Syndrome...................................40 Scleral Melt ........................................................13 Retinal Artery Occlusion ......................................42 Giant Papillary Conjunctivitis................................14 Conjunctival Lymphoma .......................................15 NEURO-OPHTHALMIC DISEASE Blue Sclera .........................................................17 Dorsal Midbrain Syndrome ..................................45 -

Treatment of Stable Keratoconus by Cataract Surgery with Toric IOL Implantation
10.5005/jp-journals-10025-1024 JaimeCASE Levy REPORT et al Treatment of Stable Keratoconus by Cataract Surgery with Toric IOL Implantation Jaime Levy, Anry Pitchkhadze, Tova Lifshitz ABSTRACT implantation in the right eye. On presentation, uncorrected We present the case of a 73-year-old patient who underwent visual acuity (UCVA) was 6/60 OU. Refraction was –0.75 successful phacoemulsification and toric intraocular lens (IOL) –5.0 × 65° OD and –3.25 –4.0 × 98° OS. Nuclear sclerosis implantation to correct high stable astigmatism due to and posterior subcapsular cataract +2 was observed in the keratoconus and cataract. Preoperative refraction was –3.25 – left eye. The posterior segments were unremarkable. 4.0 × 98°. A toric IOL (Acrysof SN60T6) with a spherical power of 16.5 D and a cylinder power of 3.75 D at the IOL plane and Corneal topography performed with Orbscan (Bausch 2.57 D at the corneal plane was implanted and aligned at an and Lomb, Rochester, NY) showed central thinning of 457 axis of 0°. Uncorrected visual acuity improved from 6/60 to microns and positive islands of elevation typical for 6/10. Postoperative best corrected visual acuity was 6/6, 6 months after the operation. In conclusion, phacoemulsification keratoconus in the right eye (Fig. 1). In the left eye a less with toric IOL implantation can be performed in eyes with pronounced inferior cone was observed (Fig. 2), without keratoconus and cataract. any area of significant thinning near the limbus typical for Keywords: Intraocular lens, Toric IOL, Keratoconus, Cataract pellucid marginal degeneration.2 Keratometry (K)-values surgery. -

Endogenous Endophthalmitis: Diagnosis and Treatment
UVEITIS OPHTHALMIC PEARLS Endogenous Endophthalmitis: Diagnosis and Treatment ndogenous endophthalmitis Pathogenesis 1 (EE) is an uncommon intraoc- The infectious agent travels via the Eular infection with potentially bloodstream and multiplies in the cho- devastating visual consequences. An roid, eventually infiltrating the retina endogenous source is responsible for and spreading into the vitreous.4 roughly 2% to 8% of all endophthal- A diagnosis of EE merits a systemic mitis.1 Prompt diagnosis and treatment workup for the source of infection, are essential to obtain the best visual although in 44% of cases no source is outcomes. The underlying infection found.2 EE has been most commonly should also be investigated and man- associated with liver abscesses, sinus aged, although it remains unidentified infections, endocarditis, meningitis, or in many cases. presence of indwelling catheters. Etiology Diagnosis About half of reported EE cases are Presentation. Patient presentation YEAST INFECTION. Fundus photo of caused by bacteria and half by fungi.2 ranges from asymptomatic to symp- a white, fluffy chorioretinal infiltrate In North America and Europe, the toms typical of severe uveitis, including erupting into the vitreous. Vitreous fluid most frequently identified causative a red, painful eye with photophobia, grew Candida albicans. bacteria are Staphylococcus aureus and floaters, or reduced vision. Although EE Streptococcus pneumoniae, while in East is most often unilateral, up to a third of conditions, infectious and noninfec- Asia, Klebsiella pneumoniae is chiefly cases have bilateral involvement.5 tious, should be considered in formu- responsible.1 Among fungal etiologies, Ocular examination. Symptomat- lating the diagnosis. See “Differential Candida albicans (Fig. 1) is the most ic patients may have reduced visual Diagnosis” on the next page. -

Shift Work: a Risk Factor for Central Serous Chorioretinopathy
Shift Work: A Risk Factor for Central Serous Chorioretinopathy ELODIE BOUSQUET, MYRIAM DHUNDASS, MATHIEU LEHMANN, PIERRE-RAPHAE¨L ROTHSCHILD, VIRGINIE BAYON, DAMIEN LEGER, CIARA BERGIN, ALI DIRANI, TALAL BEYDOUN, AND FRANCINE BEHAR-COHEN PURPOSE: To investigate if shift work or sleep distur- and focal serous detachments of the neurosensory retina bances are risk factors for central serous chorioretinop- and retinal pigment epithelium alterations. The role of athy (CSCR). choroid hyperpermeability in the pathogenesis of CSCR DESIGN: Prospective case-control study. has been well documented recently with multimodal imag- 2 METHODS: Forty patients with active CSCR and 40 ing modalities. In CSCR patients, a thick choroid has controls (age- and sex-matched) were prospectively been reported not only in the affected eye but also in the recruited from the Ophthalmology Department of Hoˆtel fellow eye, which is consistent with bilateral choroidal Dieu Hospital, Paris, between November 2013 and hyperpermeability.2,3 December 2014. All patients were asked to complete a To date, several risk factors for CSCR have been questionnaire addressing previously described risk factors identified,3 and the most consistent is corticosteroid and working hours, as well as the Insomnia Severity exposure from therapeutic administration or from endog- Index (ISI), a validated instrument for assessing sleep enous overproduction, as in Cushing syndrome.4–6 disturbances. Corticosteroids were recently shown to induce RESULTS: The mean age of the CSCR group was 44